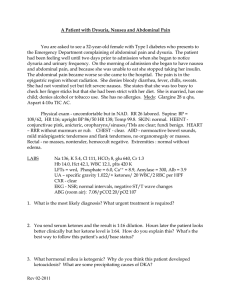
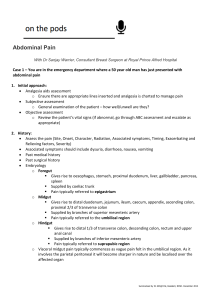
Abdominal Pain
advertisement
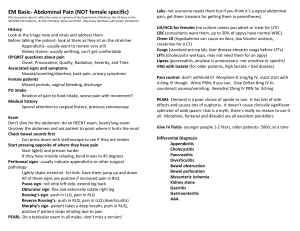
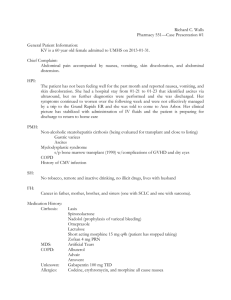
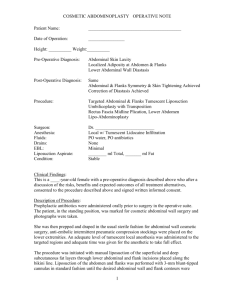
Abdominal Pain Case 1 A 19 year old male presents with a two day history of abdominal pain. He states that at onset, his pain was in the middle of his abdomen, and has since moved to the right lower side. He notes nausea, emesis, anorexia, and a low grade fever. On exam, he has rebound tenderness to the RLQ, pain with leg movement, hip rotation, and pain in the RLQ on LLQ palpation. How often do perfect clinical cases like this present to the ED? Introduction 6.7% of ED visits are for abdominal pain History, physical, labs often not as helpful as Cope would have you believe. Goal is to detect life-threatening causes of abdominal pain, if not to make a solid diagnosis. The Elderly, the Young, and those who cannot get follow-up are high risk groups that may require further study and admission even in the absence of abnormal findings. Pain Visceral ◦ Stretching of unmyelinated fibers that innervate walls or capsules of organs. ◦ Crampy, dull, achey pain. ◦ Localized to a sensory level, but often midline Parietal ◦ Irritaion of myelinated fibers in the parietal peritoneum ◦ Localizable, causing guarding, rebound ◦ Patients like to stay still Pain Referred pain ◦ ◦ ◦ ◦ ◦ ◦ Pain that is remote from the source Caused by developmental embryology Normally ipsilateral Boaz Sign? Kehr’s Sign? Where might renal pain get referred to? Priorites Finding critical illness and stabilizing ◦ Normal vitals signs are not excluding for critical illness ◦ Resuscitate and diagnose at the same time 2 LB IV’s, O2, monitor CBC, BMP, Coag, T&S ◦ Don’t neglect to do a thorough exam. ◦ Intensity of pain bears no relation to severity of illness. Priorities Finding critical illness ◦ Red Flags Extremes of age Rapid onset of severe pain Abnormal vitals Dehydration Pallor, vomiting, diaphoresis ◦ Shock most likely hemorrhagic if of rapid onset ◦ Temperature least helpful of vitals History OPQRST ◦ ◦ ◦ ◦ ◦ ◦ Onset Provocations/palliations Quality Radiation Severity Timing What has been done Last oral intake History Pertinent illnesses ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ DM HTN, CAD, PVD Liver or Renal disease Surgical history Sexual history Meds/IUDs Any trauma Any similar episodes? Physical Exam Uncover as much as necessary ◦ Check for that perirectal abscess and Fournier’s First, inspect ◦ Distended, stigmata of liver disease, surgical scars? Masses? Then, auscultate ◦ Low sensitivity! Physical exam Finally palpate ◦ Have the patient point to where it hurts ◦ Hit that area last ◦ May have patient bend knees if they cannot otherwise relax abdominal wall muscles ◦ Interrater reliability 60-92% for abdominal tenderness (Yen, K, et al, Arch Ped Adol Med, 2005, Apr, 159(4):373-6) ◦ Consider early use of Ultrasound at the time of palpation. Labs Should be diagnosis specific Consider pattern of pain How likely is it that an LFT will help someone with LLQ pain? Preg test – always necessary for women of childbearing age and capability Labs CBC ◦ WBC least useful in the panel ◦ Hemoglobin – anemia from what? Can be useful for trending ◦ Platelet counts – liver disease, ITP, HEELP BMP ◦ Renal function most important ◦ Calcium ◦ CO2 level as a flag for metabolic acidosis Imaging Ultrasound ◦ Many choose to use ultrasound like a stethoscope ◦ Modality of choice for RUQ pain ◦ Recommended as first line for flank pain, RLQ pain in kids – operator dependent ◦ Modality of choice for pelvic pain Imaging Plain films ◦ Useful only for Free air Obstruction/volvulus Pneumonia ◦ Overall, low value Imaging CT ◦ ◦ ◦ ◦ High sensitivity High specificity High radiation risk High cost Elderly, immune compromised, those who you are uncertain, but look ill. PO contrast – bowel obstruction, bowel mass No contrast – renal stone, renal insufficiency Name that Story! Dull RUQ pain in a 16 year old male, worse with eating, associated with nausea and diarrhea? Name that Story! Low grade fever, LLQ tenderness, and rectal bleeding in a 55 year old male. Name that Story! Epigastric pain which is boring and cramping, which radiates to back, and is associated with eating cheese and alchohol. Amylase and lipase are normal. This is the 6th visit for this in a year. What level of bilirubin is needed to produce scleral icterus? Name that Story 55 year old diabetic with epigastric pain, weakness, nausea and vomiting. Some SOA, no diarrhea. Hx of HTN. Pain is off and on for the past week. Name that Story Post parandial pain in a 65 year old female who has nausea, emesis, appears to be in pain, but a benign abdominal exam, trace blood on rectal exam. Name that Story 65 year old male who presents with left flank pain that is gnawing, kept him up at night, and is not associated with syncope or hypotension. His last US showed a 3.5cm AAA. Name that Story 20 year old male sharp flank pain after backing into something. Has a 1 inch laceration to left flank. Vitals signs are stable. 30 minutes later, he is dead. Name that Story! 16 year old virgin presents with vaginal bleeding, RLQ abdominal pain and weakness. She is tachycardic, and her rosary-holding mother (who has been in the room) is concerned about fibroids. High Risk Groups Treatment TRUE OR FALSE? Pain should not be treated until a surgeon has laid hands on the patient? Treatment Fluids Symptom management NPO status until you know a surgeon won’t be needed anytime soon Antibiotics ◦ ◦ ◦ ◦ Gram negative for gut (flagyl, AG) E.coli for gut and urine (Cipro) Gram positives for SBP STD guidelines for PID Disposition Discharge ◦ ◦ ◦ ◦ ◦ Pain better Nasuea better Tolerates PO Negative eval, or no critical findings Adequate follow-up Otherwise admit Surgical consults as needed. Gastric Bypass High risk for leak ◦ Septic, abdominal pain, fever Dumping Syndrome ◦ Dietary changes ◦ Octreotide SQ drips for severe cases Internal hernia Immediate bowel obstruction may cause gastric rupture.