mechanical properties of the heart
advertisement

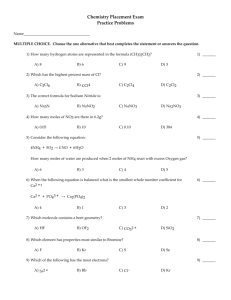
MECHANICAL PROPERTIES OF THE HEART Sandor Gyorke, Ph.D. Office: DHLRI 507 Telephone: (614) 292-3969 Learning Objectives • Compare and contrast cardiac and skeletal muscle cells in terms of mechanisms of contraction and relaxation, cross bridging, and ion transport. • Define the determinants of myocardial oxygen consumption • Relate cardiac muscle mechanics to ventricular function using LaPlace’s Law: define pressure and volume work • Describe the effects of parasympathetic and sympathetic stimulation on cardiac muscle cells. Learning Resources Pathophysiology of heart disease. Fifth Edition, Ed. L.S. Lilly, Lippincott Williams & Wilkins, Baltimore, MD, 2011 (pp. 23-27; 28-43; 217-227) D.E. Mohrman & L.J. Heller. Cardiovascular Physiology, 8th edition, McGraw-Hill, New York 2014. Lecture Topics • Cardiac excitation-contraction coupling. • Modulation of myocyte calcium handling by parasympathetic and sympathetic influences. • Force-length relationships. • Myocardial oxygen consumption. Introduction • Heart muscle has many properties in common with skeletal muscle. Both muscles are striated, and have similar contractile elements including sarcomeres that contain thick and thin filaments. The basic principles of muscle structure and function are covered in the Bone and Muscle block. • At the same time many important functional and morphological differences exist between cardiac and skeletal muscles, including differences in Ca2+ handling, connectivity, and energetics. • This eModule will focus on principles underlying the clinically relevant concepts of myocardial contractility and pressurevolume relationships as well as oxygen consumption. Excitation-Contraction Coupling in Cardiac Muscle Na+-Ca2+ exchange Na+ Sarcolemma Ca2+ Ca2+ Na+ channel Na+ T-tubule Ca2+ ATP Troponin-C Ca2+ Ca2+ channel Sarcoplasmic reticulum Ryanodine receptor Sequence of Events in Cardiac ExcitationContraction Coupling • Action potential (AP) propagates over the surface of the myocyte and into the myocyte along the T-tubule. • The AP in the T-tubule opens voltage dependent Ca2+ channels allowing the entry of Ca2+ from the extracellular fluid into the cell. • This rise in cytosolic [Ca2+] causes the release of a larger pool of Ca2+ stored in the sarcoplasmic reticulum (SR) through Ca2+ release channels called ryanodine receptors. This mechanism is known as Ca2+-induced Ca2+ release. • The released Ca2+ binds to troponin, which disinhibits actin and myosin interactions and results in force production. • Contraction ends when released [Ca2+] is pumped back to the SR by Ca2+ ATPase Relation Between Tension and Cytosolic Calcium Concentration in Cardiac Muscle Relative force (%) 100% peak of enhanced contraction Diastole 10 peak of normal contraction -7 [Ca2+]i (molar) 10 -5 •The rise in [Ca2+] in normal cardiomyocytes during a beat is only large enough to produce a fraction of the intrinsically available tension. •The strength of contraction can be increased by increments of [Ca2+] attained via inotropic interventions. Similarities Between Length-Tension and VolumePressure Relationships 100 50 peak resting Pressure (mm Hg) Force (100% maximum) 200 Intraventricular systolic pressure Intraventricular diastolic pressure 100 0 0 60 120 Length (% resting) 180 Peak and resting force produced by a stimulated and unstimulated, respectively, cardiac muscle strip. 0 100 200 Diastolic volume (ml) The intraventricular systolic pressure is similar in shape to the total force development measured in a muscle strip. Contractility Positive and Negative Inotropes CONTRACTILITY (or INOTROPIC STATE) is defined as the strength of contraction at a constant initial muscle (sarcomere) length Inotropic interventions that increase contractility are called POSITIVE INOTROPES (noradrenaline, digoxin) Inotropic interventions that decrease contractility are called NEGATIVE INOTROPES (acetylcholine, Ca2+ channel blockers) Positive and Negative Inotropic Effects on the Ventricular Volume-Pressure Curve Ventricular pressure norepinephrine (digoxin) control acetylcholine End-Diastolic volume (Ca-channel blockers, Heart failure) Molecular Mechanisms of Positive Inotropic Effects of Norepinephrine Ca Channel Norepinephrine AC b -R Gs P ATP cAMP PKA C Phospholamban P SR CaATPase R C Myosin ATP Ca2+ Sarcoplasmic reticulum Molecular Mechanisms of Negative Inotropic Effects Of Achetylcholine Ca Channel Ach AC mAchR Gi ATP cAMP Mode of Action of Digoxin in Increasing Intracellular Cystolic Calcium Concentration [Ca2+] Na+ -Ca2+ exchange digoxin (-) 3Na+ 3Na+ (-) 2K+ Ca2+ (-) [Ca2+] [Na+] raises Metabolism • High fatigue resistance due to a large number of mitochondria (oxidative phosphorylation) and a good blood supply, which provides nutrients and oxygen. • Most of energy comes from fatty acids and carbohydrates. • Only ~1% of energy is derived from anaerobic metabolism (through lactate production) at basal metabolic rates. • In ischemic conditions not enough ATP can be produced to sustain ventricular contractions. Main Sources of ATP Production in Cardiac Muscle ADP + Pi Lactic acid ATP Amino acids and ketones Glycogen (5%) Glucose Fatty acids Oxygen Glycolysis (35%) (60%) Oxidative Phosphorylation Major Determinants of Myocardial Oxygen Consumption (MVO2) Organ MVO 2 Cardiac State MVO2 (ml O2/min per 100g) (ml O2/min per 100g) Brain 3 Kidney 5 Skin 0.2 Arrested heart 2 Resting heart rate 8 Resting muscle 1 Heavy exercise 70 Contracting muscle 50 Myocardial O2 consumption Heart rate Contractility Wall tension (T = Pr/2h, T-wall tension, P intraventricular pressure, r-radius, and h-wall thickness) Coronary blood flow. Vascular tone (adenosine and nitric oxide, etc) Mechanical factors (compression) Summary • • • • The Ca2+ which enters the cardiomyocyte during the action potential triggers Ca2+induced Ca2+ release from the sarcoplasmic reticulum (SR), causing contraction by sliding of thick and thin filaments. The force of contraction is modulated by increasing or decreasing the amount of Ca2+ released from the SR and bound to troponin binding sites. Sympathetic stimulation, results in phosphorylation of Ca2+ channels and of the SR Ca2+ pump regulatory protein phospholamban, thereby increasing SR Ca2+ release and contractility (positive inotropy). Stimulation of the parasympathetic system reduces contractility by reducing phosphorylation of the same proteins (negative inotropy). An increase in myocardial fiber length (as occurs with augmented ventricular filling) increases contractile strength due to a more optimal overlap between the thin and thick filaments (Frank-Starling relationship). The heart relies almost entirely on aerobic metabolism for energy production. Carbohydrates and fatty acids used as energy sources, the energy of which is converted into ATP by oxidative metabolism in the mitochondria. Thank you for completing this module Questions? sandor.gyorke@osumc.edu