Chapter 10: Gram
advertisement

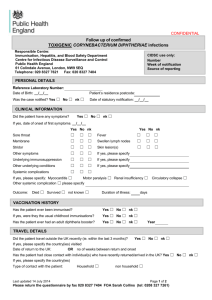
Chapter 10: Gram-Positive Rods 1. Corynebacterium (Coryneforms) – – Genus: Corynebacterium Species: Corynebacterium diphtheriae Corynebacterium xerosis Corynebacterium pseudodipheriticum Corynebacterium ulcerans – General Genus Characteristics • • • • • • • Gram (+) straight or slightly curved bacilli, frequently swollen one or both ends (club-shaped) Methylene Blue film metachromatic granules – polyphosphate storage granules (velutin) VERY resistant to drying Non-spore former Binary fission (cell division) – characteristic V and L shaped figures; “Chinese Letters” Non-motile and unencapsulated Most spp. are facultative anaerobes C.diphtheria Gram stain Methylene blue stain from Loefflers slant Arrangement of C. diphtheria كرينه باكتريوم محيطهاي كشت : تلوريت پتاسيم لفلر تينسدال CTAمحيط پايهٌ قندي • • • • • كرينه باكتريوم بيوتايپهاي كرينه باكتريوم ديفتريه در محيط تلوريت پتاسيم • از هم جدا مي شوند : بيوتايپ گراويس به شكل گل مينا و بزرگ • بيوتايپ مي تيس به اشكال مختلف(تخم مرغ نيمرو)و • متوسط بيوتايپ اينتر مديوس كوچكتر از بقيه و به شكل تخم • قورباغه Gram-Positive Rods 1. Corynebacterium (Coryneforms) – Growth Conditions • • Selective Media – blood tellurite reduction of tellurite gray/black colonies 3 biotypes of C. diphtheriae – Gravis: grave infection – Intermidius: intermediate infection – Mitis: little infection ***All 3 serotypes are capable of producing the same toxin & clinical disease. Gram-Positive Rods 1. Corynebacterium (Coryneforms) • Corynebacterium diphtheriae – – – Normal Flora – URT (throat and Nasopharynx) Reservoir – Human pathogen ONLY Infection 1. Respiratory (diphtheria) 2. Cutaneous (skin infection) – Transmission/Epidemiology – person-to-person (asymptomatic or diseased patients) 1. Inhalation of aerosols (i.e., respiratory droplets) 2. Direct contact w/ cutaneous lesions (analogous to impetigo) 3. Direct contact w/ contaminated fomites=( لوازم اشياءleast frequent) Gram-Positive Rods 1. • Corynebacterium (Corniforms) Corynebacterium diphtheriae – Virulence Factor • Diphtheria Toxin – very powerful exotoxin – Avirulent C. diphtheriae infected by bacteriophage (tox +) Lysogenic conversion to Virulent stain C. diphtheriae (tox +) Recall: Lysogeny – bacteriophage has ability to insert their DNA into DNA molecule of host bacterium. – Expression of tox gene • Regulated by Fe concentration – – – Tox gene repressor: Fe-containing protein Function of repressor – inhibits toxin production [Fe2+] decreased limited repressor available toxin gene Gram-Positive Rods 1. Corynebacterium (Corniforms) • Corynebacterium diphtheriae – Pathogensis • Diphtheria Toxin – 2 subunit fragments A & B – – B Fragment: Binds to specific cell surface receptors Mediates transport of A fragment into cell A Fragment: Inhibits protein synthesis => cell death/necrosis » Specifically, fragment A catalyzes a rxn. between NAD+ and the polypeptide chain elongation factor, EF-2: transfer of ADPR from NAD+ to EF-2 » Result = ADPR:EF-2 complex is INACTIVATED & protein (peptide) synthesis is terminated Gram-Positive Rods 1. Corynebacterium (Corniforms) • Corynebacterium diphtheriae – Clinical Disease 1. Localized infection Respiratory (Pharyngeal Diphtheria) Cutaneous Diphtheria (both toxigenic & non-toxigenic strains) 2. Systemic infection - toxemia Gram-Positive Rods 1. • Corynebacterium (Corniforms) Corynebacterium diphtheriae – Pharyngeal Diphtheria Mode of Infection 1. Inhalation 2. Attachment – to mucous membranes of passageways of oral cavity 3. Attachment/Colonization – non-specific virulence factors 4. Toxin production – necrosis of mucosal cells lesion expansion= توسعه بسط انبساط 5. Pseudomembrane formation – grayish-white patches= تكه وصله مشمع روي زخمof thick fibrous exudate (neutrophils, corynebacterium, epthelial cells) 6. Tight= سفت محكم مانع دخول هواadherence – to epithelial surface w/ no invasion of underlying tissue 7. Spread of pseudomembrane – involvement of nasopharyngeal tissues (mouth, pharynx) or larynx & trachea 8. Entry of toxin into the blood stream – multi-organ involvement: heart, CNS and kidneys; most frequent & serious damage d/t toxin occurs in the heart and CNS, w/ death resulting from damage to the heart. Gram-Positive Rods 1. • Corynebacterium (Corineforms) Corynebacterium diphtheriae – Pharyngeal Diphtheria: Summary • • Location infection of the throat (URT infection) Production of thick, grayish, adherent exudate • Pseudomembrane Composition = cell debris from mucosa & inflammatory products Coats the throat; may extend into nasal passages or downward into RT, obstructing the airways leading to suffocation w/ disease progression – generalized sx’s d/t production & absorption of toxin MAJOR CLINICAL EFFECTS: Heart & Peripheral Nerve involvement Cardiac conduction defects & myocarditis CHF & permanent heart damage. Neuritis of CN’s & paralysis of muscle grps – seen in late dis. Gram-Positive Rods 1. Corynebacterium (Corineforms) • Corynebacterium diphtheriae – Cutaneous Diphtheria • Localized infections arising from: insect bites, skin trauma, poor personal hygiene Ex. Puncture wound or cut in skin introduction of bacterium into subcutaneous tissue chronic, nonhealing ulcer w/ grayish membrane. • • Risk Group: homeless Sx’s: impetigo-like lesions Gram-Positive Rods 1. Corynebacterium (Corineforms) • Corynebacterium diphtheriae – Systemic Spread of Primary Infection 1. Heart – myocarditis 2. CNS – cranial & peripheral; nerve degeneration (paralysis) 3. Kidneys – filtering inadequacies; kidney failure – 1. 2. 3. 4. Risk Groups Individuals w/ low socioeconomic status Crowded & unsanitary conditions Non-immunized children (1-10 yoa) Elderly – low immunization status Gram-Positive Rods 1. • Corynebacterium (Corineforms) Corynebacterium diphtheriae – Diagnosis • • • Clinical: sx presentation (gray-membrane w/ swelling) Serological: Ab detection (to the toxin Ag.) Laboratory identification • Specimen – swab cultures ( pharynx, nasopharynx, or cutaneous sites) Microscopic appearance – smears alone are unreliable, possible presence of diphtheriods Cultivation – Media 1. Loeffler media Overnight growth film (Methylene Blue) metachromatic granules 2. Selective media (Tinsdale agar, containing tellurite) Blood tellurite corynebacterium reduce tellurite gray/black colored colonies w/ halos Tinsdale’s Agar contains Potassium tellurite, an inhibitor of other respiratory flora Gram-Positive Rods 1. • Corynebacterium (Corniforms) Corynebacterium diphtheriae – Treatment: 1. Respiratory Diphtheria • • 2. Cutaneous Diphtheria • – Passive Immunization: DAT (Diphtheria antitoxin) => for neutralization of the toxin Antibiotic Tx: penicillin or erythromycin => slows infection spread by killing the organism, preventing further toxin production Compresses soaked in penicillin applied to lesions Control/Prevention • Active Immunization – toxoid vaccine (DPT) – • Start @ infancy; booster injections – administered @ ~10yr. Intervals throughout life Harvest bacteria purify toxin inactive toxin Formaldehyde toxoid Gram-Positive Rods 1. • Corynebacterium (Corineforms) Diphtheroids – – – – – – Other corynebacterium spp. that morphologically resemble C. diphtheriae Non-pathogenic Normal flora – eyes (conjunctiva), skin, nose, mouth/throat, vagina and urethra (UT) NO toxin production Opportunistic infections, esp. in immunosuppressed pts. Ex. 1. Corynebacterium xerosis – opportunist in eye & postoperative infections 2. Corynebacterium pseudodipheriticum – endocarditis in pts. undergoing cardiac surgery/valvular prostheses Gram-Positive Rods 2. Bacillus – – – Genus: Bacillus Species: Bacillus anthracis – causes anthrax Bacillus cereus – GI infection Microscopic Morphological Appearance • • • • • Large, Gram (+) bacillus ***Spore former*** (Endospores) Non-motile Encapsulated Aerobe (strict or facultative) – – Note: most species of Bacillus are found in soil & water, and are usually encounters in the medical laboratory as airborne contaminants Most clinically important = B. anthracis (Anthrax) Gram-Positive Rods 2. Bacillus – Virulence factors 1. Capsule 2. Exotoxin – complex of 3 protein factors • • • – Edema Factor (EF) Protective Agent (PA) Lethal Factor (LF) => EF + host cell calmodulin Action of Exotoxin • PA inserts into the cytoplasmic (phospholipid) membrane of host EF binds to PA transfer of EF into host cytoplasm – PA facilitates transfer of EF into host cytoplasm Gram-Positive Rods 2. Bacillus – Action of Exotoxin (Pathogenesis) • Rxn: EF + calmodulin → → activation of Adenyl Cyclase [ ATP → cAMP] → ↑cAMP => EDEMA – Increased levels of cAMP → cell oversecretion (EDEMA) – Transmission – animal to man • • Cutaneous infection Pulmonary infection • Intestinal infection 3 diff. types of infection -based upon route of entry Gram-Positive Rods 2. Bacillus – Human Anthrax • Causative agent = B. anthacis; rare in US – – • 1984-1997: only 3 cases of cutaneous anthrax reported 2001: 20 cases – probable exposure to B. anthracis powder sent thru US mail; unknown source. Epidemiology – – – – Anthrax is an enzootic disease of worldwide occurrence. Enzootic diseases are endemic to an animal population; occurrence changes little over time. Anthrax affects domestic herbivores » Sheep, goats, horses Transmission to humans by contact w/ infected an. products or contaminated dust (fig 10.6 p. 95) Gram-Positive Rods 2. Bacillus – Human Anthrax • Epidemiology – Infection initiated by subcutaneous innoculation of spores thru incidental skin abrasions – Also, but less frequently, inhalation of spore-laden dust causes Pulmonary Anthrax – Spores can remain viable for many years in contaminated pastures, bones, wool, hair, hides, or other an. materials. » Highly resistant to physical & chemical agents Gram-Positive Rods 2. • Bacillus 3 different types of B. anthracis infection 1. Cutaneous Anthrax – m/c; localized infection of skin; Least dangerous – – – – 2. Inoculation of spores → deposit beneath the skin, where they germinate → resulting in exotoxin production Malignant pustule – located on hands, forearms and head Eschar – black scab (painless) Possible invasion to regional lymph nodes, then entry into general circulation Pulmonary Anthrax = Woolsorter’s Disease – Most serious, but least common in US; mortality rate ~100% – – – – – Inhalation of spores → deposit in lung alveoli Characterized by progressive hemorrhagic lymphadenitis Occupational risk groups; transmission of spore to individuals working w/ infected animals Sx’s: onset – sudden w/ high fever & respiratory distress (similar to respiratory infection. Pneumonia is often followed by sepsis and death in untx’ed cases Gram-Positive Rods 2. • Bacillus 3 different types of B. anthracis infection 3. Gastrointestinal Anthrax – – • • Ingestion of spores → exotoxin production in intestinal tract → necrotic lesions Results from eating contaminated meat Immunity = permanent immunity is acquired post infection Treatment: broad spectrum antibiotics; penicillin is NOT recommended b/c of inducible β-lactamase in B. anthracis Control/Prevention • – – – – – Sterilization of wool, hair, etc. prior to the handling of animals Sacrifice of infected animals Immunization of animals Vaccine for workers in high risk occupations – purified toxoid Post-exposure antibiotic prophylaxis Gram-Positive Rods 2. • Bacillus Bacillus cereus – – Common inhabitant of rice when spores NOT killed properly Infection/Disease 1. 2. – Virulence factor • – Enterotoxins Sx’s 1. 2. – Gastroenteritis – Food intoxication: eating cooked, improperly stored rice Emetic-type gastroenteritis Gastroenteritis – abdominal pain, diarrhea Emetic-type gastroenteritis: vomiting Control/prevention • Refrigeration of food – no germination of spores Gram-Positive Rods 3. Listeria – – – – – – – – Spp. are short, slender, Gram (+) rods Non-spore formers Occur in short chains or diplobacilli Intracellular parasites Catalase (+) “tumbling” motility, as seen by light microscopy in liquid medium @ 25°C Distinct from catalase (-) streptococcus & nonmotile corynebacterium Grow facultatively Gram-Positive Rods 3. Listeria – Epidemiology • • • Listeria monocytogenes = ONLY spp that infects humans Listeria spp are widespread in nature among animals Human infections are usually food-borne 2-3% processed dairy products (ice cream, cheese) 20-30% ground meats Majority of retail poultry Refrigeration does NOT suppress growth in food 1-15% of healthy humans are asymptomatic intestinal carriers Infections are m/c in pregnant females, fetuses/newborns, immunocompromised individuals (i.e., elderly, corticosteroid use) 200 cases reported/yr. in US w/ 450 deaths & 100 stillbirths Gram-Positive Rods 3. Listeria – Pathogenesis of L. monocytogenes (fig 10.8 p.98) • • • Attaches to & enters a variety of mammalian cells by normal phagocytosis (i.e., macrophages) Escape from phagocytic vacuole d/t formation of Listeriolysin O, a membrane-damaging toxin. Growth in host cell cytoplasm, stimulating changes in cell function that facilitate its direct passage from cell-to-cell Assembly of actin filament tail that pushes the bacterium to the surface of the macrophage Pseudopod extension forms, facilitating transfer into another phagocyte. Membrane-degrading phospholipases mediate passage of org into next cell w/ IS avoidance Gram-Positive Rods 3. Listeria – L. monocytogenes Clinical Disease (Listeriosis) • • • • M/C = septicemia & meningitis Focal skin lesions (granulomatous) sometimes seen Immunocompromised individuals w/ defects in cellular immunity – potential serious infections Pregnant females in 3rd trimester may have mild “flu-like” illness – This and asymptomatic colonization of vaginal tract – can allow organism to be transmitted to newborn » L. monocytogenes = common cause of newborn meningitis Gram-Positive Rods 3. Listeria – Laboratory Dx of L. monocytogenes • • • Isolation of organism from Blood, CSF Blood agar – production of small colony, surrounded by narrow zone of β-hemolysis Distinguishable from streptococci + motility Production of catalase – – Treatment: antibiotic therapy Prevention: proper food preparation & handling Gram-Positive Rods • Miscellaneous Non-spore forming, G(+) Rods 1. Propionibacterium – – – – 2. Lactobacillus – – – – 3. Common inhabitants of normal skin Genus of anaerobic or microaerophilic rods of diphtheroid-like morphology Rare cases of endocarditis P. acnes = strict anaerobe; causes acne Commensal flora of human mucous membranes Produce lactic acid during fermentation Assist in maintaining acid pH of normal mucous epithelia Acid production by oral lactobacilli => dental caries Erysipelothrix rhusiopathiae – – Filamentous, Gram (+) rod that causes dis. in animals Rare skin infection in humans who handle animal products (i.e., butchers, DVM’s, fisherman) Chapter 11: Neisseriae • Genus Neisseriae consists of Gram-negative, aerobic cocci. – – Organisms primarily reside on mucosal surfaces 2 Neisseriae spp are pathogenic for humans 1. N. gonorrhoeae (gonococcus) Cuasative agent for gonorrhea 2. N. meningitidis (meningococcus) Frequent cause of meningitis – Gonocci & Meningococci • • Both are non-motile DIPLOCOCCI; look very similar Both are pyogenic cocci b/c infections are characterized by production of purulent material comprised largely of WBC’s Neisseriae • General characteristic of the Genus 1. Gram-negative Diplococci (kidney-bean shaped) Small, round, glistening, white-to-cream colored after 24 hr. colonization Non-hemolytic Non-motile Non-spore forming Oxidase-positive (presence of enz. cytochrome oxidase – for rapid dx) Fastidious growth requirements 2. 3. 4. 5. 6. 7. • • • • 8. 9. 10. 11. Optimal growth temp = 37°C Aerobic or microaerophilic, utilizing an oxidative form of metabolism Require atmosphere of 5% CO2 Require thiamine and thiamine pyrophosphate for nucleic acid biosynthesis Produces catalases, using the enzymes for fermentation of certain CHO’s Highly Autolytic – autolysis causes cell wall breakdown (PG fragments) – highly inflammatory Highly sensitive to dessication d/t capsular polysaccharide Laboratory tests for distinguishing pathogenic strains from commensal strains N. gonorrhoeae => (+) for glucose utilization, (-) for maltose utilization N. meningitidis => (+) for glucose utilization, (+) for maltose utilization Neisseriae • NEISSERIAE GONORRHOEAE – One of m/freq’ly reported infectious diseases in US – Causative agent = N. gonorrhoeae, a Gram (-) Diplococcus – Commonly found w/in PMN leukocytes of clinical samples – Transmitted via sexual contact; rarely during delivery thru infected vaginal canal – Survival rate outside body = LOW d/t high sensitivity to drying – Epidemiology: major health problem worldwide Neisseriae • NEISSERIAE GONORRHOEAE – Structure of Gonococci: Unencapsulated, piliated, non-motile, diplococci 1. Pili – hairlike surf. Appendages; • • • • VIRULENCE Factor! Composed of protein pillin Enhance attachment to host epithelial & mucosal cell sufaces Confers resistance to phagocytosis Potential to produce genetically different pilin molecules over time – antigenic variation or gene conversion Neisseriae • NEISSERIAE GONORRHOEAE – Structure of Gonococci: Unencapsulated, piliated, non-motile, diplococci 2. Lipoligosaccharide (LOS) • • w/ shorter, more highly branched, non-repeat O-antigenic side chains that do the LPS’s of other Gram-negative bacteria Human serum IgM Ab’s are directed toward LOS Ag’s 3. Other Membrane Proteins (OMPs) • • Contribute to the virulence of N. gonorrhoeae OMP II = “opacity protein” b/c its presence renders gonococcal colonies less translucent; along w/ pili – mediated attachment of organism to host cell. Neisseriae • NEISSERIAE GONORRHOEAE – Pathogenesis • Pili & OMP II => facilitate adhesion to epithelial cells of urethra, rectum, cervix, pharynx, conjunctiva – Make colonization possible • Production of IgA protease that cleaves human IgA Ab’s – evasion of IS response – Seen w/ BOTH gonococci & meningococci Neisseriae • NEISSERIAE GONORRHOEAE – Clinical Notes • 4th m/c Sexually Transmitted organism today • Colonization of mucous membrane of GU tract of rectum • Cause localized infection w/ production of pus • May lead to tissue invasion, chronic inflammation & fibrosis • Females > males w/ regard to being asymptomatic carriers – can transmit gonococcal infection Neisseriae • NEISSERIAE GONORRHOEAE – Clinical Diseases 1. Genitourinary Tract infections • • Acute & easy to Dx in Males Pt. presents w/ yellow, purulent urethral discharge & painful urination. Female – infection w/in endocervix (cervicitis) & extends to urethra & vagina m/c presentation = greenish-yellow discharge; intermenstrual bleeding is possible May progress to uterus, causing Salpingitis (inflammation of Uterine/Fallopian Tubes), Pelvic Inflammatory Disease (PID): gonococci ascend to Reprod. Tract – affect uterus, ovaries & contiguous structures; destruction of upper reproductive tract mucosa 20% infertility rate w/ gonoccocal salpingitis d/t tubal scarring Neisseriae • NEISSERIAE GONORRHOEAE – Clinical Diseases 2. Rectal Infections (Proctitis) – seen w/ male homosexuals • Sx’s: constipation, painful defecation, purulent discharge 3. Pharyngitis • • Contracted by oral-genital contact Sx’s: purulent exudate; may mimic mild viral or streptococcal sore throat 4. Opthalmia Neonatoreum • • • Infection of the conjunctival sac acquired by newborn during passage thru infected birth canal Blindness if untreated Tx: 1% Silver Nitrate on eyes prevents disease or 1% Tetracycline or 0.5% erythromycin Neisseriae • NEISSERIAE GONORRHOEAE – Clinical Diseases 5. Disseminated Infection/Bacteremia • • Bacteremia is rare d/t limited gonococcal ability to multiply in bloodstream (NOTE: meningococcal multiply rapidly in the blood) Some gonococcal strain w/ ability to cause bacteremia Gonococci cross mucosal barrier d/t blood-barrier breakdown; blood culture (+) for Gram (-) Diplococci Sx’s (Both male & female; m/c in females, though): Fever; painful, purulent arthritis; small pustules on skin scattered on a erythematous base – may develop into necrosis Gonococcal = m/c cause of septic arthritis in sexually active adults Neisseriae • NEISSERIAE GONORRHOEAE – Clinical Laboratory Identification • Males: numerous neutrophils )PMN’s( containing Gram (-) diplococci in urethral exudate = provisional Dx – start TX. • Females: a positive gonococcal culture needed to Dx infection • If bacteremia suspected – additional cultures from skin lesions, joint fluid, blood Neisseriae • NEISSERIAE GONORRHOEAE – Clinical Laboratory Identification 1. Growth conditions • • • • • • Growth best under aerobic conditions Most strains require enhanced CO2 N. gonnorrhoeae ferments glucose (not maltose, lactose or sucrose) Oxidase-positive Mixed growth seen on plain Chocolate Agar medium (non-selective medium) Pure culture (selective growth) seen w/ Thayer-Martin Chocolate Agar Medium – to isolate gonoccoci Neisseriae • NEISSERIAE GONORRHOEAE – Clinical laboratory Identification 2. Selective Media • – Thayer-Martin chocolate agar medium contains several antibiotics that suppress the growth of non-pathogenic neisseriae and other normal/abnormal flora Important medium for cultures obtained from GU tract & rectum Culture of N. gonorrhoeae on Thayer-Martin agar is the “goldstandard” for DX Treatment & Prevention (diff to control b/c dis tied to sexual promiscuity) • • • • >20% of gonococcal isolates are resistant to penicillin, tetracycline, cefoxitin, =/or spectinomycin Penicillin-resistant organisms = Penicillinase-producing N. gonorrhoeae Tx w/ 3rd generation cephalosporins for uncomplicated infections of urethra, endocervix or rectum Abstinence, avoiding casual sexual contact, limiting # of sexual partners, taking birth control measures (i.e., condom use) Neisseriae • NEISSERIA MENINGITIDIS – One of the m/c causes of MENINGITIS – Causative agent = N. meningitidis – Infection can take form of fulminant meningococcemia, w/ intravascular coagulation, circulatory collapse, and potentially fatal shock (w/out meningitis) – Outbreaks common in winter & early spring; favored by close contact • Schools, institutions, military barracks – N. meningitidis – afflicts young, previous well individuals; and can progress to DEATH in hours Neisseriae • NEISSERIA MENINGITIDIS – Structure of meningococci • Non-motile, Gram (-) Diplococci; always found in pairs • Piliated – pili allow attachment to nasopharyngeal mucosa, where organism it harbored in carriers and those w/ disease. • Encapsulated – Meningococcal polysaccharide capsule = antiphagocytic; most important VIRULENCE factor! Neisseriae • NEISSERIA MENINGITIDIS – Structure of meningococci 1. Serogroups14 different capsular polysaccharide types (LOS) • • • Most infections w/ serogroups A, B, C, W and Y 90% w/ A, B, and C Serogroup A => massive epidemics in developing countries Serogroup B => most predominant cause of disease and mortality in US 2. Serotypes • 2nd classification sys: serotyping (1,2,3,….20) Serological, based upon properties of OMPs and LOS Neisseriae • NEISSERIA MENINGITIDIS – Pathogenesis • Maintenance of infection conferred by the meningococcal capsule w/ antiphagocytic properties • LOS is released during autolysis & bacteial cell division – toxic effects in disseminated dis. • Production of IgA protease that cleaves human Ab IgA – evasion of the IS response Neisseriae • NEISSERIA MENINGITIDIS – Clinical Notes • N. meningitidis – initial colonization w/in nasopharynx, causing asymptomatic meningococcal pharyngitis • In young & immunocompromised, organism can gain entry to bloodstream (disseminated dis or bacteremia) meningitis +/or fulminant septicemia • N. meningitidis = m/c cause of meningitis Neisseriae • NEISSERIA MENINGITIDIS – Clinical Diseases 1. Meningitis • • • • • • • Meningococci normally inhabit nasopharynx (barrier to the bacteria; no blood entry) If meningococci penetrate barrier and enter blood – can rapidly multiply => Meningococcemia Sx’s: fever, if not severe case If organism crosses BBB and seed the meninges – multiply & induce Inflammatory Response, accomp’d by influx of PMN Leukocytes result = purulent meningitis Joint sx’s and petechial rash – common After initial fever & malaise, severe HA, rigid neck (stiff neck & back), vomitting & sensitivity to lights Orthopedic Test: Kernig’s Sign A sx. of meningitis evidenced by reflex contraction & pain in Hamstring m. when attempting to extend the leg after flexing the thigh upon the body. Neisseriae • NEISSERIA MENINGITIDIS – Clinical Diseases 2. Septicemia • • • Life-threatening in <12 hrs in healthy individuals 30% pts w/ meningitis progress into fulminant septicemia Severe septicemia & shock (exotoxin LOS responsible) Seen mainly in very young children Waterhouse-Friderichsen Syndrome: an acute adrenal insufficiency d/t hemorrhage into the adrenal gland caused by meningococcal infection, characterized by: large, purple, blotchy skin hemorrhages; vomiting and diarrhea; circulatory collapse; necrosis of the adrenals; death w/in 10-12 hrs. Neisseriae • NEISSERIA MENINGITIDIS – Clinical Laboratory Identification • Gold standard for Dx of systemic meningococcal infection is isolation of N. meningitidis from CSF – – Under light microscope, specimens obtain from CSF or skin lesion aspirates appear as Gram (-) Diplococci, often in association w/ PMN leukocytes Carriers: swab the nasopharynx 1. Culture Conditions • • • Chocolate Agar w/ increased CO2 Selective medium is NOT required b/c samples usually taken from STERILE CSF Thayer-Martin chocolate agar – needed for samples obtained from skin lesions, nasopharyngeal swabs => eliminate contam Neisseriae • NEISSERIA MENINGITIDIS – Clinical Laboratory Identification 2. Additional Tests • • All Neisseria spp are Oxidase-positive Differentiation between species, therefore, is by sugar fermentation • • • N. meningitidis ferments BOTH glucose & maltose N. gonorrhoeae ferments ONLY glucose CSF in bacterial meningitis Increased pressure Elevated protein Decreased glucose (b/c of bacterial consumption) Increased # of neutrophils Note: presence of the organism or of antigenic capsular substance => confirms the DX Neisseriae • NEISSERIA MENINGITIDIS – Treatment & Prevention • • Bacterial meningitis is a Medical Emergency!!! High fever, HA, and rash are tx’ed immediately to prevent fulminant septicemia (i.e., to prevent DEATH) – • 1. Penicillin G and ampicillin use; or cefotaxime or ceftriaxone Diagnosis • 2. Confirmation of bacteriologic dx: too much time Gram-stains of CSF, latex agglutination tests with serogroup specific anticapsular Ab – for rapid presumptive Dx Vaccines • Conjugate meningococcal vaccine (MCV4) approved in 2005 for use in adolescents and adults 11-55 yoa • 3. Tetravalent vaccine w/ capsular polysacch’s from serogroups A,C, W-135, and Y conjugated to the diphtheria toxoid – confers T-cell memory Prophylaxis • Rifampin – usu. used to tx family members of an infected individual; effective in eliminating carrier state