PPT - Cochin GUT Club
advertisement
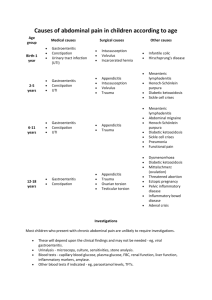
A case of abdominal pain and vomiting Dr charles panackel Demography 14 year old boy Presenting complaints Abdominal pain since early childhood Vomiting of 2 months duration History of presenting complaints Complaints started as recurrent attacks of abdominal pain since early child hood. Severe Colicky pain, lasting for 15- 20 mts. Periumblical in location. No radiation of pain. Pain aggravated by food intake. Relieved by injections and medications from local hospital. Patient used to have 2-3 episodes per year. Each episode used to last for 1-2 weeks and relieved with treatment from local hospital. Evaluated with x-rays and USG abdomen and no definite diagnosis made. History of presenting complaints Presently patient has abdominal pain for last 2 months. Colicky pain lasting for 15-20mts. Periumblical in location. No radiation. Pain was aggravated by food intake There was no associated fever, jaundice. No dysuria, hematuria. No Steatorrhea History of presenting complaints Associated bilious vomiting and pain was relieved by vomiting 2-3 episodes per day. Occurs ½-1 hour after food intake. There was no delayed or stale food vomiting. Patient had associated ball rolling sensation. There was no abdominal distension or borborygmi. There was no associated constipation. There was no hematemesis, melena or hematochizia. There was no associated postural symptoms or oliguria. No autonomic symptoms like excessive sweating, postural syncope or palpitation No purpura, urticaria, vesicular / bullous eruptions, No arthritis/oral ulcers No history of pica. Was admitted and evaluated in local hospital treated symptomaticaly with no relief of pain or vomiting and referred here. Past history Second borne of a nonconsanguinous marriage. Normal developmental mile stones and scholastic performance. No history of steatorrhea, respiratory symptoms, jaundice. No history of tuberculosis No history of any anorectal, renal or cardiac anomalies. No history of surgery Family history No family history of Similar abdominal pain No history of pancreatitis, skin lesions, psychosis, tuberculosis Was on treatment from local hospital for abdominal pain. DD 14 year old boy with recurrent periumblical colicky abdominal pain from early childhood now presenting with sudden aggravation of pain and bilious vomiting of 2 months duration. Differential diagnosis Malrotation with mid gut volvulus Congenital band Meckels diverticulum with mid gut volvulus Annular pancreas Intussuception Recurrent pancreatitis Congenital biliary defects Examination No dehydration PR-78/’ BP- 110/70 no postural fall RR -16/’ Moderately built and poorly nourished for the age Ht 142 cm Wt 32 kg BMI 15.8 No pallor /No jaundice / edema / lymphadenopathy No stigmata of malabsorption like phrynoderma, bitots spots, glossitis, cheilitis, bone tenderness No perioral or pigmentation, no skin lesions like purpura, vesicles, ulcers, No skeletal anomalies, ptosis, ophtalmoplegia No skin or joint laxity No anorectal or external genitalia abnormalities Oral cavity- Normal. No perioral pigmentation Abdomen – Not distended/ No visible peristalsis/ dilated veins /swelling/ abdominal wall defects Liver was palpable 3cm below the right costal margin. Span 12cm. Soft, nontender, rounded margins and smooth surface Spleen was not palpable No mass palpable Normal bowel sounds P/R – Normal Hernial orifices normal Chest - Normal CVS; S1 and S2 normal.No murmur CNS –No ptosis, ophthalmoplegia, myopathy or neuropathy Fundus; normal Differential diagnosis Malrotation with recurrent gut volvulus Congenital ladds band Meckels diverticulum with mid gut volvulus Annular pancreas Intussuception Investigations Hb 11.8 TC 6700 DC P68 L30 E2 ESR 22 RBS 82 S.Na 142 S.K 3.7 S.Ca 8.2 BU/Cr- 15/0.7 Bb 0.7 SGOT /PT 32/23 ALP 72 TP 6.8 Alb 3.2 USG Dilated stomach with stasis no other abnormality noted OGD Esophagus was normal. Stomach, D1 and D2 were dilated with stasis. Scope was not introduced beyond D2. CT – Suggestive of intestinal malrotation with midgut vovulus Surgery Duodenum dilated upto D3 Band from transverse colon to D3/D4 jn---released the band Volvulus 1/4th rotation – No strangulation -Untwisted the bowel Small bowel put on the right side Large bowel put on the left side Inversion appendicectomy done Final diagnosis Intestinal Malrotation Partial intestinal obstruction at D3 level with Ladds bands and Midgut Volvulus Malrotation of midgut Occurs in 1/1600 live births Normally midgut goes out of the abdominal cavity during 4 th week of gestation Comes back inside by the 10 th week Midgut rotates around the axis of SMA for an angle of 270degrees Initial 90 degree rotation takes place outside the abdominal cavity Second stage inside the abdomen – rotates through 180 degrees Third stage is the descend of cecum Anomalies Non rotation (most common) Malrotation Reverse rotation Symptoms Most patients have symptoms within the first month Recurrent vomiting Abdominal pain Malabsorption Chylous ascites Asymptomatic Associations 30 to 60% Omphalocoele Gastroschisis Diaphragmatic hernia Duodenal or jejunal atresia Hirshsprung’s disease Esophageal atresia Biliary atresia Annular pancreas Meckel’s diverticulam Mesenteric cysts Congenital cardiac defects Imaging modality Plain radiograph Upper GI contrast study Barium enema Ultrasonography Findings suggestive of malrotation Nasogastric or orogastric tube that extends into an abnormally positioned duodenum The "double-bubble"sign of duodenal obstruction A clearly misplaced duodenum (ie, ligament of Treitz on the right side of the abdomen) that has a "corkscrew" appearance Duodenal obstruction, which may appear similar to that seen with duodenal atresia or may have more of a "beak" appearance if a volvulus is present Complete obstruction of the transverse colon, particularly if the head of the barium column has a beaked appearance Abnormal position of the superior mesenteric vein (either anterior or to the left of the superior mesenteric artery) Dilated duodenum (indicating duodenal obstruction) The "whirlpool" sign of volvulus (caused as the vessels twist around the base of the mesenteric pedicle) Treatment Surgery Thank you