as a Mentor of SEARCH - SEARCH Health Clinic
advertisement

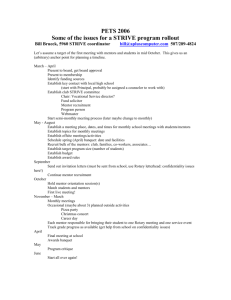
Mentor Volunteer Package 1 Table of Contents 1- Thank You and Requirements…………………………………………….....(page 3) 2- Who Are We………………………………………………………………....(page 4) 3- Mission, Vision & Values…………………………………………………...(page 5) 4- Shift Information…………………………………………………………….(page 6) 5- Teams and Social Programs………………………………………………….(page 7) 6- Policies……………………………………………………………………….(page 8) 7- Child Abuse Disclosure……………………………………………………...(page 14) 8- Code of Ethics: Key Points to Guide our Actions…………………………...(page 16) 9- Professionalism……………………………………………………………....(page 17) 10- Code of Conduct…………………………………………………………….(page 18) 11- Social Determinants of Health………………………………………………(page 19) 12- Cultural and Community Competencies……………………………………..(page 20) 13- Confidentiality Policy………………………………………………………..(page 24) 14- Online Scheduling…………………………………………………………....(page 27) 2 Thank you for your interest in becoming a Mentor at SEARCH! We are excited to have you share your knowledge and professionalism with students, staff and other mentors during SEARCH shifts. We respectfully request that as a mentor you will fulfill the following requirements: 1) Provide a copy of your resume with references. 2) Provide a criminal records check if not required by your professional organization. 3) Provide a copy of proof of registration with your respective professional organization. 4) Provide a copy of proof of malpractice insurance if not included with your professional registration or license. 5) Have experience or willingness to work with issues facing clients living in marginalized circumstances including addictions, poverty, housing, homelessness, mental health, chronic diseases, and different ethnic backgrounds. 6) Experience with teaching, leading, facilitating and working with adults in some capacity is an asset. 7) A willingness to share knowledge and information about your profession in a nonjudgemental and collaborative interprofessional environment. Questions If you have questions regarding SEARCH, contact our Coordinator at reginastudentclinic@gmail.com. 3 Who Are We SEARCH is a student run interdisciplinary health care initiative situated in the North Central Community in Regina. This student run initiative provides access to clinical and social services in an after-hours clinical setting. Primary health care, social programming, childcare, and a meal are offered on a drop-in basis. SEARCH is a non-profit organization and we are supported by the Saskatchewan Ministry of Health, Regina Qu’Appelle Health Region, Four Directions Community Health Centre, North Central Community Association, University of Regina, University of Saskatchewan, First Nations University of Canada, and the Saskatchewan Institute of Applied Science and Technology. Students representing many disciplines are involved in SEARCH including Nursing, Medicine, Social Work, Health Studies, Kinesiology, Education, Dental Hygiene, Physical Therapy, Arts & Science and others. Students are currently volunteering in co-operation with faculty members from the University of Saskatchewan, University of Regina, SIAST, First Nations University of Canada, their represented colleges, and with various community organizations. SEARCH and the Four Directions Community Health Centre operate in a seamless manner; SEARCH acting as an extension of Clinic in-patient care, policies, advocacy and protocols. Student volunteers prepare and serve healthy snacks and drinks, provide child care for clients seeing the doctor or participating in adult programs, and in running the programs geared towards children and youth. Programming may include physical activity and nutrition training, anger management, healing from abuse, teenage pregnancy, literacy, and parenting. SEARCH monitors client feedback to current programs and frequently surveys their opinion for new programming ideas. Thank you for your very important contribution to SEARCH as a Mentor volunteer. In this student run wellness initiative, you play a critical role in both patient care and education. Therefore, it is very important for you to be aware of a number of important SEARCH policies in order to deliver a high level of consistency in the service provided for clients. These guidelines are provided to all SEARCH mentors and volunteers even though some of these policies apply to physicians only. All staff, mentors, and students should be aware of them. Should you have any concerns, new ideas or questions please do not hesitate to contact someone from SEARCH. Again, thank you for your participation. 4 Mission, Vision & Values of SEARCH Our Vision External Vision: “The North Central Community has achieved improved health and wellbeing through equitable, accessible programming delivered by an interdisciplinary collaborative of students and mentors” Internal Vision: “SEARCH students and mentors are leaders and champions of collaborative interdisciplinary approaches to professional practice.” Our Values SEARCH values are inclusive of the student mentoring process and the community we serve. They are our philosophical approach which guides all of our interaction and how we operate. Compassion - caring relationships built upon respect, empathy and active listening in an atmosphere of warmth and belonging. Continuous Learning - commitment to quality of life through ongoing development, improvement and evaluation of ourselves, our team and our services. Holistic view - supporting individuals, families and the community (physical, spiritual, emotional and mental) through an approach that is accepting, inclusive and honours the stories of others. Collaboration - working as a team in a respectful way where diverse ideas are shared, varied skills and perspectives are valued, and the contributions of all are recognized. Strength - our positive approach focuses on the strengths and assets of others, empowering them to make decisions as experts in their own lives. Our Mission SEARCH is a student run interdisciplinary primary health care initiative situated in the North Central Community in Regina. Our goal is to provide access to social and clinical programs in an after-hours, clinical setting with diverse populations. 5 Shift Information Orientation Each mentor will attend a mandatory orientation session prior to beginning work at SEARCH. When are shifts? SEARCH shifts are held on Saturdays (closed long weekends) from 12:00 to 4:00 at the Four Directions Community Health Centre, 3510 5th Avenue, Regina. How many people are on each shift? The shifts are comprised of the following personnel: Professionals – SEARCH Coordinator, physician mentor, 3 professional mentors Student Volunteers – A maximum of up to 16 students who participate in either social or clinical aspects of each shift. Outline of SEARCH Shift A SEARCH shift goes from 12:00 pm – 4:00 pm. Students and mentors arrive prior to the start of a shift around 12:00 pm. Proceed to the Gathering Room to put away any belongings and begin set-up preparations. All students will sign in on arrival in order to maintain a record of who is on-site during a particular shift; as well, please fill out a name tag at the beginning of the shift and wear it at all times. Before the clinic opens all of the volunteers will gather for a brief “opening circle. During this time everyone introduces themselves, the shift supervisor discusses any plans or activities for the day, and duties are assigned. Operational hours are 12:30 pm – 3:30 pm. At 12:30 pm the doors are unlocked and the clinic is open. The clinical team offers primary health care. The social team offers lunch and beverages, social programming, individual counselling, and childcare. Once a month, the regular social programming offered (with the exception of counselling) is replaced by Literacy Day activities. At 3:30 pm the doors are locked and the clinic is closed. Students tidy the appropriate areas and put away any supplies used during the shift. Once this is done, all volunteers and mentors gather for a mandatory “debrief session”. Everyone shares how the shift went for them. At the end of this session the shift is complete. 6 Teams and Social Programs Clinical Team – SEARCH offers medical services each Saturday to the clients who attend the clinic. These services can be for adults or children to see a doctor or a nurse for prescription refills, health inquiries, and any other needs of a client. Students on this team assist with the clinical needs of the clients within scope of practice based on level of schooling under the supervision of mentors. Social Team – SEARCH offers a variety of social programs and a hot meal. This team ensures a welcoming environment and provides social programs to clients of all ages. Kitchen duty – In charge of preparing and providing the meal and beverages to clients. Door Greeters – In charge of greeting clients, ensuring sign in, letting clients know what is on the agenda that day, and taking down stats. Childcare Room – In charge of engaging children/youth and running appropriate children’s programming. Social Programs: “What’s the Buzz” – A health awareness session that can be directed at children and adults, depending on the topic. Often a community partner or presenter is brought in to educate clients on a particular issue. Topics are usually chosen based on the interest of the clients as well as presenter availability. Examples of past topics covered include dental care, bullying, bike safety, and heart health. “Fun with Food” – A cooking program for clients of all ages. Clients can learn to cook quick, easy and healthy meals. The goal of this program is education on cost comparisons, healthier eating options, learning basic cooking skills, and health related concerns such as diabetes. Literacy Days – Focus on literacy skills through various family-friendly activities and teachings to promote literacy at the clinic in a way that reflects the cultures and traditions of the community. Community partners may come in to facilitate literacy activities. Students engage clients in activities and provide information on the importance of developing various literacy skills, such as reading, writing, and storytelling. Children’s Programming – Optional activities are provided for various age groups that focus on development of different skills, such as math, creativity, and literacy. Women’s Group – A therapy session or talking circle for women led by women. Topics can be planned in advance or chosen by the clients. This is led by a mentor and assisted by a student in their final years of study. Counselling – Individual counselling is provided on a drop-in basis in a private setting. This is facilitated by a mentor. A student further along in their studies may sit in on the session if permitted by client. 7 Policies All students and mentors are required to sign in - on the Sign-In Sheet provided - upon arrival for our records and for safety procedures in case of fire or accident. Mentor Registration: Mentors are required to be registered with a professional association in order to be credible in their field and ensure ethical standards are being upheld in each professional mentor’s practice. Proof of registration must be provided to SEARCH prior to attending a shift. Mentors and Paid Positions per Shift: Mentors and physicians have the responsibility to sign up using the online scheduling system to attend a shift at SEARCH. A maximum of 3 paid positions will be offered on a first come first serve basis and at there is to be only one paid physician per shift. It is not the shift coordinator’s role to assume that a mentor is attending a SEARCH shift. Mentor Honorariums: Only the first physician mentor to sign up online will be offered an honorarium per shift. Only the first three mentors of any other professional field to sign up online will be offered an honorarium per shift. If a mentor chooses not to take the honorarium it will be given to SEARCH in the form of a donation. Reference Checks: Upon showing interest in mentoring with SEARCH, mentors will be required to provide the Coordinator with an updated resume and three references. After satisfactory reference checks have been received, the Coordinator will approach the mentor to plan an orientation. Teaching Policy: In addition to serving clients and ensuring the highest quality of service delivery, all mentors play the important role of teachers and role models to student volunteers. The level of student involvement may vary from an observatory role to complete initial assessment with consultation from the mentor afterwards. This will depend on the student’s level of training as indicated by the appropriate Scope of Practice for that discipline. It may also depend on the comfort level of all three parties involved - client, mentor and student – as to the student’s level of assessment involvement. It is also a student’s responsibility to learn as much as possible from the mentors and staff available to you on any given shift. Inter-professional Policy: In addition to students training in the same discipline, all mentors are expected to engage and teach students from other disciplines. This interdisciplinary component is meant to introduce students to the activities of other disciplines, to develop an understanding of teamwork and for students to be able to apply this approach to their future professional practices. Students must be willing to work openly in this interdisciplinary atmosphere. It is also important that students learn how to make appropriate client referrals. 8 Personal Conduct Policy: Everyone working at SEARCH is expected to address any inappropriate behaviors to the attention of the Coordinator or shift supervisor. This includes any verbal and/or non-verbal violations of dignity, respect and self-worth of another; inappropriate mental or emotional behaviors; language and/or actions that results in humiliation, discomfort, that elicits fear, and/or takes unfair advantage of another, or creates an adverse or unacceptable environment. All SEARCH Students, Staff and Mentors agree to the following social contract: • To treat all clients equally and fairly. • To behave in a non-judgmental way. • To approach all clients with respect and compassion. • To act in a professional and ethical manner. Dress Code: SEARCH is a business casual workplace. Clothing that is ragged and/or stained, is revealing (cleavage, back, chest, stomach or underwear), and has words, terms, or pictures that may be offensive to other volunteers or clients is considered inappropriate. Also, because of potential fragrance sensitivities, please refrain from wearing scents. If clothing fails to meet these standards you will be asked to leave. We ask everyone to wear a SEARCH name tag at all times for identification purposes and to do so when you sign in each shift. Liability Insurance: You will need to provide all paperwork before working a SEARCH shift this is required for insurance purposes. All mentors provide proof of professional license liability insurance. SEARCH covers general liability should something happen to you while you are working a SEARCH shift. Orientation: An orientation session will take place with the Executive Director any time before attending a first SEARCH shift. Volunteer Numbers: In order for SEARCH to operate there needs to be a minimum of 8 volunteers signed up for a shift (this includes students and mentors). If there is less than that the shift will be cancelled for that week. There is a maximum of 20 volunteers allowed per shift (16 students and 4 mentors) and is determined on a first come first serve bases through the online scheduling system. Scheduling: SEARCH is only open on Saturdays (but not a Saturday that falls on a long weekend). As a volunteer it is your responsibility to schedule yourself, and then attend the shift you are scheduled for. If you have any problems with using the scheduling calendar, please email the SEARCH Coordinator. Safety Policy: For the safety of all SEARCH volunteers, safety protocols should be observed – When the clinic is not open the doors must remain locked and no one is allowed out of the building without shift supervisor permission; volunteers may carry their cell phones on their person during the shift (please use the device responsibly); there must be a minimum of two volunteers greeting clients; while operating during summer evenings a security guard will also be 9 at the front of the clinic; leave the building in pairs; no one travels home in anything but a vehicle (if this is not possible, the shift supervisor or the SEARCH Coordinator will make the appropriate arrangements). If a volunteer feels unsafe at any time during the shift, inform the shift supervisor or the SEARCH Coordinator. In the event of an emergency during a shift, call 911 immediately. If the duress alarm goes off during a shift, any one in a safe place has the responsibility to call 911. If possible, everyone else should try to get to a safe location. Feedback Policy: We depend on recommendations and feedback to make SEARCH a better place for everyone involved – clients, mentors, staff and students. For suggestions regarding our operation, please direct them to the shift supervisor, the SEARCH Coordinator, or a SEARCH board member. End of Clinic Policy: All mentors and students will participate in the reflection session at shift’s end. This is facilitated by the shift supervisor and held in the Gathering Room. Client Exam Room Policy: Except when changing into gowns, patients should not be left alone in an exam room for more than a few minutes. When this is necessary (e.g. when a student leaves the room to present to a mentor) the exam room door may be left open. Female clients may not be accompanied by a male in the exam room unless deemed appropriate by the clinical team. This is in the event a female chooses to disclose abuse. Private exams should be done with 2 people in the room (in addition to the client). A female chaperone must accompany the examining physician for any pelvic exams. When pelvic exams are done, please make sure the proper samples are obtained and that the appropriate measures for patient privacy are taken. All requisitions/forms should be filled out appropriately and be ready to be sent out. Charting Policy: With the patient’s first visit to SEARCH, we must inform them that SEARCH is a teaching clinic and that they will be seen by students. If they do not wish to be a part of the educational experience that is their choice. When a mentor, student or staff person sees a client for any reason, the encounter will be documented on the client’s chart. As all charts are the property of the Four Directions Community Health Centre we must adhere to the charting format used by the Clinic. The following formats are recommended DAP and SOAP: D – DATA Subjective and objective data about the client. Subjective – what the client can say or feel. Objective – observable/behavioural A – ASSESSMENT 10 What’s going on? Hypothesis, brief assessment of client’s current condition. P- PLAN Response or revision. What are you going to do? Treatment plan, lab work ordered, referrals made, follow up appointments. The SOAP Method - subjective, objective, assessment and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission note. Documenting patient encounters in the medical record is an integral part of practice workflow starting with patient appointment scheduling, to writing out notes, to medical billing. Pre-hospital care providers such as EMTs may use the same format to communicate patient information to Emergency department clinicians. It is mandatory for all notes made in a client’s chart to be signed by the mentor (note your discipline) and by the student/s and their discipline. The mentor must also ensure that the chart is signed by the student/s that saw the client. It is both the student and mentor’s responsibility to ensure all charts are signed properly. Patient Follow-up and Continuity of Care: To make SEARCH and Four Directions Community Health Centre operations as seamless as possible, patient follow-up is everyone’s responsibility. When lab work is ordered by SEARCH personnel, it is the responsibility of Four Directions staff to ensure that the lab work results, when received, are forwarded to either the client’s family physician or left for the physician at Four Directions. All referrals or charts needing follow-up will be left in a designated area to be dealt with by Four Directions the following business day. Seeing a Client Alone Vs. With A Second Person: In situations where a partner wants to be in the clinical room with the patient, the protocol is that we will first see the patient on their own. Together, in consult with the patient, clinical team, physician or mentor and the shift supervisor, the decision will be made as to whether the partner should join the client. In the event the client is being abused by the other person, seeing them together would not allow for either an accurate or truthful account of why they are seeking help nor disclosure to the clinical team about the abuse which would preclude the offer of help. Prescription Policy: No new psychiatric drugs will be prescribed. Narcotics, benzodiazepines/ tranquilizers are not prescribed unless they are restricted to short term use for acute illness or acute pain management, or long term use such as Palliative Care. If the physician believes that a patient requires a narcotic immediately, SEARCH will pay for the transportation of that individual to the Emergency. As there are a number of places in the area where illegal drugs are sold no narcotics are kept on the premises, nor will they be allowed in the Clinic. Distribution of Condoms Policy: Clients may request free condoms. Anyone may distribute them as records are not kept. Please ask another mentor, physician, or the shift 11 supervisor if you have questions about how to give information about the use of condoms to clients. Reproductive Policy: SEARCH supports a woman’s choice to have an abortion and is in favour of full accessibility and completely funded abortion services as a matter to be resolved between a woman and her physician. SEARCH staff will aid women fully in their reproductive choices including abortion. SEARCH recognizes unplanned pregnancy is a delicate and controversial subject. For the protection of both clients and students, it is SEARCH policy that no student will enter into discussion of this matter with clients without supervision and client permission. Any client who presents with a possible unplanned pregnancy will be referred to the physician. Chest Pain, Difficulty Breathing, Heavy Bleeding: These situations, or any other extreme health issue, they are very serious; therefore, the patient is to see the physician immediately and the physician will determine what action is to be taken. Mentor in Women’s Group: A qualified mentor must be present in order for women’s group to operate. If a mentor is not present to run women’s group, it will be cancelled for that shift. Under no circumstances can a student run this session alone as difficult discussion topics may arise. Individual Counseling Policy: Counseling will be offered to individuals who are 18 years of age or older on a drop-in basis. An appropriate mentor must always be present during a session. Only one student in a higher level of their education will be allowed to sit in on a session. Each session can be up to 50 minutes long and will be conducted in a private setting, allowing for ample time to teach, chart, and debrief. Referrals will be made to other organizations if necessary. People Under the Influence: People who are under the influence will be provided clinical services as long as that individual is not behaving in an intrusive or offensive manner to other clients or volunteers. If the person becomes disruptive the shift supervisor will ask that client to leave, or call the police as needed by dialing (9)911. Suicide Ideation: If suicide is mentioned at all during a shift the patient goes directly to the physician as this needs immediate attention and the client is in need of further assessment. This is also a liability issue for the physician and potentially SEARCH, therefore it is imperative that the physician be involved in making an assessment. Child Abuse Disclosure Policy: If a child discloses ANY type of abuse to you at ANY time, it is your responsibility BY LAW to ensure that it is reported to Mobile Crisis or the Ministry of Social Services. Within the realm of SEARCH, you will need to listen to the child, DO NOT ASK QUESTIONS, reassure the child and believe the child. Do Not Over React. Without alarming the child, get immediate assistance from a mentor or physician. Do not let the child leave the clinic until the physician has been made aware of the situation. 12 Mobile Crisis 757-0127 or 569-2724 Child Protection Emergency 787-3760 Family Services 787-3800 Kids Help Phone 1-800-668-6868 13 WHAT TO DO IF A CHILD DISCLOSES ABUSE When a child tells you they have been abused, the child may be feeling scared, guilty, ashamed, angry and powerless. You, in turn, may feel a sense of outrage, disgust, sadness, anger and sometimes disbelief. It is important for you to remain calm and in control of your feelings in order to reassure the child that something will be done to keep him or her safe. The child's feelings about themselves may be influenced by your initial reaction to the abuse. You can show your care and concern for the child by: Listening to the child. Controlling expressions of panic and/or shock. Expressing your belief that the child is telling the truth. Using the child's language or vocabulary. Telling the child that this has happened to other children, and they are not the only one. Reassuring the child that to disclose is the right thing to do. Emphasizing that whatever happened was not the child's fault, and the child is not bad. Telling the child that you know some adults do wrong things. Acknowledging that it is difficult to talk about such things. Letting the child know you will make a report to the appropriate authorities so they can help stop the abuse. Telling the child you are pleased they told you. If you suspect abuse, but the child has not told anyone, be aware of the emotional distress that the child may be experiencing. Approach the child in a caring and sensitive manner and assure them that you are willing to listen and to help if there is a problem. You will not be helping the child if you: Make promises you cannot keep, such as promising that you will not tell anyone. Push the child into giving details of the abuse. Your role is to listen to what the child wants to tell you and not to conduct an investigation (beware of asking any direct questions of the child as this may prejudice any subsequent investigation). Indiscriminately discuss the circumstances of the child with others not directly involved in helping the child. The child may get angry and may displace his/her anger on you by shouting or swearing at you or attempting to strike you. Don't take this personally, even if the attack seems very personal. He/she needs someone to vent his/her anger on, and because you're there and you're safe, he/she will choose you. Continue to treat the child with caring, understanding and kindness. Don't berate the child for his/her situation and don't dwell on things that are beyond his/her control "you shouldn't have let him do it,” "you should have told me (earlier)," "you shouldn't have been playing there anyway." Keep in mind that what/how you say may make the child feel guilty and responsible for the assault, and children are not powerful enough to prevent adults from abusing them (kids are expected to do what adults tell them to do). The child can't change what's already happened. 14 Don't dwell on the sexual aspects of the assault. Offer unconditional, non-judgmental support. Acceptance will help the child overcome feelings of loneliness, of being "dirty" or of being "unworthy" of being cared for. Let the child decide when or if he/she wants to talk about his/her feelings about the assault. Reinforce his/her feelings, help him/her to know that it is okay to feel that way, and emphasize that he/she is in no way responsible for what happened. Mostly, just listen and REMEMBER THAT YOU ARE NOT IN THIS ALONE! REFERENCES South Eastern CASA. (2011). What to do if a child discloses to you. Retrieved from http://www.secasa.com.au/articles/tag/child-sexual-abuse. Victims of Violence (2008). Retrieved from http://www.victimsofviolence.on.ca/rev2/. 15 Code of Ethics Key Points to Guide our Actions Create a positive environment with respect to attitude. Protect and enhance your own health and wellbeing by identifying those stress factors in your professional and personal lives that can be managed by developing and practicing appropriate coping strategies. Treat your colleagues with dignity and as persons worthy of respect. Recognize your limitations and recommend additional opinions and services to be sought if needed. Recognize the profession's responsibility to society in matters relating to public health, health education, environmental protection, legislation affecting the health or well-being of the community and the need for testimony at judicial proceedings. Seek help from colleagues and appropriately qualified professionals for personal problems that might adversely affect your service to patients, society or the profession. At the center of our actions should be a holistic approach to the patient’s well-being. Treat all patients with respect; do not discriminate against any patient on such grounds as age, gender, marital status, medical condition, national or ethnic origin, physical or mental disability, political affiliation, race, religion, sexual orientation, or socioeconomic status. Make every reasonable effort to communicate with your patients in such a way that information exchanged is understood. Recognize, disclose and resolve conflicts of interest in the best interest of patients; Do not exploit patients for personal advantage. Take all reasonable steps to prevent harm to patients; should harm occur, disclose this information to the patient. Promote equitable access to health care resources. Use health care resources prudently. Provide the appropriate care of patient to include physical, psychosocial, and spiritual aspects, recognizing that community, society and the environment are important factors in the health of individual patients. Provide your patients with the information they need to make informed decisions about their medical care, and answer their questions to the best of your ability. Respect patient autonomy by respecting the right of a competent patient to accept or reject any medical care recommended. Provide whatever appropriate assistance you can to any person with an urgent need for medical care. Recommend only those diagnostic and therapeutic services that you consider to be beneficial to your patient or to others. Protect the personal health information of your patients. Disclose your patients' personal health information to third parties only with their consent, or as provided for by law, such as when the maintenance of confidentiality would result in a significant risk of substantial harm to others or, in the case of incompetent patients, to the patients themselves. In such cases take all reasonable steps to inform the patients that the usual requirements for confidentiality will be breached. 16 Professionalism Ensure honesty with patients and with SEARCH Board/Staff. Patients deserve the information needed for making informed, autonomous decisions. It is also our responsibility to acknowledge any medical errors that could occur in health care. Be honest about our own limits and recognize when it is necessary to seek outside help and/or guidance. Maintain patient confidentiality. Maintain appropriate relationship with patients; one must not exploit a relationship for sexual or emotional purposes, financial gain, or any other self-serving reason. Create and uphold well-defined firm boundaries. Improve the quality of care by continuously learning and collaborating with colleagues to address where downfalls are occurring. Improve access to care and justly distribute finite resources by maintaining a state of equality and having no tolerance for discriminative attitudes in making health care decisions. Acquire informed consent from a patient before implementing a treatment. Keep in mind the capacity of your patient and maintain an environment that allows for one to volunteer for treatment, not be forced into one. 17 Code of Conduct (as a Mentor of SEARCH) I will adhere to the principles of democracy; I will be honest about my motives and not subscribe to hidden agendas. I will air my concerns and opinions openly in the appropriate forum. I will not act upon personal grudges. I will consider the issues, not the personalities. I will evaluate someone’s opinion based on merit, not who proposes it. I will accept diversity. I will understand of others’ concerns and priorities, even if they are not my own. I will be appreciative of volunteer effort. I will be tolerant of volunteer mistakes and won’t hold volunteers to standards they cannot be expected to meet. I will use available continuing education to help volunteers and others improve their understanding of a co-operative’s functioning. I will avoid factionalism. I will support consensus making and the resulting decisions. I will make its resolution a priority when a conflict arises. I will ask the help of trained, experienced people when necessary. I will participate not just because SEARCH needs me but because I need to feel a part of it in order to be an effective member. 18 Social Determinants of Health A health care system – even the best health care system in the world – will be only one of the ingredients that determine whether your life will be long or short, healthy or sick, full of fulfillment, or empty with despair. -The Honourable Roy Romanow, 2004 The primary factors in shaping the health of Canadians are the social determinants of health – the living conditions that one experiences. General socioeconomic, cultural and environmental conditions, social and community networks, as well as individual lifestyle factors all have an immense impact on our wellbeing. Canadians are largely unaware that our health is shaped by how income and wealth is distributed, whether or not we are employed, and if so, the working conditions we experience. Furthermore, our wellbeing is also determined by the health and social services we receive, and our ability to obtain quality education, food and housing, among other factors. And contrary to the assumption that Canadians have personal control over these factors, in most cases these living conditions are – for better or worse – imposed upon us by the quality of the communities, housing situations, our work settings, health and social service agencies, and educational institutions with which we interact. Research is also finding that the quality of these health-shaping living conditions is strongly determined by decisions that governments make in a range of different public policy domains. The 14 social determinants of health include: Aboriginal Status Disability Early Life Education Race Food Security Health Services Gender Housing Income and Income Distribution Social Exclusion Employment and Working Conditions Social Safety Net Unemployment and Job Security More information can be found at www.thecanadianfacts.org. REFERENCES Mikkonen, J., & Raphael D. Social determinants of health: The Canadian facts. University of Toronto: York School of Health Policy and Management. 2010. 19 Cultural and Community Competencies Where does SEARCH fit into the community context? Sensitivity Issues Within the core neighbourhoods of Regina, there are many different health issues faced by different people coming from different economic and cultural backgrounds. As a volunteer it is important that you are aware of these differences and that you use this awareness to act appropriately with the people you will be serving. Economic Status Some members of the core communities have very low annual incomes and as such may be sensitive about certain issues and may be more prone to certain health conditions. For example, people with low incomes may not want to make appointments to see another doctor because they may not be able to pay for the medications or they may not have a Health Card because they do not have a permanent address. Un- or under- employed people are more likely to suffer from deprivation in particular areas of health determinants – food security, housing or social and are therefore more prone to deprivation related health concerns (Stronks et. al., 1998). Deprivation related health concerns could include but not be limited to poor nutrition, psychological stress, disease and/or substance use. It is important to understand the client’s situation so that you can offer realistic treatments and recommendations. Cultural Sensitivity The population of Canada is truly multicultural as immigrant populations continue to rise (Shah and Zakus, 2004). People from different cultures may have circumstances that make them more prone to certain health conditions. In some instances there may be a language barrier during the assessment which may require a translator and may cause stress for the patient. It is possible that with this third individual present the patient will not speak frankly about their condition. Brochures and written information, including health campaigns, may not be well understood by all people (Shah and Zakus, 2004). A language barrier can result in miscommunication and your language may need to be graded or you may need to speak more slowly. It is possible that alternative medical practices are part of a patient’s culture and should be respected. The roles and status of people within a family/kin group may be different from those with which you are familiar and may impact the health status of the patient (Shah and Zakus, 2004). For example, an older family member may be the primary caregiver of the children and so may spend their days running after small children. The patient may have religious or cultural beliefs, which you will need to take into consideration when making recommendations for treatment. Some ethnic groups are more prone to certain health conditions. For example, many people become lactose intolerant in adulthood and genetic diseases can be more common in one group than another (ex: cystic fibrosis or sickle cell anemia). Also newly arrived immigrants may not come with medical records or have a regular doctor (Talbot et al, 2001). Once again the 20 situation of the patient must be understood so that you can offer realistic treatments and recommendations. Aboriginal Culture According to the 2001 Census, Regina has one of the highest Aboriginal populations of any major Canadian city. The five primary First Nations groups in Saskatchewan are Cree, Dene, Saulteaux, Assiniboine and Dakota and each has its own distinct beliefs, systems and language. First Nations people have a culture that is based on respect. There is a strong belief in spirituality, traditions, and ceremonies. Many ceremonies are practiced regularly (i.e. a pipe or sweet grass ceremony) and spirituality plays a role in the everyday life of many Aboriginal people. Elders within the community are people who are actively involved in their culture and who have knowledge of their culture and traditions. Elders act as advisers in the community and offer wisdom and act respectfully to others. Kin groups are very large which means that there is often very close contact between members of an extended family i.e. cousins may be treated more as siblings. According to the Medical Services Act some medical services are applicable to the different terminology listed below. Aboriginal People refers to Indian, Metis and Inuit peoples of Canada. Treaty Indian is a person who has an ancestor who signed a treaty. Status or Registered Indian is someone registered as an Indian with the federal government’s Indian Register. Native is a term used for an Indian person. First Nations is a term used to identify an Indian person and most preferred by Indian people themselves. Métis is a person of Native and European decent. What is cultural competence? Cultural competence is defined as the "provision of health care that responds effectively to the needs of patients and their families, recognizing the racial, cultural, linguistic, educational and socio-economic backgrounds within the community." (Masi, 2000) It is “a set of congruent behaviors, attitudes, and policies that come together in a system, agency, or among professionals and enables that system, agency, or those professionals to work effectively in cross-cultural situations.” (Cross, Bazron, Dennis, & Isaacs, 1989) It can be operationally defined as “the integration and transformation of knowledge about individuals and groups of people into specific standards, policies, practices, and attitudes used in appropriate cultural settings to increase the quality of health care; thereby producing better health outcomes.” (Davis, 1997, as cited in Cross, Bazron, Dennis, & Isaacs, 1989) Cultural Competence refers to the relationship between the “helper” and the person being “helped” in a cross-cultural context. It focuses on the capacity of the health worker to improve health status by integrating culture into the clinical context and acts as a vehicle for increasing access to quality care for all patient populations, by tailoring health care delivery to meet patients’ social, cultural, and linguistic needs (King, Sims and Osher). 21 What is Cultural Safety? Cultural Safety focuses on the experience of the patient - it is based on the experience of the recipient of care, rather than from the perspective of the medical practitioner. It accepts the legitimacy of difference and diversity in human behavior and social structure. Cultural Safety, in practice, involves the effective care of a person or family from another culture by a medical practitioner who has undergone a process of reflection on their own cultural identity and recognizes the impact their culture has on their own medical practice. It recognizes that the attitudes and beliefs, policies and practices of medical practitioners can act as barriers to service access, and is concerned with quality improvement in service delivery and consumer rights Why exercise Cultural competency? to maximize gains from a health intervention where the parties are from different cultures (Mason, 2001); to increase access to quality care for all patient populations, by tailoring delivery to meet patients’ social, cultural, and linguistic needs (King, Sims and Osher); to increase the closeness between practitioner and patient in terms of understanding and mutual respect so as to increase the client's access to the best possible care, and to bridge the gap between practitioner and clients. How does one become a culturally competent individual? One has to know oneself to be culturally competent: an individual must undergo a process of reflection on their own cultural identity and recognize the impact their culture has on their own medical practice; One must understand the term culture and its place in a health care setting; One must be sensitive to the cultural issues of each individual client, and One must comprehend and have the capacity to utilize specific methods to deal with cultural issues (American Association of Medical Colleges, 2000). Why is communication essential in to the exercise of cultural competence? Cultural competence is an important aspect of communication, and communication a crucial element in achieving the delivery of high quality, appropriate health care. When information has been successfully communicated by the client and understood by the health care provider, there is greater likelihood that the client will be able to access and receive the appropriate care. How can SEARCH members be culturally competent in their interactions with the community they serve? When interacting with community members it is crucial to realize that culture can influence communication in many ways - from language used and emotional responses, to eye contact and touching. We must understand that: Culture encompasses many elements such as beliefs, attitudes, values, verbal communication and non-verbal communication. 22 Culture may be influenced by a number of factors such as location, race, ethnicity, religion and socio-economic status. Equally important influencers of culture are factors such as disability or sexual orientation: o For instance, the hearing impaired have a unique culture, in that they possess their own language with non-verbal cues, which are specific to that group o Gay, lesbian, bi-sexual and two-spirit individuals are another example of a population that must be treated with cultural competence. REFERENCES Cross T., Bazron, B., Dennis, K., & Isaacs, M. (1989). Towards a culturally competent system of care, volume I. Washington, D.C.: Georgetown University Child Development Center, CASSP Technical Assistance Center. Durie, M., (2001). Cultural competence and medical practice in New Zealand. Australian and New Zealand Boards and Council Conference. Wellington, New Zealand. Health Canada (2001). Certain circumstances: equity in and responsiveness of the health care system to the needs of minority and marginalized people. Retrieved from http://www.hc-sc.gc.ca/hcssss/alt_formats/hpb-dgps/pdf/pubs/2001-certain-equit-acces/2001-certain-equit-acces-eng.pdf. Isaacs, M., Benjamin, M. (1991). Towards a culturally competent system of care, volume II, programs which utilize culturally competent principles. Washington, D.C.: Georgetown University Child Development Center, CASSP Technical Assistance Center. King, M. A., Sims, A., & Osher, D. (2001). How is cultural competence integrated in education. Centre for Effective Collaboration and Practice. American Institutes for Research. Shah, A., Zakus, D. (2004). The future of healthcare in canada: diagnosing the needs of immigrants. University of Toronto Medical Journal. 82 (1). Stronks, K., van de Mheen, H. D., Mackenbach, J. P. (1998). A higher prevalence of health problems in low income groups: does it reflect relative deprivation? Journal of Epidemiology and Community Health, 52, 548-557. Talbot, Y., Fuller-Thomson, E., Tudiver, F., Habib, Y., McIsaac, W. J. (2001). Canadians without regular medical doctors: who are they?. Can Fam Physician, 47, 58-64. 23 Policy on Confidentiality of Patient/Client Information (For the following and more detailed information about HIPA see http://www.health.gov.sk.ca/health-information-protection-act) Mental and physical health information and all matters relating to the care of clients and patients are private and confidential. Personal health information will be defined according to the Saskatchewan Health Information Protection Act (HIPA) 1. Definitions: 1.1 “Personal health information” means, with respect to an individual, whether living or deceased: 1.1.1 information with respect to the physical or mental health of the individual; 1.1.2 information with respect to any health service provided to the individual; 1.1.3 information with respect to any body part or bodily substance of the individual including those donated by the individual; 1.1.4 information collected in the course of, or incidentally to, providing health services to the individual; 1.1.5 registration information. 1.2 “Record” means a record of personal health information in any form and includes information that is written, photographed, recorded, digitized or stored in any manner. 1.3 “Trustee” is defined as SEARCH INC. in the context of this policy. SEARCH Inc. is the trustee of all personal health information collected in the course of, or incidental to, providing health services to an individual. 2. Overall Principles 2.1 SEARCH Inc. shall respect the privacy of each patient/client and shall ensure that all his/her personal health information is treated confidentially. 2.2 This policy applies to all students, mentors, employees, and all others involved with the operation of SEARCH Inc. 2.3 SEARCH Inc. shall treat personal health information in accordance with all applicable legislation. 3. Duty to Preserve Confidentiality 3.1 Personal health information shall be used or disclosed only for the purpose which it was collected; or for a reason consistent with that purpose; or in accordance with HIPA. 3.2 Personal health information shall be available only to those persons who need the information in order to provide care to the patient/client, with the provision that the information will be used for the benefit of the individual. 3.3 Any person who has legitimate access to personal health information shall preserve the confidentiality of the information and shall be accountable for its preservation. 3.4 Any person who inadvertently has access to personal health information in the course of their duties in SEARCH Inc. shall preserve the confidentiality of the information and shall be accountable for its preservation. 3.5 Breach of confidentiality or this Policy may result in disciplinary action. 4. Ownership of the Record 4.1 The record in which the personal health information is stored is owned by Four Directions Community Health Centre. 24 4.2 SEARCH Inc. has an obligation to the individual patient/client to preserve the confidentiality of the personal health information contained in the record. 4.3 SEARCH Inc. has an obligation to take reasonable steps to ensure that all records are accurate and complete. 4.4 SEARCH Inc. has an obligation to protect the integrity and accuracy of the record from any unauthorized access, use, disclosure, or alteration. SEARCH Inc. has further obligation to maintain the integrity of the records it holds in accordance with legislation. 5. Consent Requirements (SEARCH will provide clients with patient consent form before any assessment or treatment) 5.1 The patient/client is entitled to all relevant information needed to give consent to the collection, use or disclosure of his/her personal health information. 5.2 Consent shall be voluntary and informed. 5.3 Consent may be either written or verbal. A permanent record of verbal consent is advised. 5.4 Consent may be implied if it is reasonable to suppose that: 5.4.1 By his/her actions, the individual has agreed to the collection and use of his/her personal health information. 5.4.2 The individual would consent to the disclosure of the personal health information in order to receive necessary health services. 5.4.3 No barriers exist to the disclosure of personal health information to immediate family members or other persons with whom the individual has a special relationship. 6. Collection, Use and Disclosure 6.1 Collection 6.1.1 The individual shall be informed of the purpose for which the personal health information is being collected. 6.1.2 The individual shall have the right to withhold information unless withholding the information contravenes a statutory obligation to provide it. 6.2 Use 6.2.1 Personal health information shall be used only for the purpose for which it was collected. 6.2.2 Explicit consent of the individual must be obtained if any other use of the personal health information is proposed. 6.2.3 De-identified personal health information may be used without explicit consent for statistical or demographic purposes, planning or evaluating the provision of health services and/or approved research. 6.2.4 As required by law, personal health information may be used to protect public safety in terms of infectious disease reporting or abuse of children. 6.3 Disclosure 6.3.1 Disclosure of personal health information to a third party requires consent, unless excepted by HIPA. Only authorized and informed personnel can disclose personal health information to a third party. 6.3.2 Care-providers involved in the planning or provision of care services may have access to the health information of a patient/client on a “need to know” basis for the purposes 25 of on-going care or for the evaluation of the health services provided. Identification and authorization will be required. 7. Failure to Comply 7.1 Failure to comply with this policy or failure to preserve the confidentiality of personal health information in accordance with relevant legislation shall be a matter of investigation. 7.2 Penalties imposed for failure to comply with the policy shall be determined on a case by case basis by the Executive Council Members of SEARCH Inc. Sources: 1.1 Health Information Protection Act (HIPA) 2m 1.2 HIPA 2p 1.3 HIPA 2t 2 District Health Policies & Procedures Confidentiality–Health Information (7311-75003) 1.2 3 HIPA IV 23 – excluding Section 3.5 – is Section 3.5 needed or is this covered by Section 7 4.1 Needs to be changed/removed 4.2 HIPA III 16 4.3 HIPA III19 4.4 HIPA III16 5 Sections 5.1-5.4 – HIPA II 6 subsection 1-5 5.4 All Subsections of section 5.4 are from SDH Policy (above) 1.5.4.1-3 6.1 HIPA IV 6.2 HIPA IV 26, 27 6.3 HIPA IV 27 7. SDH policy (above) 1.7 26 The “How-to” for Online Self-scheduling 1) Link to online website: http://www.supersaas.com/schedule/reginastudentclinic/Shift_Schedule 2) Log-in using the following information: a. Account Name: SEARCH Password: REGINA 3) You will sign up on the Shift Schedule calendar for the shift you are available to attend. 4) On the screen you will see a calendar in the upper right hand corner. You can scroll through the different months using the arrows next to the month title. The dates that have an event scheduled will be highlighted in colour. 5) To schedule yourself for a shift: a. Click on the desired date on the calendar in the upper right hand corner. Below the calendar in the upper right hand corner, highlighted in blue, you will see an agenda for the shift for the date that you have chosen. b. Click on the highlighted blue section of the daily agenda found just below the calendar in the upper right hand corner. A white window will show up. In this window you will see the names and category/discipline of those who have signed up for the event/shift thus far. Below the names of those who have signed up, you will find two options to choose from: i. New Booking – choose this option if you would like to sign up for the event/shift on that date ii. Close – choose this option if you are on the wrong date and would like to close out of this window. c. After clicking on the New Booking option, another white window will appear. Please provide us with the following information: i. Full Name ii. Email address iii. Phone number iv. Category/Mentor and Discipline 1. e.g. category A, education student 2. e.g. mentor, social work v. Social/Clinical team 1. e.g. social team 2. e.g. clinical team d. After filling in the above information, you will have the option of signing yourself up for additional events/shifts that you already know you would like to volunteer for. Next to the word Repeat, there is a button that you can hit “…” After hitting this button, all dates in which events/shifts are currently scheduled for will show up. You can then proceed to check off any of those dates that you would like to volunteer for. By choosing this option, you will not be required to fill out the above information (i.e. full name, email, etc) multiple times. e. Hit “Create Booking” button at bottom of the window to sign yourself up. 6) You will then be able to click on the highlighted blue agenda for that date and see that you have signed up for that event/shift. 27 7) You will receive an email shortly confirming that you have signed yourself up for the event/shift. Two days prior to the event/shift, you will also receive a reminder email. 8) If you have to cancel an event/shift that you have signed up for you must email the coordinator to cancel at reginastudentclinic@gmail.com. If you have any issues signing up please contact the coordinator at the above email address. 28 Appendix – D Emergency Procedures For Building Emergencies: Call Pasqua Security 306-766-2900, tell them your name, that you work for SEARCH at the Four Directions Community Health Center on Saturday/Monday. Let them know what you are requesting. Duress Buttons: Duress buttons are located in each room at Four Directions. These only sound within the building, they do not automatically dial anyone. If one is triggered, make sure everyone is safe. Call 911 or Pasqua Security if necessary. Disarm in the mail room, behind front desk. Fire Escape Plan: 1. Anyone discovering a fire is to sound the alarm by calling “Code Red”. 2. Receptionist is to call the fire department by calling 9-9-1-1 3. Receptionist to take staff list and begin orderly evacuation through main entrance The following areas will evacuate through the main entrance: -Childcare room -CHC rooms -Public washrooms -Sage room -Front waiting rooms -Front desk reception area -Gathering room -Addictions Services office -Counselling room -CLW Office -SLP office The following areas will evacuate through the staff entrance (east side of building): -Staff room -Caretaker room -Resource room off Gathering room -Staff washrooms -Staff work area -Supervisors office 29 The following areas will evacuate through the rear entrance: -Vaccine room -Primary Care reception -Primary Care exam rooms -Primary Care Practitioner office -CCNE office -Rear washrooms 4. If the hazard is located near one of the entrances/exits, all personnel will evacuate through a clear remaining exit. NOTE: ALL CLIENTS ARE TO BE EVACUATED WITH STAFF 5. THE MARSHALLING AREA FOR ALL STAFF IS THE STAFF PARKING LOT ON THE SOUTH SIDE OF THE BUILDING OR CONEXUS 6. At the marshalling area the Fire Marshall will begin roll call for all staff 7. Upon arrival of the Responding Agency, the Fire Marshall is responsible for informing them: -If all employees are accounted for -If any personnel remain in the building, the location and the problem -The exact location of the hazard, if known Safety Policy: For the safety of all SEARCH volunteers, safety protocols should be observed – When the clinic is not open the doors must remain locked and no one is allowed in or out of the building without shift supervisor permission; volunteers may carry their cell phones on their person during the shift (please use the device responsibly); there must be a minimum of two volunteers greeting clients; while operating during summer evenings a security guard will also be at the front of the clinic; leave the building in pairs; no one travels home in anything but a vehicle (if this is not possible, the shift supervisor or SEARCH Coordinator will make the appropriate arrangements). If a volunteer feels unsafe at any time during the shift, inform the shift supervisor or SEARCH Coordinator. In the event of an emergency during a shift, call 911 immediately. If the duress alarm goes off during a shift, any one in a safe place has the responsibility to call 911. If possible, everyone else should try to get to a safe location. WHMIS: Use the WHMIS binder in the med storage room located on wall beside door (in clinic) or beside janitor room. Evacuate the building and call Fire Department/911. 30 First Aid Kits: See the clinic for needed supplies in the event a first aid kit is needed. See physician on duty to assess the situation. If other medical assistance is required, call 911. Prohibited/Restricted Areas: No clients are allowed in the back offices of Four Directions Community Health Center. This includes all areas behind the breastfeeding room. Alarm Issues: If the alarm is set off throughout the shift, first try to disarm it with the code. If this does not work, call Pasqua Security, 306-766-2900. 31