Susceptibility of Corynebacterium
advertisement

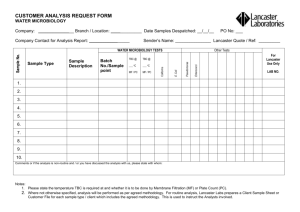
Practicals WT4 Mycobacterium, Corynebacterium • • • • • Laboratory diagonosis of mycobacteria + ATB susceptibility tests Laboratory diagnosis of. corynebacterium + ATB susceptibility test Lysogenic conversion Antituberculotics Microscopy - M.tbc - Ziehl Neelsen, C, diphtheria - Gram, Albert, C. pseudodiphthericum - Gram • Cultivation - M. tbc - Lowenstein and broth medium, C. diphtheriae a C. pseudodiphthericum - Blood agar and tellurit medium • Biochemical characteristics of C.diphtheriae a C. pseudodiphthericum • Toxigenicity of C. diphtheria - ELEK´s method and animal model Laboratory diagnosis of mycobacterium • Sampling - in pulmonar tbc - morning sputum -3 consecutive days, extrapulmonar - appropriate sample - big quantity of liquid urine, menstrual blood… • Microscopy - Ziehl Neelsen, fluorescence - increased sensitivity, preliminary dg • Cultivation -sample proceeding, decontamination of nonmycobacterial flora, condensation of the sample - NaOH, centrifugation. Eggs media - Šula, Lowenstein / solide and broth / - pigment, shape - in broth - membrane, sediment - Long generation time - quick methods - based on detection of metabolits of palmit acid and CO2 • Genetic probes - detection of aminoacids sequences Staining • Ziehl Neelsen - cover heat fixed and dried smear with a piece of filtrate papaer. Apply 5-7 drops of carbolfuchsine. Heat from beneath till vaporisation. Discard paper with forceps, rinse and dry. Decolorise with acid alcohol (HCl+ethanol) untill the color is stining the water. Conterstain with methylen blue. Rinse, dry. M. tbc - red, surroundings - light blue. • Albert - methylen blue or toluidin blue Lab. dg. of corynebacterium • Diagnosis of the disease is based on clinical picture and epidemiological history. Lab. dg. is long and complicated Appropriate sampling • Microscopy - smear with Gram staining and Albert´s staining does not distinguish between C. diphtheriae and other Corynebacteria. • Cultivation: Blood agar - 3 typs od colonies - mitis, gravis, intermedius, Loffler´s medium, tellurit medium brown colonies with halo • Biochemical identification- differentiation from other corynebacteria present in throat • toxigenicity of the strain - ELEK, • ATB susceptibility Antituberculotics and therapy • Streptomycin(kill actively multiplying M.tbc) Izoniazid,Rifampicin (effective on M.tbc in caseous necrosis) Ethanbutol Etionamid Kanamycin Cycloserin Pyrazinamid ( active i.c.) • In pacient with pulmonar tbc - 3 populations of M.tbc - localised extracelullarly in cavitas, intracelullarly in macrophages, inside caseouse necrosis • Combination of 2-3 ATT. Resistence fighting -overgrowinf of resistent mutants in culture of M.tbc - for INH 1:105 for STM 1:106 in infectious place there is 107- 10 9 of bacteria Lysogenic conversion • Strain of C. diphtheriae gains his toxigenicity by lysogenic conversion thanks to bacterophage. Bacterial virus bactrophage is able to transfere genetic information about the production of toxin tox gen - fom one cell ( toxigenic) to the other (non toxigenic) C. diphtheriae cell. Cultivation of Corynebacteria • C. diphtheriae - blood agar • C. pseudodiphthericum - blood agar, inverse CAMP • C. diphtheriae on tellurit medium - brown colonies with brouwn ring - halo Microscopy • Ziehl Neelsen staining - acid-fast M. tbc - not willin to accept stain. If colored - very difficult to decolorise • Gram staining of C. diphtheria - G+rods • Albert´s staining - metachromatic staininig of granules - resulting color is different from color used for staining - C. diphtheriae • Comparison of Gram smear of C. diphtheriae a C. pseudodiphthericum Cultivation of M. tbc • Egg medium - Lowenstein - colony morphology, no pigment • Broth medium - growing in membrane • cultivation 3-6 weaks - reading every weak Biochemical characteristics • Fermentation: differentiation of C. diphtheriae from other corynebacteria isolated from throat (C.ulcerans, C. pseudotuberculosis, C. xerosis, C. pseudodiphthericum • C. diphtheriae • granul catalase gelatine, urea, lactose, maltose, glc • + + + + • + + + • C. pseudodiphthericum Detection of toxigenicity of C. diphtheriae • ELEK´s test of toxigenicity - imunodiffusion of suspension of tested strain and antidiphtheric serum in agar - zone of precipitation • Annimal mode: application of diphtheria toxin i.d. ………………..necrosis • antidiphtheric serum (i.p. or i.d.) + toxin …no necrosis ATB susceptibility • Susceptibility test for antituberculotics - ATT are dissolved in medium • Method of proportional susceptibility testing - dilution method. Dilution of inoculum so that there is from 100-300 CFU - colony forming units on a plate • If there is more than 1% of M. tbc cells resistent to ATT the therapy will not be cliniccňally suscessful • Susceptibility of Corynebacterium - PNC, ERY - for elimination of bacteria or carriage state - therapy of diphtheria - primarily antitoxic. Preventive measures. • Nondiphtheriae corynebactria - Vancomycin, (Cefalosporins of the 1st generation) • Spontaneous appearance of resistent mycobacteria without exposition to ATT • Frequency of resistent cells in the culture is 1:105 for INH and 1:106 for STM - if both are given in combination the incidence of resistent strains will be 1:1011. • The overall population of bacilli in patient with open cavity is 10 7 - 109 , so there is 102 - 104 resistent strains. • 1 ATT means overgrowing of resistent strains that will replace susceptible killed bacteria. • Combination of 2 and more ATT: INH+RIF - 9 months, + STR+ Ethanbutol for 2-8 weaks, from 2nd months only 2 times weakly, INH + Ethanbutol 18-24 months, • Tests for ATT susceptibility - correlation between in vitro and therapy success. • If more than 1% of M. tbc in vitro are resistent - therapy will not be successful • Tests determine ratio between susceptible and resistent strains • Agar dilution method - depend on innoculum - if too thick - there is too much of resistent strains - false resistent, if less concentrated - false positive - possible resistent strains not identified. • Optimal dilution 100-300 CFU on plate • Inconvenience - aga can inhibit activity of ATT as well as of mycobacteria, long incubation decrease activity of ATT Principles of therapy • Therapy: ATT are active only on growing mycobacteria, growth depends on oxygen availability and pH (optimu neutral or alkaline) - Max in open cavity, min in caseouse necrose. • In i.c. - in phagosomes - pH is 5,5, acid - slow growth, less of bacilli, less resistent strains - ATT supporting acid environment - Pyrazinamide. (STM not able to enter phagosomes and looses activity in acid pH) • in chronic closed caseouse necrose - slow blood supply and oxygen, slow metabolism, less living cells, pH neutral but slow multiplication ATT • Bactericidal: STM - mycobacteria extracelullarly in cavities • INH - kills slowly and quickly growing cells • Rifampicin - effective on mycob. Closed in caseouse necrosis and macrophages • Pyrazinamide - only in acid pH and in macrophages • Bacteristatic: Ethanbutol - only in combination, able to penetrate in mycobacteria situated i.c. and e.c. • Capreomycin, Kanamycin - bactericidal, for e.c mycobacteria in cavities • Ethionamid, cycloserin - bacteriostatic for i.c and e.c