INTRODUCTION TO SCIENTIFIC RESEARCH
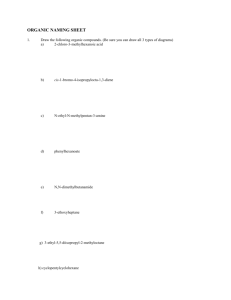
advertisement

LOCAL ANESTHETICS Local Anesthetics Historically the first local anesthetic discovered was the tropane alkaloid cocaine: Cocaine is still used in ocular surgery (anesthetic) and nasal/sinus surgery to decrease post-operative bleeding due to its vasoconstrictive properties----cocaine addicts Readily absorbed from the mucous membranes with good local activity - Rapidly hydrolyzed and inactivated due to the presence of two ester groups Addiction includes both physical and psychological addiction Desirable Properties of Local Anesthetics 1) Reversible 2) Non-irritating to the tissues 3) Rapid onset of acting 4) Long duration of acting 5) High therapeutic index 6) Effective topically and by injection 7) Proper physical properties solubility and stability in solution) (water LOCAL ANESTHETICS CHEMISTRY •It composed of hydrophilic domain • Which either tertiary or secondary amine • and hydrophobic domain • it aromatic residue • separated by alkyl chain • The hydrophobic & hydrophilic domains linked with either ester or amide • This bonds determine the pharmacology of L.A. ANESTHETICS Pharmacological Classes of Local anesthetic a- Amide 1- Lidocaine (lignocaine) Risk B & C 2- Prilocaine Risk B & C 3- Bupivacaine (Marcain) Risk C 4- Ropivacaine (Naropin) Risk C 5- Dibucaine Risk C 6- Mepivacaine ( Scandonest or Carbocaine) Risk C 7- Etidocaine (Dranest) Risk B Pharmacological Classes of Local anesthetic B- Ester 1- Tetracaine (Amethocaine) Risk C 2- Benzocaine Risk C 3- Cocaine Risk C & X 4- Proparacaine (Fluoracaine) Risk C 5- Procaine Risk C 6- Chloroprocaine Risk C Pharmacological Classes of Local anesthetic C- Miscellaneous 1- Dyclonine (ketone) Risk C 2- Pramoxine (ether) MECHANISM OF ACTION * Block initiation & propagation of action potential * By preventing the voltage-Dependent increase in sodium conduction * Via physical plugging the transmembrane pore * The binding site is in the inner end of sodium channel SEQUENCE OF EVENTS WHICH RESULT IN CONDUCTION BLOCKADE 1. Diffusion of the base form across the across the nerve sheath and nerve membrane 2. Re-equilibration between the base and cationic forms in the axoplasm 3. Penetration of the cation into and attachment to a receptor site within the sodium channel. 4. Blockade of the sodium channel SEQUENCE OF EVENTS WHICH RESULT IN CONDUCTION BLOCKADE 5. Inhibition of sodium conduction 6. Decrease in the rate and degree of the depolarization phase of the action potential 7. Failure to achieve the threshold potential 8. Lack of development of a propagated action potential 9. Blockade of impulse conduction CONDUCTION OF A NERVE IMPULSE Ionized Common features of Local Anesthetics • Weak bases (pKa > 7.4) [poorly water soluble] • Packaged as an acidic hydrochloride [pH 4-7 now soluble] • In solution- non-ionized lipid soluble (free base) AND ionized water soluble (cation) • Body buffers raise the pH, increase free base • lipid soluble form crosses axonal membrane • water soluble form blocks sodium channel Important Clinical Properties of Local Anesthetics • ONSET • POTENCY • DURATION OF ACTION Important Clinical Properties of Local Anesthetics • ONSET = pKa • pKa = pH at which 50% of drug is ionized • LA’s <50% exists in the lipid soluble nonionized form • Only the nonionized form crosses into the nerve cell ROLE of pH and pKa in LOCAL ANESTHETICS Important Clinical Properties of Local Anesthetics Speed of Onset • low pKa = fast onset • Bupivacaine 8.1 Lidocaine 7.7 • ? LA action in septic tissue – acid tissue -> é ionized % of LA -> slow entry into membrane -> low concentration of LA for block Important Clinical Properties of Local Anesthetics Anesthetic Potency • Potency <=> lipid solubility • Higher solubility <=> can use a lower concentration and reduce potential for toxicity [LA] Important Clinical Properties of Local Anesthetics DURATION OF ACTION Duration <=> protein binding • Bupivacaine 95% • Lidocaine 65% • Procaine 6% Important Clinical Properties of Local Anesthetics CLEARANCE • ESTERS hydrolysis via pseudocholinesterase • AMIDES metabolism via hepatic enzymes Important Clinical Properties of Local Anesthetics Absorption of local at site • LA’s cause some vasodilitation • LA washout related to blood flow • LA toxicity related to rate of absorption via blood flow Important Clinical Properties of LA’s ADDITION of VASOCONSTRICTORS 1- Why it is combined with L.A. ? • Vasoconstriction <=> slows systemic absorption & increases duration 2- Epinephrine is commonly used in 1 in 200000 to 80000 (5ug-12.5ug/ml) • Least effective with high lipid soluble LA’s (bupivacaine/etidocaine) • Epi may produce distal and systemic effects ADDITION of VASOCONSTRICTORS 3- The total dose should not exceed 200-500ug 4- Epi-Drugs interaction •Tricyclic anti-depressant • Sympatholytic drugs 5- Contraindications ? -not recommend for digits injection 6- Do you prefere Norepinephrine OR EPINEPHRINE? Effect of pH on the efficacy of local anesthetics 1- The activity of local anesthetic is strongly pH dependent 2- L.A. need to penetrate the nerve sheath and axon to reach the binding site of sodium channel 3- In acidic media penetration is very poor 7- Inflammed & infected tissues are acidic ADDITION of Sodium Bicarbonate •NaHCO3 - é pH & nonionized base •Speeds onset of block •1 mEq NaHCO3 per 10 ml Lido/Mepiv •.1 mEq NaHCO3 per 10 ml Bupiv Methods of administration of L.A. 1- Infilteration Lidocaine or Bupivacaine 2- Surface Lidocaine, tetracaine, benzocaine 3- Intravenous regional anesthesia prilocaine 4- Nerve block mainly lidocaine , lidocaine or bupivacaine 5- Spinal anesthesia mainly lidocaine , tetracaine 6- Epidural anesthesia mainly lidocaine , marcain A. Surface or Topical Anesthesia 1. The oral cavity, pharynx, larynx and tracheobronchial tree provide examples of mucosal surfaces where local anesthetics are applied topically. 2. A great danger exists in these areas for overdosage since rapid absorption into the circulatory system may occur and exceed the rate of detoxification of the drug. 3. To avoid this danger use a fine spray with a low concentration of the drug and limit the volume of solution used. 4. Most often used agents cocaine (4-10%), tetracaine (1-2%) and lidocaine (2-4%) B. Local Infiltration 1. Used for superficial surgery such as removal of moles, warts, sebaceous cysts, etc. Also for iv insertion. 2. Use the lowest concentration of drug which will block sensory perception. Large volumes are generally used. 3. Epinephrine approximately doubles duration of action. 4. Most frequently used agents include lidocaine 0.5-1% and Bupivacaine 0.5% C. Regional Nerve Block and Field Block 1. Field block: Similar to local infiltration, but the goal is to specifically interrupt nerve transmission proximal to the site to be anesthetized. 2. Nerve Block - The goal is to inject local anesthetic into or about individual nerves or nerve plexuses. Produces even greater areas distal of anesthesia with a smaller amount of drug 8. Agents include Procaine (0.5-2.0%); Lidocaine (1-2%); Mepivacaine (up to 7 mg/kg of 1-3%); Bupivacaine (0.250.75% up to 3 mg/kg ); Tetracatine (up to 1.5 mg/kg of 0.1-0.2%). D. Intravenous Regional Anesthesia 1. Consists of iv injection of local anesthetic into vein of exsanquinated extremity with proximal tourniquet. 2. Binding of drug occurs in tissues of extremity - with tourniquet down (after 15-30 min minimum up time) only 15-30% released into systemic circulation. 3. More effective in upper extremity 4. Lidocaine (1.5 mg/kg of 0.5%) frequently used. E. Epidural Anesthesia (caudal anesthesia) 1. Epidural space terminates cephically at the foramen magnum. 2. Epidural anesthesia consists of epidural injection into the lumbar, or less frequently, the thoracic area. 3. Two sites of action (a) diffusion into subarachnoid space (b) diffusion into paravertebral area through intervertebral foramina to produce multiple paravertebral blocks Continue--. Epidural Anesthesia (caudal anesthesia) 4. Danger of inadvertent subdural and subarachnoid puncture. * Lidocaine & Bupivacaine for longer action are used. 5. Unlike spinal, no differential zone of sympathetic blockade. There is a zone of differential motor blockade 4-5 segments less than sensory block. 6. Other dangers include anterior spinal artery syndrome, hematoma, infection, and adhesions. 10. Advantages include (a) blood pressure remains stable (b) in obstetrical cases, the mother retains motor control of the abdominal muscles and can assist in the delivery of the fetus F. Spinal Anesthesia (subarachnoid block) 1. Injection of local anesthetic into the lumbar subarachnoid space ; usually at T2-T3 or T3-T4 interspace. 2. Distribution of the drug in the subarachnoid space determines the level of anesthesia. This is controlled by: a) Positioning of the patient b) Speed of injection c) Specific gravity of solution d) Volume injected 3. Nerve fibers affected in the following sequence: autonomic sensory motor 4. Zones of differential anesthesia: sympathetic block segments higher than sensory - motor segments lower Continue-- Spinal Anesthesia (subarachnoid block) 5. It causes sympathetic blockade. Most important changes are on venous side of circulation. 6. Cardiovascular effects: hypotension, bradycardia, ↓preload ↓afterload 7. Respiratory complications: due to ischemic paralysis of medulla and not usually phrenic paralysis 8. Other dangers: * chemical transection of cord * traumatic destruction of a spinal end artery * traumatic damage of a nerve root & chronic arachnoiditis * postural headache and infection. 9. Agents frequently employed include: Tetracaine & Lidocaine Pharmacology of L.A. •They interfere with function of all organs in conduction occurs A- CNS Stimulate CNS leads to restlessness and may proceed by clonic convulsion •Then CNS depression • Respiratory failure is main cause of death • Drowsiness is the most complain Pharmacology of L.A. B- Cardiovascular • Decrease mycardium excitability •Conduction • Decrease force of contraction • Hypotension • These effects occurred in high dose which cause CNS toxicities • Arteriodilation • Rarely occurs in infilteration Pharmacology of L.A. C- Hypersensitivity • Mostly occurred with ester type • Allergic dermatitis • asthmatic attack • Amide almost free of hypersensitivity Lidocaine 2% 1- DOSE *OVER 10 YRS: Not exceed 6.6 mg/kg or 300 mg per dental appointment 2- under 10 years 100-150 mg per dental CH appointment H 3 N 3- Drug interaction -beta blockers -antiarrhythmia agents 4- Metabolism O CH3 N CH3 CH3 Lidocaine HCl - Xylocaine®, Octocaine®, Dilocaine®, Duo-Trach® Also available with or without Epinephrine CH3 Prilocaine 4% 1- DOSE: -Less than 10 yrs CH3 H N O N H CH3 Prilocaine HCl - Citanest® 40 mg per setting or less - greater than 10 yrs and adult 40-80 mg -Not exceed 400-600 mg in adult 1- Toxicities * Methemoglobinemia 2- under 10 years 100-150 mg per dental appointment BUPIVACAINE 0.5% 1- DOSE: -Less than 10 yrs NOT ESTABLISHED - greater than 10 yrs and adult 9 mg -Not exceed 90 mg in adult per dental appointment CH3 2- duration H N -Nerve block 5-7 hrs O CH3 3- Toxicities - much greater than lidocaine N CH3 Bupivacaine HCl - Marcaine®, Sensorcaine® MEPIVACAINE Amide Products: Longer duration of action CH3 H N O CH3 N CH3 Mepivacaine HCl - Carbocaine®, Polocaine®, Isocaine® 1- Indications: Peripheral, transvaginal, paracervical, caudal, epidural and infiltration nerve block, dental procedures 2- protein bound 78% 3- Warnings: * NOT recommended for obstetrical epidural anesthesia due to cardiac arrest and death * Reserve the 0.75% solution for surgical procedures where prolonged activity is needed—danger of inadvertent IV injection and cardiac arrest ETIDOCAINE Amide Products: - Longer duration of action CH3 CH3 H N N O CH3 CH3 CH3 Etidocaine HCl - Duranest® 1- Indications: peripheral, central or lumbar peridural nerve block; intra-abdominal/pelvic/lower limb/ceasarean section surgery; caudal or maxillary block 2- Onset of action 3-5 minutes 3- with a duration of action of 5-10 hours 4- surprisingly epinephrine addition does NOT increase the duration—why?----Partition coefficient is 7050X of procaine---94% protein bound ROPIVACAINE Amide Products: - Longer duration of action CH3 H H N O CH3 N CH3 Ropivacaine HCl - Naropin® 1- Indications: local or regional anesthesia for surgery, post-operative pain management and obstetrical procedures 2- Avoid rapid administration of large doses---use fractional or incremental administration 3- ideal for continuous infusion for epidurals during birth 4- Onset of action is 10-15 minutes 5- with a duration of action of 2-8 hours---safe to use this as an epidural product for up to 24 hours CH3 O TETRACAINE O Ester Products: N CH3 HN CH3 Tetracaine HCl - Pomntocaine® 1- Indications: Spinal anesthesia including high, median, low and saddle blocks including prolonged action of 2-3 hours 2- Slower onset of action than procaine but duration is 2-3 hours ------ can increase to 3-5 hours by including epinephrine 3- This drug should not be used in children due to a lack of safety data COCAINE (1)- Mechanism of action A- Blocks sodium channel B- inhibit NE UPTAKE-1 (2) Direct vasoconstrictor action and potentiation sympathetic system (3) Extensive cardiovascular actions (4) Powerful CNS stimulant (5) Considered a narcotic with potentially for psychic dependence (6) Used for surface anesthesia in 1.0-10.0% solutions, occasionally with epinephrine (7) Metabolized by esterases and hepatic enzymatic degradation; t1/2 after oral or nasal administration, approximately 1 hour LOCALLY ACTING AGENTS LOCAL HAEMOSTATIC AGENTS LOCALLY ACTING AGENTS LOCAL HAEMOSTATIC AGENTS 1- Sympathomimetic •Epinephrine with LA •Epinephrine-imprignated cord to retract and control gingival haemorrhage 2- Astringents & STYPTICS -They react with proteins of oral cavity and make protective layer: •Aluminum chloride (Sansilla) –Example of Styptics : Silver nitrate rod LOCAL HAEMOSTATICS •Aluminum chloride retraction cord (HEMODENT 25%) • Tannins: Pyralvex -it is an oral paint contains tannic acid and salicylic acid - It is used for mild peri-oral lesion & less effective in oral lesion 3- Mechanical haemostatics •They forms matrices in which blood cells and fibrin can trapped •They are more effective than astringent, styptics or sympathomimetics • in controlling capillary oozing & surface bleeding Types of mechanical haemostatics 1- Absorbable gelatin (Gel Foam) * Advantages of absorbable gelatin -It does not interfere with the followings: •Thrombin •Epithelization •Bone regeneration 2- Oxidized cellulose (Oxycel &Novocel) • It has high affinity to haemoglobin & it is form of gauze of cotton pellets •It is more effective than Gelfoam •It interfere with followings: - Epithelization & bone regeneration (not suitable for packing in bone fracture - Inactivates thrombin 3- Oxidized regenerated cellulose (Surgicel) •Advantages - It does not interfere with epithelization -Therefore , it is suitable for surface dressing •Disadvantages - It interferes with bone regeneration - Inactivates thrombin 3- Microfibrillar collagen hemostat (Avitene) It is in the form of powder & used to control bleeding after oral surgery * Advantages - It does not interfere with: * epithelization * bone regeneration * activity of thrombin SYSTEMIC HAEMOSTATICS HAEMOSTATIC SYSTEMS •1- Formation of fibrin via clotting factors 2- Fibrinolysis 3- Platelets aggregation 4- Blood vessels (PGE12) Examples of systemic haemostatic agents VITAMIN K •Role of vitamin K in clotting system - Vit K is necessarly for final stage of clotting factors synthesis such as prothrombin ,factor vii, ix &x Premature Clotting factors Mature clotting factor CAUSES OF VIT K DEFICIENCY 1- Obstructive jaundice 2- malabsorption 3- Reduced GIT flora -Rarely after broad spectrum antibiotics CLINICAL USES OF VITK 1-Reverse bleeding induced by oral anticoagulant 2- Inadequate vit k availability 3- new born baby VIT K Preparations vit k1 (phytomenandione) konakion - it is lipid soluble and injected in new born baby -onset within 12 hours -Menadiol sodium phosphate (vitk3) • it is water soluble • onset 24 hrs • prefered in malabsorption or obstructive jaundice •It has tendency to induce hemolytic anemia TRANEXAMIC ACID 1- MECHANISM OF ACTION •Prevents plasminogen not to attach to fibrin • resulting in inhibition fibrinolysis • inhibits the proteolytic activity of plasmin 2- Clinical uses •Use as Mouthrinse 4.8% to prevent bleeding in hemophiliac & patient under warfarin due to dental extraction • ORAL: 25 MG/KG FOR 2-8 DAY in haemophiliac •Hereditary angioedema & menorrhagia •Thrombolytic over dose TRANEXAMIC ACID 3- pregnancy Risk factor B •to prevent bleeding in hemophiliac & patient under warfarin due to dental extraction 3- Adverse effects •If taken orally -GIT Disturbances such as diarrhea -Hypotension -Thrombosis -Blurred vision requires regular eye examination --Regular liver function tests in long term oral use for hereditary angioedema AMINOCAPROIC ACID 1- Mechanism of action •Inhibits the activation of plasminogen to plasmin 2- Clinical uses •Treatment of excessive bleeding from fibrinolysis • 5-30 g/day in divided dose at 3-6 hrs interval AMINOCAPROIC ACID 3- pregnancy Risk factor C •4- Adverse effects •Hypotension • bradycardia •Arrhythmia •Myopathy •GIT irritation APRPTONIN (Trasylol) It is inhibitor of plasmin (plasmin causes fibrin lysis) •CLINICAL USES - Over dose of thrombolytic drugs such streptokinase - Hyperplasminia as a result of mobilization and dissection of malignant tumor SIDE EFFECTS -Hypersensitivity --localized thrombophlebitis ETHAMSYLATE OR ETAMSYLATE DICYNENE® 1- Mechanism of action •CORRECT ABNORMAL PLATELETS ADHESION 2- Clinical uses •Short term use in blood loss in menorrhagia(500mg tablets four times daily during menses •Prophylaxis and treatment of periventricular haemorrhage in low birth weight infants (i.v. or i.m.) 3- Clinical uses - Rashes , Nausea and Headache DESMOPRESSIN ACETATE(Stimate®) 1- Mechanism of action •Enhance reabsorption of water in kidney •Increase Von Willebrand factor & factor viii 2- Clinical uses •Control bleeding in mild hemophilia & Von Willebrand disease during dental extraction •Diabetes insipidus •Nocturnal enuresis •CAUTION : Avoid overhydration (it has ADH activity) DESMOPRESSIN ACETATE 3- pregnancy Risk factor B •4- Adverse effects •Facial flushing • Dizziness •Nasal congestion •hyponatremia •Water intoxication BLOOD PRODUCTS 1- Anti-hemophilic factor (Kogenate®) •It is factor viii derived from recombinant DNA - CLINICAL USES - Control bleeding in hemophilia A - Life threatening haemorrhage 2- FACTOR VIIa (NovoSeven®) -It is recombinant DNA CLINICAL USES: * PATIENT WITH INHIBITORS TO FACTORS VIII & IX BLOOD PRODUCTS 3- FACTOR IX (Replenine®) •- CLINICAL USES - it indicated in patient with factor ix deficiency (Hemophilia B) - CAUTION : Risk for thrombosis FIBRIN GLUE (Beriplast) 1- Composition •Two separate solutions a- fibrinogen b- thrombin & calcium •It is completely reabsorb within 2 –4 weeks •Some products contain -tranexamic acid or aprotonin 2- Effective in preventing bleeding in bleeding disorders Management of patient under warfarin 1- Minor surgery •Use tranexamic mouth rinse • without adjustment of anticoagulation if INR is less than 4 2- Major surgery •Stop warfarin preoperative • use low molecular weight heparin Intrinsic Pathway Extrinsic Pathway Tissue Injury Blood Vessel Injury Tissue Factor XIIa XII Thromboplastin XIa XI IXa IX Xa X Factors affected By Heparin VIIa Prothrombin Vit. K dependent Factors Affected by Oral Anticoagulants Fibrinogen XIII VII X Thrombin Fribrin monomer Fibrin polymer ANTI-COAGULANTS 1- Drugs inhibit vit k actions (oral anticoagulant) -By prevents maturation of the clotting factors - slow onset (3 days) 2- Drugs directly acting on the clotting factors - Rapid onset (Heparin) 3- Drugs inhibit platelets aggregation 4- Fibrinolytic drugs (dissolve clot) ORAL ANTI-COAGULANTS WARFARIN (Coumadin®) 1- CLINICAL USES OF WARFARIN •Prophylaxis and treatment of venous thrombosis such as : - Deep vein thrombosis (DVT) - Atrial fibrillation - prosthetic cardiac valves with antiplatelets - thromboembolic disorders such post MI or Stroke and embolism ORAL ANTI-COAGULANTS WARFARIN (Coumadin®) 2- MOA OF WARFARIN •Warfarin interferes with hepatic synthesis of vit K-dependent factors (ii, vii, ix, x) • PREVENT RECYCLING OF VIT K by inhibiting reductase enzyme which convert epoxide vit K to vit K 3- ONSET OF WARFARIN -Within 36-72 hours Mechanism of action Descarboxy Prothrombin Prothrombin Reduced Vitamin K Oxidized Vitamin K NAD NADH WARFARIN ORAL ANTI-COAGULANTS WARFARIN (Coumadin®) 4- MONITORING ITS EFFICACY •Prothrombin time expressed by : •International Normalized Ratio (INR) determined daily initially then at longer intervals depends on the response • INR 2-2.5 For prophylaxis of DVT, AF, Cardioversion, dilated cardiomyopathy, MI, Rheumatic valve disease • INR 3.5 For recurrent DVT , pulmonary embolism and mechanical prosthetic heart valve ORAL ANTI-COAGULANTS WARFARIN (Coumadin®) 4- ADVERSE EFFECTS OF WARFARIN • The main is hemorrhage •Skin necrosis in patient with protein c & s deficiency 5- PREGNANCY •AVOID RISK FACTOR D •REPLACED BY HEPARIN ORAL ANTI-COAGULANTS WARFARIN (Coumadin®) 6- DRUG INTERACTION •INCREASE EFFECTS: - NSAIDs - Sulfa drugs - cimetidine •Decrease effects liver enzyme inducer such as: -phenobarbitone, rifampicin, phenytoin HEPARIN 1- RAPID ONSET, inject only S.C. OR I.V. 2- CLINICAL USES •Preventive and treatment of thromboembolic disorders such as DVT, MI, pulmonary emobolism • patient undergoin general surgery (low dose) • orthopedic surgery • unstable angina & Pregnancy •Extracorporeal circuits such as hemodialysis & cardiopulmonary bypass HEPARIN 3- DOSES OF HEPARIN • PROPHYLAXIS DOSE A- Post-operative & MI 5000 units s.c. every 8-12 hrs B- pre-surgery 5000 units 2 hours before surgery C- Pregnancy 5000 -10,000 units every 12 hours (REQUIRED APTT monitoring HEPARIN 4- MECHANISM OF ACTION OF HEPARIN • Heparin enhances the activity of anti-thrombin • It inhibits factor X in small dose 5- MONITOR THE EFFICACY Prophylaxis dose does NOT require APTT (Activated partial thromboplastin) APTT should be in the ranges 1.5-2.5 Heparin mechanism of action Heparin Antithrombin III Thrombin HEPARIN 6- ADVERSE EFFECTS •Bleeding if APTT more than 3 or - impaired hepatic or renal functions •Thrombocytopenia • Osteoporosis (long term use) • skin necrosis & hypersensitivity • It may induce hyperkalemia by inhibition of aldosterone secretion •7- ANTIDOTE OF HEPARIN - Protamine sulfate 100mg neutralizes 100 unit LOW MOELCULAR WEIGHT HEPARIN 1- EXAMPLES: •Enoxaprin , Dalteparin & Ardeparin 2- Advantages A- Do not required APTT monitoring B- because it has little effects on antithrombin but it potent inhibition on factor Xa •C- Long duration (once daily)اىل هنا HEPARINOID 1- EXAMPLES: •DANAPAROID 2- MOA : inhibits Xa & IIa factors 3- Advantages A- Low incidence of thrombocytopenia * therefore it can be used in patient had history of thrombocytopenia due to heparin 4- Disadvantage : not effectively antagonized by protamine sulfate ANTIPLATELETS AGGREGATION 1- EXAMPLES: •Aspirin •Clopidogrel •Dipyridamole •Ticlopidine •Abciximab •Eptifibatide •Tirofiban ANTIPLATELETS AGGREGATION 2- THEY DECREASE PLATELETS AGGREGATION and inhibit thrombus formation in the arterial circulation where anti-coagulants have little effects. 3- General Clinical uses •cerebral vascular diseases such as Transient ischemic attack (TIA) •Unstable angina •Post MI •Coronary artery bypass surgery & Angioplasty ASPIRIN 1- CLINICAL USES OF ASPIRIN (small dose) Prophylaxis for MI (75mg- 81mg-160-325 mg) • Transient ischemic episode & stroke (600 mg twice daily) •Following coronary bypass surgery • percutaneous transluminal coronary angioplasty •Eclampsia in small dose ? Unlabelled 2- MOA : Irreversibly inhibits COX (cyclooxygenase) leading to inhibit thrombane A2 in platelets ASPIRIN 3- ADVERSE EFFECTS OF ASPIRIN •GIT upset may develop ulcer •May precipitate bronchial asthma in patient has histry of bronchial asthma • Some patient develop subcutaneous hemorrhage (as spots) 4- contraindication * children under 12 years and breast feeding mother * active peptic ulcer * bleeding disorders 5- Caution: * asthma , pregnancy CLOPIDOGREL (PLAVIX) 1- CLINICAL USES *Reduces atherosclerosis events such as MI, Stroke & peripheral artery diseases •Prevent of thrombotic complications after coronary stenting •Acute coronary syndrome such as unstable angina or non-Q-wave MI • It can be used instead of aspirin if patient allergic to aspirin 2- MOA It blocks the ADP receptors in platelets which prevent fibrinogen CLOPIDOGREL (PLAVIX) 3- ADVERSE EFFECTS •Bleeding (GIT & Brain) & leukopenia •GIT upset such as gastritis (less than aspirin) 4- CONTRAINDICATIONS •Active bleeding avoid first few days after MI & 7 days after stroke •Not recommend for angioplasty •Stop it 7 days before surgery TICLOPIDINE (TICLID) 1- CLINICAL USES •It is reserved for patients who are intolerant to ASPIRIN •Prophylaxis of major ischemic events in patient with a history of ischemic stroke •Adjuvant therapy with aspirin following coronary stent to reduce stent thrombosis 2- MOA Similar to plavix TICLOPIDINE (TICLID) 3- ADVERSE EFFECTS •Bleeding •Neutropenia , agranulocytosis & pancytopenia •Thrombotic thrombocytopenic purpura •Increases liver enzymes •Jaundice •hyperlipidemia DIPYRIMADOLE (PERSANTIN) 1- CLINICAL USES: Maintains patency after surgical grafting include coronary artery bypass •Used with Warfarin to decrease thrombosis in patient after artificial heart valve replacement •Use with ASPIRIN to prevent thromboembolic disorders •It can be given 2 days prior open heart surgery 2- MOA: Inhibits adenosine deaminase & phosphodiesterase leading to accumulation of: •Adenosine , adenosine nucleotides These inhibit platelets aggregation DIPYRIMADOLE (PERSANTIN) 3- ADVERSE EFFECTS •Hypotension •Headache •Increased bleeding during or after surgery •Worsening symptoms of coronary heart disease 4- CAUTIONS •Rapidly worsening angina •Aortic stenosis ABCIXIMAB(REOPRO) 1- CLINICAL USES •Adjunct to percutaneous transluminal coronary angioplast •Prevention of acute ischemic complications in patients at high risk for abrupt closure of treated coronary vessels •Use with heparin in unstable angina 2- MOA It binds with platelets iib/iiia receptors preventing FIBRINOLYTIC DRUGS 1- EXAMPLES •Alteplase (recombinant DNA tissues plasminogen activator) •Reteplase •Streptokinase •tenecteplase ALTEPLASE (ACTIVASE) 1- CLINICAL USES •Management of acute MI •& pulmonary embolism for lysis of thrombi 2- MOA * It initiates local fibrinolysis by binding to fibrin in clot and converts entrapped plasminogen to plasmin ALTEPLASE (ACTIVASE) 3- adverse effects •Multiple emboli •Arrhythmia due to cardiac reperfusion •bleeding ANTICOAGULANT DRUGS TO TREAT THROMBOEMBOLISM Drug Class Anticoagulant Parenteral Prototype Heparin Action Inactivation of clotting Factors Effect Prevent venous Thrombosis Anticoagulant Warfarin Decrease synthesis of Oral Clotting factors Prevent venous Thrombosis Antiplatelet drugs Aspirin Prevent arterial Thrombosis Thrombolytic Drugs Streptokinase Fibinolysis Decrease platelet aggregation Breakdown of thrombi ORAL PROTECTIVE AGENTS 1- CLINICAL USES :Protectives are used for non-specific mouth ulceration such as aphthus ulcer •It is usually combines with local anesthetic and antiseptics such as [ORAL B®] composed of: -lidocaine, cetylpyridinium, menthol & cineole 2- examples of oral protectives •Carmelose gelatin (ORABASE®) •Choline salicylate dental gel (BOJELA®) •Benzdamine (DIFFLAM®) ANTI-SEPTIC MOUTH RINSE 1- Chlorhexidine 2- Cetylpyridinium chloride & Triclosan 3- phenols 4- Hexitidine (oraldene mouth rinse) 5- Domiphen bromide (Bradoral lozenges) CHLORHEXIDINE 0. 2% CORSODYL® & Hexidine® 1- PROPERTIES OF CHLORHEXIDINE * It is used in 0.2% as mouth rinse * It is the most effective mouth rinse •It Reduces gingival pathogen •The anti-microbial last several hours • it is effective in gingivitis associated with bleeding & PUS • it cause permanent stain of restorative •But reversibly stains natural teeth & dorsum of the tongue CHLORHEXIDINE 0. 2% CORSODYL® & Hexidine® 2- MOA •It broad spectrum antiseptic • its bacterial action exerts by disruption of bacterial membrane of both gram positive & negative bacteria 3- CLINICAL USES •Oral hygeine especially if there heavy plaque •Inhbition of plaque formation •Gingival infection •It may help in recurrent aphous ulcer CHLORHEXIDINE 0. 2% CORSODYL® & Hexidine® 4- ADVERSE EFFECTS •Reversible brown staining of natural teeth •Irreversible brown staining of artificial teeth (restorative) •Idiosyncratic Epithelial irritation of oral cavity •Rarely parotid gland swelling •Inflammation of salivary glands • It may mask periodontitis CETYLPYRIDINIUM CHLORIDE0.5% SCOPE® 1-PROPERTIES •It is surface active agent •It is ineffective in present of bleeding, sputum & pus •It is weak antibacterial 2- MOA •It acts as detergent which help removal of bacteria & Disrupts the membrane of bacteria PHENOLS CHLORASEPTICS® •It contains phenol • Available as spray , mouth rinse & lozenges 2- ADVERSE EFECTS OF PHENOL •Nephrotoxicity if exceeds the dose • It inhibits polymerization of resin restoration • It damage the cavity liner Agents used in dental procedures 1- HYDROGEN PEROXIDE • It is used for root canal irrigation • Its action is mediated by releasing nascent oxygen which kills bacteria 2- SODIUM HYPOCHLORITE 5% •It is used to irrigate root canal • It is irritant to mucous membrane of oral cavity Agents used in dental procedures 3- OBTUNDANTS A- DEFINTION OF OBTUNDANT Chemical precipitates cellular protein of nerve fiber Causing paralysis of nerve fiber which leads to diminish sensation of dentine B- IDEAL PROPERTIES OF OBTUNDANTS •Acts without initial pain •Does not stain teeth, dentine or enamel •It penetrates quickly through the dentine but not too deep otherwise it may lead to inflammation of the pulp Agents used in dental procedures C- MOA OF OBTUNDANT •It precipitates cellular protein of nerve fiber • Causing paralysis of nerve fiber which leads to diminish sensation of dentine D- CLINICAL USES Obtundants allow painless excavation EXAMPLES OF OBTUNDANTS 1- Eugenol •It causes initial stimulation followed by paralysis of nerve 2- Zinc chloride •It stains teeth and has poor penetration 3- Absolute Alcohol •It requires the oral cavity to be dry 4- Cresote Agents used in dental procedures 4- MUMIFYING AGENT A- Definition of mumifying agents •It is a chemical causes aseptic dryness and hardness of pulp tissues and root canal •They have astringent and antiseptic properties • All mumifying agents are obtundant but not all obtundants are mumifying agents B- CLINICAL USES * They applied when pulp or content of the root can NOT be removed EXAMPLES OF MUMIFYING AGENTS 1- Iodinated cresol 2- beta-naphthol 1% in alcohol 3- iodoform 4- Ammonical silver nitrate (it stains teeth) 5- Forlmaldehyde FLOURIDE PREPARATIONS 1- NATURAL SOURCE OF FLOURIDE •Water (1PPM iseffective cincentration) • Fish (20 PPM) • Tea (100 PPM) 2- METABOLISM & ABSORPTION OF FLOURIDE •Calcium and magnesium decrease flouride absorption • Flouride concentrates in bone & teeth •In children, the flouride concentrates in bone and teeth than elderly FLOURIDE PREPARATIONS 3- MECHANISM OF ACTION OF FLOURIDE •Flouride converts hydroxyapatite to FLOUROAPATITE which leads - Makes the apatite structure more stable which improve CRYSTALLINITY of the structure - FLOUROAPATITE is less soluble in acid - FLOURIDE inhibits bacteria enzymes EXAMPLES FLOURIDE PREPARATIONS 1- ACIDULATED PHOSPHATE FLOURIDE (APF) • It contains flouride between 10,000 to 20,000 PPM • It is the preparation of choice for professional flouride application • It benefits last 2-3 years after application on the teeth • Contact time upon application is (1-4 minutes) depends on the type of preparation. EXAMPLES FLOURIDE PREPARATIONS ACIDULATED PHOSPHATE FLOURIDE (APF) A- Advantages of APF • Stable in solution • Not irritant to gingiva • Agent of choice for professional application B- Disadvantages of APF • APF is acidic solution may affect CEMENTUM • Not suitable for dentrifrices EXAMPLES FLOURIDE PREPARATIONS 2- SODIUM FLOURIDE • It is available in tablets such as Zymaflour® 1mg • 0.25 MG (1/4 Tablet) per day required for 5-16 years old A- Advantages of sodium flouride •Stable in solution • Neutral solution (Ph 7.0) B- Disadvantages of sodium flouride • It is NOT compatible with many abrasives in tooth-paste because: - it reacts with CALCIUM & PHOSPHATE - and becomes insoluble compound EXAMPLES FLOURIDE PREPARATIONS MOUTH RINSE CONTAINS SODIUM FLOURIDE • It is more effective than MFP present in tooth-paste • but combination of sodium flouride mouth rinse with dentrifrices are more effective than either product alone • Mouth rinse containing FLOURIDE 100 PPM recommend to use it twice daily • Mouth rinse containg 250 PPM used once daily • mouth rinse contains 1000 ppm used once weekly or every other week (هنا EXAMPLES FLOURIDE PREPARATIONS 3- SODIUM MONOFLOUROPHOSPHATE (MFP) • It is commonly used in tooth-paste A- Advantages of (MFP) •Stable in various pH • It is compatible with tooth-paste abrasives B- Disadvantages of (MFP) • It is weak flouride source • Efficacy is questionable EXAMPLES FLOURIDE PREPARATIONS 4- STANNOUS FLOURIDE A- Advantages of STANNOUS FLOURIDE •Both cation & anion are effective B- Disadvantages of STANNOUS FLOURIDE • Unstable in solution • Stain teeth • bitter taste TOXICITY OF FLOURIDE A- ACUTE TOXICITY •It is common during applying APF IN CHILDREN •Fatal dose 50-225 mg/kg • Symptoms of toxicity - Nausea, vomiting - Abdominal pain - Sweating - Convulsion - Death TOXICITY OF FLOURIDE B- CHRONIC TOXICITY It is occurs at concentration ranges between 2-8 ppm consumed in drinking water • Flourosis occurs when the crown of permanent teeth are forming • DEFINITION OF FLOUROSIS - Is hypoplastic defect resulting from disturbance in the function of AMELOBLAST (enamel) during teeth development Symptoms of chronic toxicity - endemic flourosis is associated with - mottled enamel & deformed teeth DENTRIFERICES 1- It is a pharmaceutical preparations are used locally on the teeth & oral cavity to perform the followings: •Clean •Polish •Prevent bacterial fermentation •Prevent gingivitis •Prevent dental caries EXAMPLES OF DENTRIFERICES •TOOTH PASTE •POWDER •LIQUID IN FORM OF SOLUTION TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 1- Abrasive •It is am inert , insoluble and finely powdered •Examples of abrasives - calcium pyrophosphate - dicalcium phosphate •Main action of abrasive - it cleans and polish - removes stain and plaque TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 2- Flavouring agents •They have the following properties: • good odor • mild antiseptic • mild local anesthetic • counter irritant •Examples of flavouring agents - peppermint - cinnamon TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 3- SWEETNER •Examples of sweetner - Saccharin - aspartame - glycerin TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 4- HUMICTANT • FUNCTIONS OF HUMICTANTS: - Keep moisture of the tooth-paste - prevents dryness of the tooth paste - it gives plasticity to the tooth-paste - it has demulcent action on the gum •Examples of sweetner -GLYCERIN - SORBITOL TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 5- DETERGENT & FOAMING AGENTS • FUNCTIONS OF HUMICTANTS: - they lower surface tension(emulsifying agents) - emulsify fatty materials - Promote good penetration and mixing of constituents of the tooth-paste - they assists in removal mucous deposit and debris TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE EXAMPLES DETERGENT & FOAMING AGENTS Examples of detergent and foaming agents: - sodium lauryl-sulfate - magnesium lauryl-sulfo-acetate - monoglyceride - dioctyl-sodium-sulfo-succinate TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 6- THICKENING AGENTS •FUNCTIONS - Improve & maintain the consistency of the paste - they prevent separation of the tooth-paste contents under extreme temperatures (high & low) Examples of thickening agents: - glycerin starch - carboxy-methyl-cellulose - sodium alginate TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 7- PRESERVATIVES •FUNCTIONS - prevent bacterial , fungal growth which prevents fermentation of the tooth-paste Examples of preservatives: - methylparaben 0.15% - propylparaben 0.15% TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 8- FLOURIDE •FUNCTIONS - It is anti-cariogenic agent and significantly reduces caries - it is commonly used sodium-mono-flourophosphate (MFP) because : * it is stable at various Ph * compatible with many abrasives TOOTH-PASTE MAIN INGREDIENTS OF TOOTH PASTE 9- DESENSITIZING AGENTS •Not present in most of tooth-paste • examples of desensitizing agents - Potassium nitrate - Potassium oxalate GLUCOCORTICOIDS •Adrenal steroids are synthesised from zona fasciculata of adrenal cortex as needed •It is stimulated by ACTH which is release from pituitary gland • ACTH is regulated by CRF in hypothalamus •Glucocorticoids is synthesised from chlosterol • Stress also stimulate glucocorticoids Adrenal Gland Glucocorticoids MECHANISM OF ACTION •Glucocorticoids bind with specific receptors in the cytoplasms • The complex binds with DNA which leads to: * prevent transcription such as - COX-2 - Block Vit D3 –mediated induction of osteocalcin * or induce particular gene - Such as LIPOCORTIN-1 & Tyrosine hydroxylase MECHANISM OF ACTION •Glucocorticoids bind with specific receptors in the cytoplasms • The complex binds with DNA which leads to: * prevent transcription such as - COX-2 - Block Vit D3 –mediated induction of osteocalcin * or induce particular gene - Such as LIPOCORTIN-1 & Tyrosine hydroxylase Direct effects come from receptor binding CBG albumin HSP70 IP IP HSP70 HSP90 HSP90 transcription GRE GRE GRE Altered cellular function protei n Example of indirect inhibition of gene induction Cytokines COX-2 NOS-2 NF-B NF-B TNF- TNFR NF-B IB GCR IB GC IB GCR GLUCORTICOIDS (PAF) Phospholipase A2 Pharmacological action of glucocorticoids 1- General effects on metabolism - Water, edlectrolyte balance and organ systems 2- Negative feedback on Pituitary & Hypothalamus 3- Anti-inflammatory and immunosuppressive GENERAL METABOLIC & SYSTEMIC EFFECTS 1- Carbohydrate and protein metabolism 2- Decrease glucose utilization 3- increase gluconeogenesis which may induce hyperglycemia 4- Decrease in protein synthesis breakdown 5- It has permissive effects on the lipolytic response to catecholamines GENERAL METABOLIC & SYSTEMIC EFFECTS 6- Redistribute fat in large dose 7- It has some mineralocorticoids activities 8- Increase calcium secretion & decrease its absorption 9- Reduce function of osteoblast 10- and Increase the activity of osteoclast (Digest bone) * by hypocalcemia-induced parathyroid hormone secretion * These lead to osteoporosis NEGATIVE FEEDBACK EFFECTS 1- Both endogenous and exogenous glucocorticoids have a negative feedback on CRF & ACTH 2- The inhibitory effects of endogenous glucocorticoids due to exogenous steroids is prolonged (months) 3- lipocortin-1 play negative feedback on hypothalamus and pituitary 3- and leads to atrophy of adrenal cortex Atrophy due to negative feedback inhibition of ACTH 3rd vent (-) (+) CRF neuron IL-1 IL-2 IL-6 TNF- (+) immune system (-) (-) ACTH (+) Adrenal d Cortisol administered glucocorticoid Anti-Inflammatory 1- Inhibit production of prostaglandins due to decrease the expression of COX-2 2- inhibit early and late manifestation of inflammation 3- Which leads to prevent chronic inflammation 4- Decrease fibroblast which leads to inhibition of chronic inflammation (less fibrosis) and wound healing and repair Continue anti-inflammatory effects 5- Inhbits Phospholipase A2 by inducing lipocortin which leads to: •Decrease production of PAF • Arachidonic acid which is the precursor for: * Production of prostaglandins * Leukotrienes (slow reacting substance of anaphylaxis Continue anti-inflammatory effects 6- Decrease histamine release 7- decrease production of nitric oxide 8- Decrease production of PAF 9- Decrease the production of GM-CSF which is essential for production of: -platelets -Monocyte, neutrophil & eosinophil -RBCs IMMUNOSUPPRESSIVE EFFECTS * Drug binds only to certain targets •Supress initiation generation of immune response •It is non-selective ** Supress cellular immunity ** and Humeral * It induces apoptosis of lymphocyte ADVERSE EFFECTS OF GLUCOCORTICOIDS • Adverse effects occur after prolonged used • or large dose 1- Supress response to infection or injury 2- Impair wound healing 3-Slight incidence of peptic ulcer 4- Cushing’syndrome 5- Osteoporosis 6- Hyperglycemia ADVERSE EFFECTS OF GLUCOCORTICOIDS 7- Muscle wasting 8- Inhibit growth in children 9- Euphoria & Psychosis 10- decrease blood supply to bone leading to necrosis the head of the femur inhalation ADVERSE EFFECTS OF GLUCOCORTICOIDS 11- cataract 12- glaucoma 13- increase in intracranial pressure 14- disorder of menestrual cycle 15- oral thrush especially when taken by inhalation 16- Adrenal insufficiency * It may take two months or more up to 18 months GUIDELINES FOR GLUCOCORTICOID THERAPY 1- It should based on the severity of diseases 2- Dosage, frequency, duration & preparation influence the response and adverse reactions 3- Administered locally when possible inorder to minimize the adverse effects & efficacy 4- The pharmacological dose should be tapered in order to avoid adrenal crisis CLINICAL USES OF GLUCOCORTICOIDS 1- Replacement therapy (Addison’disease 2- Asthma 3-Topically in various inflammatory condition -skin , eye, nose 4- Post neurosurgery &head and spinal injury 5- Autoimmune diseases -Inflammatory bowel disease - haemolytic anemia CLINICAL USES OF GLUCOCORTICOIDS 6- Anti-cancer with other cytotoxic agents 7- Autoimmune diseases 8- Inflammatory diseases - haemolytic anemia - organ transplant with other immunosuppressants 9- Anti-emetic in conjunction with other antiemetic GLUCOCORTICOIDS USES IN DENTAL PRACTICE 10- Temporary relief of sympton associated with Oral inflammation and ulcerative lesion such as A- Recurrent aphthus stomatitis Triamcinolone acetonide (Kenalog orabase) B- Erosive lichen planus -- Dexamethasone C- Major aphthae - Kenalog orabase CLASSIFICATION OF GLUCOCORTICOIDS DURATION OF ACTION Pregnancy Risk Potency Short (8-12hrs) - Hydrocortisone - Cortisone C D 1 0.8 C C B C 5 4 4 5 Intermediate (18-36) - Methylprednisolone - Prednisolone - Prednisone - Triamcinolone CLASSIFICATION OF GLUCOCORTICOIDS Duration of action Pregnancy Risk Potency Long acting (36-54) - Betamethasone C 25 - Dexamethasone C 25-30 INHALER GLUCOCORTICOIDS DRUG Pregnancy Risk Potency Compare to dexamethasone=1 Fluticasone C 1200 Budesonide C 980 C 600 (Pulmicort, Rhinocort) Beclomethasone (Beconase, Beclovent) Triamcinolone 330 SEE YOU NEXT TIME Thank you