Anesthesiology Exam 1 6B 1. The following are objectives of
advertisement
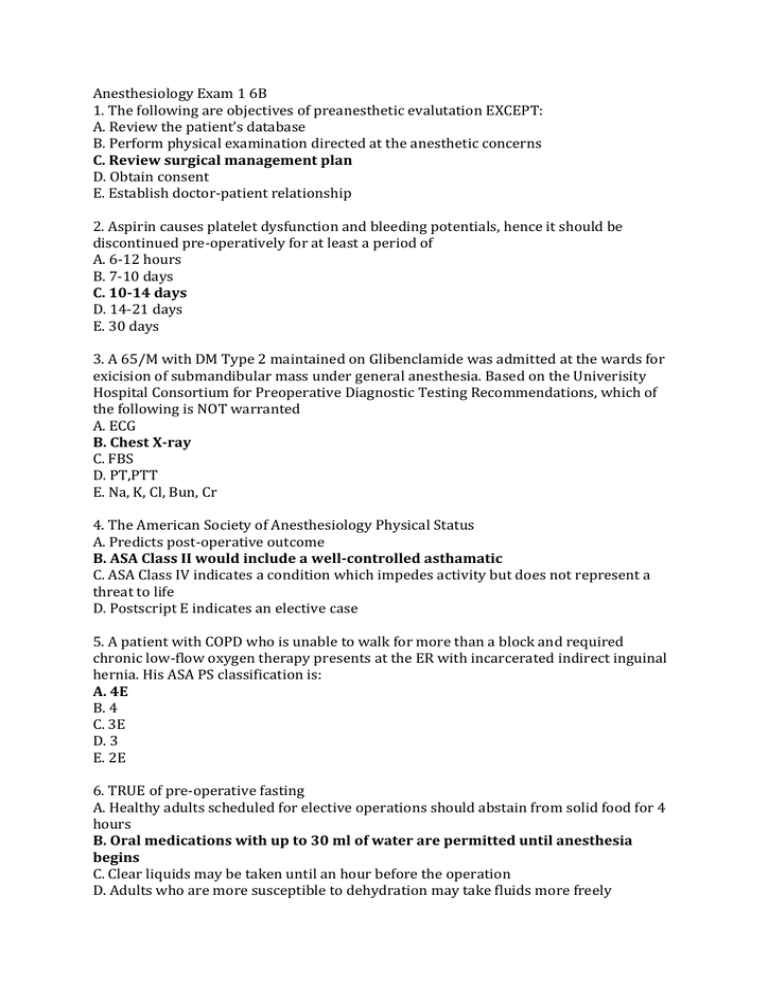
Anesthesiology Exam 1 6B 1. The following are objectives of preanesthetic evalutation EXCEPT: A. Review the patient’s database B. Perform physical examination directed at the anesthetic concerns C. Review surgical management plan D. Obtain consent E. Establish doctor-patient relationship 2. Aspirin causes platelet dysfunction and bleeding potentials, hence it should be discontinued pre-operatively for at least a period of A. 6-12 hours B. 7-10 days C. 10-14 days D. 14-21 days E. 30 days 3. A 65/M with DM Type 2 maintained on Glibenclamide was admitted at the wards for exicision of submandibular mass under general anesthesia. Based on the Univerisity Hospital Consortium for Preoperative Diagnostic Testing Recommendations, which of the following is NOT warranted A. ECG B. Chest X-ray C. FBS D. PT,PTT E. Na, K, Cl, Bun, Cr 4. The American Society of Anesthesiology Physical Status A. Predicts post-operative outcome B. ASA Class II would include a well-controlled asthamatic C. ASA Class IV indicates a condition which impedes activity but does not represent a threat to life D. Postscript E indicates an elective case 5. A patient with COPD who is unable to walk for more than a block and required chronic low-flow oxygen therapy presents at the ER with incarcerated indirect inguinal hernia. His ASA PS classification is: A. 4E B. 4 C. 3E D. 3 E. 2E 6. TRUE of pre-operative fasting A. Healthy adults scheduled for elective operations should abstain from solid food for 4 hours B. Oral medications with up to 30 ml of water are permitted until anesthesia begins C. Clear liquids may be taken until an hour before the operation D. Adults who are more susceptible to dehydration may take fluids more freely 7. The size of the blood pressure cuff influences the pressure reading. The minimum cuff width is approximately ____ percent of the circumference of the extremitiy. A. 30 B. 40 C. 50 D. 60 E. 70 8. A progressive decrease in the end-tidal CO2 occurs with the following EXCEPT: A. Thromboemboli B. Hypothermia C. Failing cardiac output D. Hyperventilation E. None of the above 9. Core temperature reflects the temperature of vital organs and is measured in the following EXCEPT: A. Central blood B. Rectum C. External auditory canal D. Midesophagus E. Nasopharynx 10. The most important monitor for all patients undergoing anesthesia is A. Blood pressure B. Pulse Oximeter C. You D. ECG 11. Physical finding/s that suggest/s difficult airway management include/s: A. Thyromental distance less than 60 mm B. Cervico-occipital extension limited to an angle at the hyoid less than 160 degrees C. Mouth opens less than 40 mm D. Atrophic mandible and chin E. All of the above 12. Visualization of only the posterior structures of the glottis during direct laryngoscopy classifies the patient under Cormack-Lehane grade: A. I B. II C. III D. IV E. V 13. In Sellick’s maneuver, external pressure is applied on the ______ against the vertebral bodies deterring regurgitation of gastroesophageal contents. A. Thyroid cartilage B. Cricoid cartilage C. Epiglottic cartilage D. Arytenoid cartilage 14. The major cause of airway obstruction in anesthetized patients is: A. Tongue B. Prominent maxillary incisors C. Tonsils D. Pharyngeal edema 15. After denitrogenation with 100% oxygen, the functional residual capacity contains: A. 3-5 minutes of oxygen supply B. 5-7 minutes of oxygen supply C. 8-10 minutes of oxygen supply D. 10-12 minutes of oxygen supply 16. Maneuver(s) to relieve airway obstruction include(s): A. Chin lift and jaw thrust B. Insert oral/nasal airway C. Turning the head to one side D. A and B E. A, B and C 17. Best criteria for a successful endotracheal intubation A. Misting of the endotracheal tube B. Equal breath sounds C. Direct visualization of the glottis E. Carbon dioxide on capnography 18. For adults, endotracheal intubation is more common in the: A. Left main stem bronchus B. Right main stem bronchus C. Both 19. During laryngoscopy, which of the following axes should be aligned? A. oral, laryngeal, tracheal B. oral, pharyngeal, tracheal C. laryngeal, pharyngeal, tracheal D. oral, laryngeal, pharyngeal 20. Mallampati 3 is described as A. Hard palate B. Soft palate, fauces, uvula, pillars C. Soft palate, uvular base D. Soft palate, fauces, uvula BONUS Enumerate the layers traversed during subarachnoid block (median approach). Skin, subcutaneous tissue, supraspinous ligament, interspinous ligament, ligamentum flavum dura Anesthesiology Exam 2 6B 1. The pharmacokinetics of a drug is separated into 3 categories that include the following EXCEPT A. Absorption B. Distribution C. Elimination D. Metabolism 2. The following statements refer to the phenomenon called the first-pass effect EXCEPT A. It results in decreased bioavailability B. It is minimized by administering the drug via intravenous, rectal, or sublingual routes C. It is decreased in those with cirrhotic liver disease D. It determines how much of the drug is in the un-ionized lipid soluble form 3. The fraction of administered drug that reaches either the site of action or biologic fluid with access to the site of action is known as the A. Bioequivalence B. Bioavailability C. Potency D. Efficacy 4. Which of the following inhalational agents cause generalized-tonic clonic seizures? A. Isoflurane B. Sevoflurane C. Desflurane D. Enflurane 5. Which of the following statements is true about minimum alveolar concentration? A. It is specific for each volatile anesthetic. B. It is increased with the use of propofol. C. It is a standard measure of efficacy of inhaled anesthetics. D. It is best measured by capnography through the inspired concentration 6. Arrange the following volatiles in order of decreasing MAC A. Desflurane > sevoflurane >isoflurane >halothane B. Halothane>isoflurane>sevoflurane>desflurane C. Sevoflurane>desflurane>halothane>isoflurane D. Isoflurane>halothane>desflurane>sevoflurane 6. Which of the following statements best describes nitrous oxide? A. The amount of nitrous oxide remaining in the cylinder tank is measured. B. Nitrous oxide decreases the potency of other volatile anesthetics. C. Nitrous oxide is less soluble in blood as compared to nitrogen. D. Diffusion of nitrous oxide from the blood into the alveoli causes a brief period of hypoxia. 7. TRUE about propofol A. Greater incidence of apnea as compared to thiopental B. The reformulated emulsion does not cause pain on intravenous injection C. Lesser incidence of nausea and vomiting compared with thiopental D. In doses used for induction, BP and heart rate is maintained 8. TRUE about thiopental A. Contraindicated in asthmatic patients B. Prolonged duration of action secondary to drug accumulation C. An additional analgesic effect to complement balanced anesthesia D. Increased cerebral metabolic rate Nos. 9-11. Give the non-opioid intravenous anesthetic most suitable for each clinical scenario. A. Thiopental B. Ketamine C. Propofol 9. 25/F with massive blood loss for radial artery repair. B 10. 5/M with hydrocephalus for VP shunting. A 11. 80/M with blurred vision on one eye for cataract extraction. C 12. On your way to the conference room for a lecture you noticed that your earlier patient has irregular shallow breathing. You further investigated and found out that she has a respiratory rate of 8, pinpoint pupils, blood pressure of 80/50 and a heart rate of 45. During her operation, you recalled that she was given the following agents: lidocaine+epinephrine via epidural catheter, fentanyl, propofol, atracurium, and isoflurane as induction and maintenance medications for general anesthesia and morphine sulfate and ketorolac as post-operative pain medications. The patient’s distress is most probably attributable to: A. Opioid-induced effects B. Residual muscle relaxant c. Sedative overdose D. Prolonged volatile anesthetics. 13. The PACU anesthesia resident came to your rescue and gave a drug intravenously. The patient’s respiration became regular and was now arousable. A few minutes later, vital signs returned to normal. The agent administered by the resident is most likely: A. Naloxone B. Neostigmine C. Flumazenil D. Ephedrine 14. If the drug above is not available, the following may be used as an alternative A. Nalbuphine B. Physotigmine C. Atropine D. Scopolamine 15. The first phase in two-compartment model represents: A. A sharp decline from the peak concentration following administration, representing rapid distribution. B. A slow decline from the trough concentration following administration, representing slow elimination. C. A sharp decline from the peak concentration following administration, representing rapid elimination. D. A slow decline from the trough concentration following administration, representing slow distribution. 16. The following are factors that increase the rate of anesthetic induction EXCEPT A. Increased fresh gas flow B. Second gas effect C. Low blood-gas solubility coefficient D. None of the above 17. The Hoffman elimination refers to: A. Hepatic elimination of Atracurium B. Spontaneous elimination of Atracurium at physiologic pH and temperature C. Ester hydrolysis of Atracurium D. Renal elimination of Atracurium 18. The following best describes succinylcholine: A. It causes a transient rise and fall in blood pressure depending on the prior state of the patient’s autonomic system B. It is a metabolized by acetylcholinesterase in plasma C. It is antagonized by neostigmine D. It causes an exaggerated rise in serum potassium in all patients. 19. A 20/M with a stab wound on the chest was brought to the OR for sternotomy. Your co-decked first year resident has used his last vial of succinylcholine in an earlier operation and was now rummaging wildly through his drug stocks. Having just studied neuromuscular blockade, you know that the alternative for RSI is: A. Pancuronium B. Rocuronium C. Atracurium D. None of the above 20. The following are true about opioids EXCEPT: A. Ventilatory depression is mainly due to the activation of mu opioid receptors B. The analgesic effect of opioids is specific to nociceptive neurons. Non-nociceptive afferents such as pressure, touch, and temperature are preserved. C. The intrinsic efficacy of opioids refers to its ability to accelerate the G proteins D. Naloxone, an opioid agonist-antagonist can precipitate severe abstinence or withdrawa in patients who are dependent on opiods Bonus: Discuss the steps of conducting general endotracheal intubation anesthesia. Anesthesiology Exam 3 Block 6B Multiple Choice 1. Unchanging goals of anesthetic management include: A. Safety B. Comfort C. Efficiency D. All of the above 2. The concept of “good anesthesia” includes the following EXCEPT: A. Making the patient comfortable B. Avoiding complications and “near misses” C. Managing the anesthetic independent of the surgical procedure D. Maintaining pleasant professional relationships with coworkers 3. A 30/M is being operated on for ruptured acute appendicitis under general endotracheal anesthesia using rapid sequence. Intraoperatively, patient suddenly developed tachycardia. Differentials would include the following EXCEPT: A. Pain B. Blood Loss C. Deep Anesthesia D.Hypercapnia TRUE or FALSE 4. Because of unpredictable responses, it seems appropriate to give bolus doses of anesthetics until proper depth of anesthesia is reached. TRUE 5. Just before incision, the alveolar inhaled anesthetic concentration is decreased in anticipation of the patient’s response to painful stimulus. FALSE 6. A properly conducted anesthetic includes a good anesthesia record. TRUE 7. At light depths of anesthesia, responses are less vigorous and movement is absent. FALSE Multiple Choice 8. Local anesthetics block neural conduction by: A. Blocking outflow of sodium ions B. Increase in the resting membrane potential C. Inhibiting the increase in sodium permeability D. Altering the ion gradient 9. The progression of neural blockade is as follows A. Motor -> Pain and Temperature -> Touch and pressure -> proprioception B. Proprioception -> touch and pressure -> pain and temperature -> motor C. touch and pressure -> proprioception -> pain and temperature -> motor D. pain and temperature -> proprioception -> touch and pressure -> motor 10. Which of the following is not an amide? A. Bupivacaine B. Mepivacaine C. Lidocaine D. Tetracaine 11. Onset of local anesthesia is hastened by the following EXCEPT: A. high lipid solubility B. high protein binding C. large volume of the drug D. greater un-ionized form 12. The potency of local anesthetics depend on A. lipid solubility B. pKa C. protein binding D. intrinsic vascular activity 13. Duration of action of local anesthetic is dependent on: A. lipid solubility B. pKa C. protein binding D. intrinsic vascular activity 14. Which of the following agents is the most cardiotoxic? A. Bupivacaine B. Tetracaine C. Lidocaine D. Ropivacaine 15. Which of the following agents is least cardiotoxic? A. Bupivacaine B. Prilocaine C. Lidocaine D. Ropivacaine 16. The maximum dose of lidocaine with epinephrine is A. 3 mg/kg B. 5mg/kg C. 7 mg/kg D. 10 mg/kg 17. Addition of vasoconstrictors to local anesthetics produces the following effects EXCEPT A. Prolongs duration of action B. Increases peak blood concentration C. Permits the use of larger amounts of local anesthestics with less risk of systemic toxicity D. None of the above 18. A 50/F for CTT insertion was given lidocaine via intercostal nerve block. Your buddy-first year resident was then pulled-out to help in a toxic trauma case and you were left alone to monitor the patient. With regards to lidocaine toxicity, which of the following would you expect to appear and thus watch out for? A. circumoral numbness B. seizures C. Sedation D. Agitation 19. After loading the patient with 10 cc of 2% lidocaine via epidural catheter, you noted that the patient’s eyes began rolling upwards and his extremities began to stiffen. Which of the following are you going to do first? A. give midazolam B. give supplemental oxygen C. intubate the patient D. give thiopental 20. At birth the spinal cord extends to A. L1 B. L2 C. L3 D. L4 BONUS: In adults, the spinal cord terminates at: L1-L2 21. After performing a successful subarachnoid block, your resident ask you to test the level of the motor block. You found out that the patient is able to fully raise his knees but unable to dorsiflex the foot. At this point, what is the level of the motor block? A. L2-L3 B. L4-L5 C. T6-T12 D. S1-S2 22. A 75/M with scrotal cancer is brought to the OR for orchiectomy under SAB. What is the minimum dermatome level of anesthetic block required for this procedure? A. T12 B. T8 C. T10 D. T6 23. Which of the following measures is not part of the treatment of post-dural puncture headache? A. abdominal binder B. complete bed rest C. increased oral fluid intake D. coffee 24. Which of the following structures is NOT found within the epidural space? A. Fats B. lymphatic vessels C. venous plexus D. spinal arteries 25. The depth of the epidural space is greatest along the midline at the level of the A. second lumbar interspace B. fourth lumbar interspace C. third lumbar interspace D. fifth lumbar interspace Bonus: What is the distance between the ligamentum flavum and dura in this interspace? 5-6mm 26. The spread of local anesthetics in the epidural space depends on what characteristic? A. volume B. concentration C. dose D. baricity 27. Which of the following is an absolute contraindication to Major Conduction Anesthesia (Regional Anesthesia) A. Hypovolemia B. Sepsis C. patient refusal D. pre-exsiting neurological disease Bonus: Give another absolute contraindication: coagulopathy, infection at site 28. Density of CSF at 37 degrees Celsius is A. 0.997-1.001 g/ml B. 1.001-1.005 g/ml C. 1.005-1.009 g/ml D. NOTA 29. True of caudal anesthesia A. A special form of spinal anesthesia B. Performed with the patient in lateral, prone, jack-knife position C. If performed correctly, CSF can be aspirated from the needle D. All of the above Bonus: The dural sac usually ends at what level? Lower border of S2 in adult 30. During spinal and epidural anesthesia, differential blockade is observed. The correct sequence according to decreasing spinal level is: A. sympathetic>sensory>motor B. Sensory> sympathetic>motor C. Motor>sympathetic>sensory D. sensory> motor>sympathetic Bonus: Spinal column consist of: Cervical vertebrae-7 Thoracic vertebrae-12 Lumbar vertebrae-5 Sacral vertebrae-5







