Chalkboard Template - University of Florida
advertisement

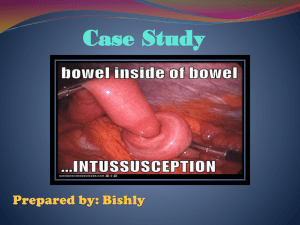
ACUTE SURGICAL CONDITIONS New Resident Orientation Michael Hong, MD June 25, 2013 University of Florida, Department of Surgery Pancreaticobiliary Service • • • Cholecystitis Cholangitis Pancreatitis Cholecystitis • • • Low grade fever, RUQ pain, nausea, vomiting Mild leukocytosis: 10-12 Key points • • RUQ US best test – stones, pericholecystic fluid, gallbladder wall thickening, CBD diameter Rule out complicating features: diabetes, peritonitis, high leukocytosis, high-grade fever, jaundice/hyperbilirubinemia. • Could indicate gangrenous cholecystitis, perforated cholecystitis, choledocholithiasis, cholangitis, pancreatitis. Cholangitis • • • • • Fever and leukocytosis can depend on early versus late stage of cholangitis. Rapid progression to sepsis. Hyperbilirubinemia, dilated common bile duct Imaging: only indicated if diagnosis is not certain. No role for MRCP in clear-cut cholangitis. Treatment: emergent ERCP for stone extraction and sphincterotomy. Pancreatitis • • • • • Acute onset epigastric pain radiating to the back Elevated amylase and lipase Possibly elevated transaminase and alk phos from impacted gallstone Common causes: alcohol, gallstone, metabolic, malignancy, drugs, medicine stuff, pancreatic divisum, hypertriglyceridemia. Treatment depends on the underlying cause, supportive care, no role for prophylactic antibiotics Acute Care Surgery • • • • • Appendicitis Cholecystitis Small bowel obstruction Incarcerated hernia Perforated gastric ulcer Appendicitis • • • • • • History and physical are the most important Acute onset peri-umbilical pain migrating to the right lower quadrant. Nausea and vomiting, subjective fevers, chills. Pain at McBurney’s point, peritonitis. Signs: Rovsing, Psoas, Obdurator Imaging: CT with IV contrast is first line, ultrasound and children and pregnant women, MRI • • • CT: enlarged appendix greater than 6 mm, contrast enhancement of the appendiceal wall, non-filling of appendix lumen with oral contrast, periappendiceal fat stranding. Management: IV fluids, IV antibiotics (Unasyn or Cipro/Flagyl in adults, Ceftriaxone in pediatrics), laparoscopic appendectomy in most cases Additional points: high fever or high leukocytosis often correlates with perforation. CT of appendicitis Small Bowel Obstruction • • History of nausea, vomiting, abdominal distention, abdominal pain, and no bowel movements for several days. Work up includes CT scan with oral contrast • • Most common cause are adhesions and hernias. • • • Look for contrast filling, proximal dilatation, distal decompression, “transition point” History must include documentation of prior abdominal or pelvic surgeries. Must rule out incarcerated hernias, volvulus. Treatment for small bowel obstruction caused by adhesions is initial conservative management with NPO, NG tube, IV fluids. Dilated promixal / Decompressed Distal Incarcerated Hernias • • Reducible, incarcerated, strangulated. Inguinal, umbilical, femoral, obturator, ventral. • • • • CT scan is helpful Do not reduce a hernia in someone who is toxic Maneuvers to increase successful reduction • • Femoral and operator hernias are difficult to diagnose on physical exam. Supine position, legs bent, deep constant pressure, Trendelenburg position, oral sedation Acutely irreducible hernia is an indication for surgery. Inguinal hernia imaging Perforated Gastric Ulcer • • • • • Acute onset abdominal pain Peritonitis, rigid abdomen Free air under the diaphragm on chest x-ray or KUB History of using aspirin, NSAIDs, Goody powder Treatment: urgent laparoscopy or laparotomy. Air under the diaphragm Treatment of Gastric Ulcer Pediatric Surgery • • • • • • Appendicitis Gastroschisis / Omphalocele Malrotation / mid-gut volvulus Intussusception Pyloric Stenosis Necrotizing Enterocolitis Gastroschisis / Omphalocele • Gastroschisis • • • • Defect of umbilical membrane near vein No coverage, to right of umbilicus Need immediate coverage Omphalocele • • Incomplete closure of abdominal wall Associated with other abnormalities (VACTERL) • • • Babygram (vertebral) Echocardiogram Usually covered by sac, sometimes ruptured Gastroschisis Omphalocele Midgut Volvulus • • • • Secondary to intestinal malrotation Bilious emesis Xray: gastric/duodenal distension UGI: oral contrast film – corkscrew appearance in duodenum, extrinsic compression by Ladd’s bands • • Small bowel on right, colon on left Duplex US: SMV is normally to right of SMA, flipped in volvulus Ladd Procedure Intussusception • • • • • Age 6 months to 2 years Hypertrophied Peyer’s patches Colicky abdominal pain, currant jelly stool Tx: air enema by radiology Operative reduction if enema unsuccessful Intussusception Pyloric Stenosis • • • • • • • • Risk factors: first born white male, erythromycin use in pregnancy Age: 2-6 weeks History: nonbilious projective vomiting shortly after feeds Physical: palpable “olive” epigastric area Labs: hypochloremic hypokalemic metabolic alkalosis Imaging: abdominal ultrasound Tx: resuscitation, correct electrolytes Operation only after medical stabilization Necrotizing Enterocolitis • • • • Abdominal distension, intolerance to feeds, bilious emesis, bloody stools soon after enteral intake in premature infant Abdominal erythema, crepitus, or discoloration is ominous Tx: NPO, IV abx, NGT, resuscitation Operation for pneumoperitoneum • Also for portal venous air, abd erythema, clinical deteriorization Pneumatosis intestinalis Vascular and TCV Surgery • • • • Acute limb ischemia DVT/PE Ruptured AAA Acute dissection Acute Limb Ischemia • • • • 6 Ps: pain, pulselessness, paralysis, pallor, paresthesia, poikilothermia Obtain history about timing, irregular heart rhythm, chest pain suggestive of heart attack, history of aneurysms. Document good pulse exam Treatment: immediate anticoagulation with therapeutic dose heparin • • Embolectomy Fasciotomy • Mild muscle weakness and sensory loss, inaudible arterial signal with intact venous signal DVT • • • • History and physical: unilateral, though leg pain increasing with movement. Unilateral leg swelling Homan’s sign is not useful Wells criteria Diagnosis: venous duplex ultrasound • • D-dimer is usually elevated postoperatively Treatment systemic anti-coagulation with therapeutic dose of heparin or Lovenox Pulmonary Embolism • • • • • • • • Tachypnea, tachycardia, pleuritic chest pain Assess for DVT CXR and EKG nonspecific (rule out other stuff) ABG: decreased CO2 (tachypnea) PE protocol CT is expensive, requires heavy dye load, and is not appropriate for low suspicion V/Q scan, like all nuc med studies, are of limited value Same tx as DVT Supplemental O2 Ruptured AAA • • • • • • Signs of shock Pulsatile abdominal mass Most common presentation is transfer from OSH with CT scan showing AAA rupture Call fellow immediately If stable, obtain CT scan for possible endovascular repair planning if not already done OR Ruptured AAA Aortic Dissection • • • • Sudden onset tearing, ripping, 10/10 chest pain radiating to back Vitals: hypertension Work up: CT, Echo Determine location: • • Stanford A/B: A = asc, B = arch + desc DeBakey I, II, III • • • • I asc + desc II asc + arch III desc distal to L SCA Treatment: beta blockers and BP control for Type B • OR for type A Aortic dissection Aortic Dissection Colorectal Surgery • Diverticulitis Diverticulitis • • LLQ pain, hx of diverticulosis Diagnosis by CT scan • • Uncomplicated – bowel thickening, localized tenderness Complicated – Hinchey Classification • • • • • Hinchey I: pericolic abscess Hinchey II: larger mesenteric abscess, extension to pelvis Hinchey III: free perforation, purulent peritonitis Hinchey IV: feculent peritonitis Treatment: • • uncomplicated clear liquids, oral abx complicated • • • Hinchey I/II: NPO, IV abx, percutaneous drainage for abscess >5cm Hinchey III: resection and primary anastomosis vs colostomy Hinchey IV: diverting colostomy Diverticulitis Burn Surgery • • Burns Necrotizing soft tissue infection Burn • • Mechanism Rule out inhalational injury • • • • • • History: enclosed space, smoke Physical: soot in mouth, singed facial hairs, hoarseness Labs: methemoglobin on ABG Bronchoscopy Resuscitate – Parkland Formula, LR Evaluate pulses for need for escharotomy / fasciotomy Necrotizing soft tissue infection • • Risk factors: Diabetes, Immunosuppression Exam: tachycardia / tachypnea / altered mental status • • • • Labs: LRINEC score Imaging: CT for gas in soft tissue / fascia • • Tenderness / pain away from erythematous area Crepitus, paralysis, bullae MRI too sensitive, difficult to obtain quickly Treatment: wide debridement and IV Abx NSTI VA General Surgery • Anything goes!