Chapter 3
advertisement

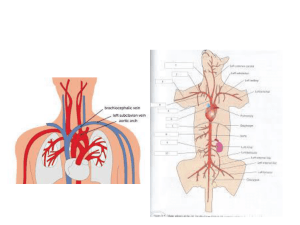
Fundamentals of Nursing: Standards & Practices, 2E Chapter 35 Skin Integrity and Wound Healing Wounds The skin is the body’s largest organ and is the primary defense against infection. A disruption in the integrity of body tissue is called a wound. Copyright 2002 by Delmar, a division of Thomson Learning 35-2 Physiology of Wound Healing Defensive (inflammatory) phase Reconstructive (proliferative) phase Maturation phase Copyright 2002 by Delmar, a division of Thomson Learning 35-3 Types of Healing Primary intention healing Secondary intention healing Tertiary intention healing Copyright 2002 by Delmar, a division of Thomson Learning 35-4 Kinds of Wound Drainage Serous exudate Purulent exudate Hemorrhagic exudate Copyright 2002 by Delmar, a division of Thomson Learning 35-5 Factors Affecting Wound Healing Age Nutrition Oxygenation Smoking Drug therapy Diabetes mellitus Copyright 2002 by Delmar, a division of Thomson Learning 35-6 Hemorrhage Some bleeding from a wound is normal during and immediately after initial trauma and surgery. Hemostasis usually occurs within a few minutes. Hemorrhage (persistent bleeding) is abnormal and may indicate a slipped surgical suture, dislodged clot, or erosion of a blood vessel. Copyright 2002 by Delmar, a division of Thomson Learning 35-7 Swelling in the area around the wound or affected body part and the presence of sanguinous drainage from a surgical drain may indicate internal bleeding. Symptoms of hypovolemic shock include decreased blood pressure, rapid thready pulse, increased respiratory rate, diaphoresis, restlessness, and cool clammy skin. Copyright 2002 by Delmar, a division of Thomson Learning 35-8 A hematoma is a localized collection of blood underneath the tissues;it may also be seen and appear as a reddish blue swelling or mass. External hemorrhaging is detected when the surgical dressing becomes saturated with sanguinous drainage. Copyright 2002 by Delmar, a division of Thomson Learning 35-9 Infection Bacterial wound contamination is one of the most common causes of altered wound healing. A wound can become contaminated preoperatively, intraoperatively, or postoperatively. Copyright 2002 by Delmar, a division of Thomson Learning 35-10 If the amount of bacteria in a wound is sufficient or the client’s immune defenses are compromised, clinical infection may result and become apparent 2 to 11 days postoperatively. Copyright 2002 by Delmar, a division of Thomson Learning 35-11 Infection prolongs the inflammatory phase of healing, competing for nutrients, and producing chemicals and enzymes that are damaging to the tissues. Copyright 2002 by Delmar, a division of Thomson Learning 35-12 Dehiscence and Evisceration Dehiscence is the partial or complete separation of the wound edges and the layers below the skin. Evisceration occurs when the client’s viscera protrude through the disrupted wound. Wound dehiscence is most likely to occur 4 to 5 days postoperatively. Copyright 2002 by Delmar, a division of Thomson Learning 35-13 Wound Classification Wounds are usually described based on their etiology. The treatment for the wound varies depending on the underlying disease process. Copyright 2002 by Delmar, a division of Thomson Learning 35-14 Classification systems describe the cause of the wound, the status of skin integrity, the extent of tissue damage, cleanliness of the wound, or descriptive qualities of the wound (such as color). Copyright 2002 by Delmar, a division of Thomson Learning 35-15 Examples of classifications systems • RYB classification system • Wagner ulcer grade classification • Classification by thickness of skin loss Copyright 2002 by Delmar, a division of Thomson Learning 35-16 Assessment of Wounds Health history • Conducted to elicit information regarding medical conditions or disease processes that are often associated with delayed or disrupted healing • Should include aggravating and alleviating factors - allergies to tape, latex, medications, or other substances Copyright 2002 by Delmar, a division of Thomson Learning 35-17 Physical examination • • • • • Location of wound Size of wound General appearance and drainage Pain Laboratory data Copyright 2002 by Delmar, a division of Thomson Learning 35-18 Nursing Diagnoses Impaired Tissue Integrity Risk for Infection Acute or ChronicPain Disturbed Body Image Deficient Knowledge Copyright 2002 by Delmar, a division of Thomson Learning 35-19 Outcome Identification and Planning The goals for clients with wounds generally focus on promoting wound healing, preventing infection, and educating the client. Copyright 2002 by Delmar, a division of Thomson Learning 35-20 Implementation Initiate emergency measures. Cleanse the wound (review Procedure 35-2 on irrigating a wound). Dress the wound (review Procedure 35-3 on applying a dry sterile dressing and Procedure 35-4 on applying a wet to dry dressing). Monitor drainage of wounds. Copyright 2002 by Delmar, a division of Thomson Learning 35-21 Provide suture care. Check bandages, binders, and slings. Administer heat and cold therapy (review Table 35-5 for overview of heat and cold applications). Copyright 2002 by Delmar, a division of Thomson Learning 35-22 Evaluation If the goals are not achieved, the nurse will need to examine the nursing interventions and strategies that were employed, and revise the nursing care plan accordingly. It is important to review techniques and procedures, especially those performed by the client or other caregivers. Copyright 2002 by Delmar, a division of Thomson Learning 35-23 Pressure Ulcers Pressure ulcers, also known as bedsores or decubitus ulcers, are localized areas of tissue necrosis that tend to develop when soft tissue is compressed between a bony prominence and an external surface for a prolonged period of time. Pressure ulcers are due to ischemia. Copyright 2002 by Delmar, a division of Thomson Learning 35-24 Physiology of pressure ulcers • The reduction of blood flow causes blanching of skin when pressure is applied. • Other forces acting in conjunction with pressure contribute to pressure ulcer formation - shearing and friction. Copyright 2002 by Delmar, a division of Thomson Learning 35-25 Risk factors for pressure ulcers • • • • • • • Immobility Inactivity Incontinence Malnutrition Decreased mental status Diminished sensation Age-related changes Copyright 2002 by Delmar, a division of Thomson Learning 35-26 Assessment • • • • Stage I Stage II Stage III Stage IV Copyright 2002 by Delmar, a division of Thomson Learning 35-27 Nursing Diagnoses • Nursing diagnoses for clients with pressure ulcers will be similar to those for clients with wounds. • Using diagnoses such as Body Image Disturbance and Anxiety will ensure that the client’s symptoms are addressed holistically. Copyright 2002 by Delmar, a division of Thomson Learning 35-28 Outcome identification and planning • Individualized outcomes based on the client’s overall physical condition, the stage of the wound, and the client’s risk factors will help in identifying priority interventions. • Client teaching should be included as an integral part of the planning process. Copyright 2002 by Delmar, a division of Thomson Learning 35-29 Implementation • • • • Ensure proper hygiene and skin care. Provide proper positioning. Employ support surfaces. Apply complementary therapies. Copyright 2002 by Delmar, a division of Thomson Learning 35-30 Evaluation • Evaluation of the plan of care for a client with a pressure ulcer will consider the physical signs of healing and the status of the pressure ulcer, as well as the client’s adaptation to the altered skin integrity. • Each intervention should be evaluated for its effectiveness. Copyright 2002 by Delmar, a division of Thomson Learning 35-31