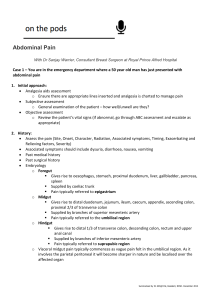
The Acute Abdomen - Airedale Gp Training
advertisement

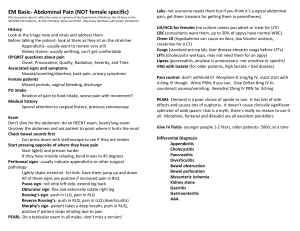
Ben Johnson Surgical Sieve Exercise • VITAMIN DC Presentation •History, examination & site of pain Causes •Medical •Gynaecological •Surgical Cases • 1-4 Summary & References ……………..Vascular ……………..Infective/inflammatory ……………..Traumatic ……………..Autoimmune ……………..Metabolic ……………..Iatrogenic ……………..Neoplastic ……………..Degenerative ……………..Congenital OHGP 3 Ed OHGP 3 Ed MI Lower lobe pneumonia PE Aortic dissection Acute hepatitis DKA UTI / pyelonephritis Herpes zoster IBS/IBD Gastroenteritis Hypercalcaemia Constipation Mesenteric adenitis Subphrenic abscess Addison’s Disease Porphyria Lead poisoning Spinal arthritis Muscular HSP Gastritis Diverticular disease Liver disease Iatrogenic Ectopic pregnancy PID Rupture/torsion of ovarian cyst Endometriosis Mittleschmertz Placental abruption, uterine rupture Dysmenorrhoea Gynae malignancy Non-specific abdominal pain Acute appendicits Cholecystitis and biliary colic Pancreatitis Peptic ulcer disease Abdominal aortic aneurysm Mesenteric ischaemia Diverticulitis Large bowel perforation Intestinal obstruction eg herniae, volvulus, adhesions Ureteric calculi Urinary retention Testicular torsion Intussusception / Meckel’s diverticulum Cancer Trauma/other causing rupture of abdominal viscera e.g. spleen Spinal artery occlusion Dylan is a 6 year old American boy who presents looking unwell with severe abdominal pain. He looks pale and is clutching his tummy. His parents say they have just arrived this morning from the US and shortly after landing Dylan woke up distressed and in pain. 1. Assessment Call for help, manage in resus, ABCDE. Low O2 sats, abdo pain , cool peripheries, looks dry 2. Management Oxygen, analgesia, keep the patient warm, iv access, blds for FBC, U&E, CRP, blood culture, VBG, ivf – fluid bolus 20ml/kg then maintenance fluids +/- %dehydration. Once stable CXR, MSU. FBC phoned through Hb 8.0, film pending……..possible diagnosis ? Sickle cell disease occurs in Africa, the Middle East, Caribbean, USA and Mediterranean populations Due to genetic defect in one of the Hb chains normal genotype produces HbA; heterozygote =sickle cell trait is HbAS in the homozygote HbS. The HbS molecule polymerizes in deoxygenated or acidic conditions causing RBC sickling. The sickle cells are fragile and haemolyse or block small vessels causing ischemia, infarction and further sickling. Can occur de novo or follow infection, cold, dehydration or any condition where tissue hypoxia or ischaemia occur The crisis may involve thrombosis, haemolysis or acute hepatosplenic sequestration. A crisis can mimic any acute medical/surgical emergency eg PE, stroke, acute abdomen, bone pain and low grade fever deoxygenation or acidosis sickling increased blood viscosity stasis sludging Kaycee-Leigh is an 8 year old who has presented with abdominal and leg pain. She is normally fit and well but has recently been treated for a throat infection by her GP. She is alert but grumpy and has a temperature of 38.2C. 1. Assessment Make a quick judgement as to whether you need help straight away. Observations. ABCDE. Is this a meningitic child ? E – exposure…rash on buttocks and both legs, nonblanching, some petechiae, some purpuric. 1. Assessment cont… Make a quick judgement as to whether you need help straight away. Observations. ABCDE. Is this a meningitic child ? E – exposure…rash on buttocks and both legs, nonblanching, some petechiae, some purpuric. She has no meningism but has vomited twice. Her abdomen is soft but she has voluntary guarding and is in discomfort when examined. Her parents tell you the abdominal pain comes and goes. Her ankles look oedematous and she has an antalgic gait. Her observations are P127, RR32, O2 99%A, T38.2C, Avpu, 2. Pertinent questions ….meningism. Foreign travel. Contact illnesses ….meleana / haematemesis ….recent infection ….haematuria 3. Management Providing you are sure this is not meningitis Analgesia +/- antipyretic Refer Paeds. Will need urinalysis FBC, U&E BP (hypertension is a sign of renal involvement) Combination of a characteristic skin rash, arthralgia, periarticular oedema, abdominal pain and glomerulonephritis. Usually occurs between 3-10yrs, 2♂:1♀, peaks during winter months, often preceded by URTI Cause unknown; postulated to involve genetic predisposition and antigen exposure increasing serum IgA. Complexes of IgA and IgG are deposited in the affected organs precipitating an inflammatory response with vasculitis. Rash in 50%, joint pain 66%, abdominal pain in many children (if severe Rx corticosteroids; can also get intussusception, ileus & protein losing enteropathy), renal involvement is common with >80% having proteinuria/haematuria. Renal involvement can progress over several years Malcolm is a 82 year old retired farmer. He presents with progressively worsening abdominal pain over the course of the day. He has had some vomits and looks uncomfortable. He is apyrexial, tachcardic at 120 and has a respiratory rate of 28. He says he has not opened his bowels for one week. His only medical history is a bladder ca. 3 years ago. He is awaiting a TURP. 1. Assessment GCS 15/15. P120. O2 95%A. BP 105/51. In pain – had 10mg morphine with YAS. Feels nauseated. Looks pale. Abdomen very tender, reluctant to move. What next…? 2. Management ?Resus ABCDE iv access x2 Monitoring Blds (FBC, U&E, LFT, Amylase, G&S, coag), VBG, iv fluids E-CXR, AXR ECG Urinary catheter Senior/Surgical review ………..?FAST scan / CT scan Results VBG : pH 7.26, PaO2 3.5, PaCO2 5.4, Hb 10.2, Glu 12.1, Na 133, K 3.3, HCO 19.1, BE -3.8 FBC : U&E, LFT : Hb 11.4, WCC 13.2, Plt 335 Na 130, K3.1, urea 7.8, creat 154 LFT normal except ALT 144, amylase 210 Coag : ECG : normal sinus tachycardia 120 ….Likely diagnosis ? Following resection of the bladder cancer this man had chemotherapy and radiotherapy The radiotherapy had caused fibrosis within the rectum requiring lifelong laxative treatment Another complication of radiotherapy to the abdomen can be damage to microvasculature of the mesentery. This in turn can lead to bowel ischaemia Due to his prostatic symptoms this man had become constipated because he drank less and omitted his laxative to manage his urinary frequency Tallula is a 30 year old lady who is 30/40 pregnant. She is G1 P0 and has until now had an uneventful pregnancy with some light spotting in the early stages. She has had normal scans at 10/40 and 19/40. The SFH record shows the baby is growing well. She has no PMH of note. She presents with a 6 hour history of generalised Abdominal pain, nausea and has vomited once. 1. Assessment GCS 15/15. P105. O2 100%A. T 37.5C. BP 112/78. Uncomfortable but mobilising ok. Nauseated but only one vomit. CVS & RS normal. Abdomen is not peritonitic but has generalised tenderness over her abdomen, more so on RUQ and Right loin. No PV discharge/bleeding. No headache or visual changes. Thoughts as to what is going on…….? 2. Management Analgesia……what ? Full observations including BP Blds, FBC, U&E, CRP, LFT, amylase, iv access Urinalysis…..(NB consider pre-eclampsia / UTI) Obstetric / surgical review ? 3. Differentials Onset of early labour Renal colic Cholestasis / gallstones Pancreatitis Appendicitis UTI / pyelonephritis Constipation Gastroenteritis Pre-eclampsia Results : Urinalysis : Leu +, Nit -ve, Ket –ve, Glu –ve, Pro -ve Blds : Hb 11.2, Plt 222, WCC 12.1, LFT and U&E normal, amylase 54, CRP 38 Most likely diagnosis……...? Most common surgical emergency UK lifetime incidence of ~6%. Peak age 10-30yrs Differentials include : mesenteric adenitis, UTI, IBD, gastroenteritis, Meckel’s, intussusception, Gynae/Obs, DKA/pneumonia etc Affects 1:1000 pregnancies. Maternal mortality is high and perforation more common (15-20%). Foetal mortality is 5-10% in simple appendicitis and 30% with perforation. Note the position of the appendix is different in pregnancy so signs may not be of classical RIF pain. Abdominal pain is a frequent PMC to the Emergency Department. As illustrated, the causes are many but common things are common. Most people will require analgesia, urinalysis +/-PT, FBC, U&E, LFT, CRP and amylase, BM +/- imaging. Non-specific abdominal pain accounts for a significant proportion of surgical admissions with most pain resolving spontaneously. Oxford Handbook of Emergency Medicine 3rd Edition Oxford Handbook of General Practice 3rd Edition Browse’s Introduction to the Symptoms and Signs of Surgical Disease 4th Edition Illustrated Textbook of Paediatrics 3rd Edition