GI Physiology Resource 1 Jan 17, 2011
advertisement

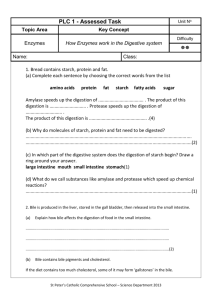
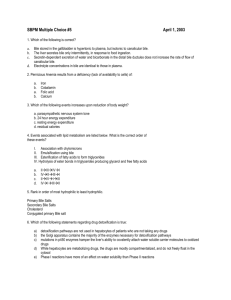
GI Physiology Resource 2 Problem Solving Exercises - Discussion 9 – 11 am, Tue Jan 24, 2012 E.S.Prakash, MBBS, MD Division of Basic Medical Sciences Mercer University School of Medicine Prakash_es@mercer.edu Follow-up Notes for this Resource will be available at http://esprakash.wordpress.com/2012/01/ from Thu Jan 26, as well as at Mercer Blackboard. License: This is an open access article distributed under the terms of the Creative Commons Attribution License http://creativecommons.org/licenses/by-nc/3.0/ which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, is properly cited. Primary objectives: • To provide formative assessment; • To provide examples of application of knowledge of physiologic mechanisms to clinical practice, and thereby to motivate learning • TOPICS Physiology and pathophysiologic aspects of: Liver and biliary system; Digestion and Absorption of Nutrients; Functions of Bile and Pancreatic Juice; Intestinal Motility; Electrolyte and Water Transport by the Intestine; Functions of the Colon Pathophysiologic mechanisms implicated in cholelithiasis • Lithogenic bile: lower in bile salts and lecithin and richer in cholesterol. – Defects in bile acid secretion in bile; – decrease in bile salt pool due to any cause; – E.coli secretes beta-glucuronidase that deconjugates bilirubin diglucuronide and bilirubin is insoluble and precipitates as calcium bilirubinate • Stasis of Bile in the biliary system due to any cause: total parenteral nutrition; prolonged fasting, denervation of gall bladder; obstruction in the biliary tract. • Excessive secretion of gall bladder mucins? Biliary sludge – a mix of cholesterol crystals, mucin, and calcium bilirubinate. Question 17 • A 32 year old pregnant woman in the third trimester of her pregnancy presents with a history of bothersome itching since the past 2 weeks. To begin with, itching was prominent in the palms and soles but it was now generalized. • Past history is notable for cholecystectomy done 3 years ago. • She is not on any medication. She is not jaundiced. • Physical examination is unremarkable. • Vital signs – WNL. She reported fetal movements and fetal heart rate was within normal limits. • S. Bilirubin (total), S. albumin, and prothrombin time were WNL. • Alkaline phosphatase - moderate elevation • -glutamyltransferase - mild elevation • What is the likely pathophysiologic basis of this presentation? • Issue – Transport of bile acids and bile salts by the hepatocyte Uptake of bile acids, bile salts, bilirubin and other organic species at the basolateral (sinusoidal membrane) of hepatocyte Transporter Function Na+ -Taurocholate Cotransporter Polypeptide (NTCP) Uptake of conjugated and unconjugated bile acids; note unconjugated BA also enter by nonionic diffusion Organic Anion Transporting Polypeptide (OATP); Na+ independent mechanism; anions exchanged for chloride from hepatocyte Uptake of bile salts, bile acids, organic dyes, steroid hormone conjugates, drugs, toxins and xenobiotics Organic Cation Transporter (OCT 1 and 2) Uptake of organic cations incl. aromatic and aliphatic amines, drugs, antibiotics, choline, thiamine and nicotinamide Secretion of bile salts, bilirubin, and other organic species at the canalicular membrane of hepatocyte Transporter Function Multidrug associated Protein (MRP-2); ATP dependent Secretion of conjugated bilirubin; defective in Dubin Johnson syndrome; note secretion is the rate limiting step in bilirubin metabolism by hepatocyte ABC transporter (ABCG5 / ABCG8) Cholesterol secretion into bile Multidrug Resistance Protein 1 (MDR 1) Excretion of organic cations and xenobiotics Multidrug Resistance Protein 3 (MDR 3) Flippase allowing extraction of lecithin by bile salts into micelles in bile Bile Salt Export Pump (BSEP) Secretion of Na & K salts of taurocholate and glycocholate. Loss of fx mutations result in a progressive decline in bile secretion and flow (intrahepatic cholestasis) Question 20 • Describe the pathogenesis of ascites in an individual with cirrhosis of the liver. PATHOGENESIS OF ASCITES IN CIRRHOSIS Splanchnic arteriolar dilation portal venules and hepatic sinusoids ↑ Portal vein pressure ↑ formation of lymph in the liver Hypoalbuminemia ↑ Resistance to blood flow through Retrograde transmission to splanchnic capillaries Dilation of portosystemic collaterals Ascites ↓ in effective arterial blood volume, cardiac output ↓ Renal blood flow Reflex ↑ renal sympathetic nerve activity Activation of renal renin-angiotensin-aldosterone axis and renal retention of Na, Cl and H2O (secondary hyperaldosteronism) Question 1 • How would you distinguish jaundice primarily due to cholestasis from that primarily due to hepatocellular disease? Hepatocellular vs. Cholestatic jaundice Note - Mixed patterns occur frequently MARKER PREDOMINANTLY HEPATOCELLULAR PATTERN PREDOMINANTLY CHOLESTATIC PATTERN S. Total Bilirubin Raised Raised S. conjugated Bilirubin Raised Raised Yes Yes S. Alanine aminotransferase S. Aspartate aminotransferase Urobilinogen in urine Raised Absent Color of Stools Normal Pale Urine bilirubin S. Alkaline phosphatase • Fourfold or greater elevation in alkaline phosphatase occurs especially in cholestatic liver disease. • The presence of elevation of serum 5 nucleotidase or γ-glutamyltransferase in combination with an elevated alkaline phosphatase strongly points to the liver as the source of these enzymes. Question 2 • Based on your knowledge of the anatomy and physiology of the digestive system, predict the consequences of resection of the terminal ileum on digestion and absorption of nutrients explaining the underlying mechanisms. Deficiency of Consequences Vitamin B12 Macrocytic anemia (may take years to develop) Bile salts Bile acid diarrhea: Bile acid induced secretion of Na and Cl in colonic epithelial cells (diarrhea); Steatorrhea: due to an eventual reduction in total bile salt pool and fat malabsorption Deficiency of fat soluble vitamins (A, D, E and K) Question 3 • A 50 year old man has undergone a cholecystectomy as part of management of acute cholecystitis. How would you expect cholecystectomy to impact on digestion and absorption of nutrients? • A mechanism for storage of bile is lost • Bile flow less precisely regulated • More bile flows into the duodenum during the interdigestive phase • A large amount of bile cannot flow quickly in response to CCK • Advise avoiding fatty meal Question 4 • You are examining a 50 year old male who underwent bowel surgery the previous morning. The patient is conscious, alert, and complains of a bloating sensation in the abdomen but reports no pain in the abdomen. He says he has not passed flatus since he has been awake. Percussion of the abdomen elicits a tympanitic resonant note, bowel sounds are consistently absent throughout the abdomen, and x-ray reveals distention of the small bowel and colon by pockets of gas and fluid. • What pattern of motility in the intestines is this consistent with? There are different ways of thinking and organizing our ideas about GI motility 1. 2. 3. Digestive versus interdigestive motility Propulsive movements versus mixing movements Anatomical: motility in the stomach versus that in the duodenum versus that in the proximal colon. BER frequency varies from region to region. SMALL INTESTINAL MOTILITY IN THE DIGESTIVE PHASE INTESTINAL MOTILITY IN THE DIGESTIVE PHASE Segmentation contractions – Migrating Motor Complex (MMC) from allow greater exposure of mucosa mid-stomach to ileum; once every 90 to chyme and foster absorption min; house keeping functions. Followed by peristalsis PROPULSIVE MOVEMENTS Peristalsis (digestive phase) Migrating Motor Complex (interdigestive phase) Mass action contractions (simultaneous contraction of large confluent areas of colon – say entire transverse and descending colon; occur only in the colon; 2-3 times per day; induce the desire to defecate MOVEMENTS THAT PRIMARILY CAUSE MIXING OF CHYME AND FOSTER ABSORPTION OF NUTRIENTS Segmentation contractions (in small intestine) Haustral shuttling (in large intestine) In this Question • Abdominal distention + no abdominal pain + tympanitic resonant note + individual has not passed flatus as yet + bowel sounds absent + x-ray shows intestines distended by pockets of gas and fluid • • • • • Paralytic ileus (postoperative ileus in this case) Mechanism: Ileus is a reflex response to injury to peritoneum and abdominal viscera; sympathetically mediated Hypokalemia is a risk factor for ileus Recovery occurs within 2-3 days in the absence of complicating factors Until then decompress the lumen with a nasogastric tube; and nil per oral Question 5 • How would you distinguish whether diarrhea in an individual is primarily due to increased secretion of electrolytes and water, or due to abnormally large amounts of an ingested and unabsorbed osmole in the intestinal lumen? SECRETORY DIARRHEA Diarrhea due to an abnormally elevated secretion of Na and Cl and consequently water by epithelial cells in crypts. OSMOTIC DIARRHEA Diarrhea primarily due to the presence in the lumen of large amounts of an unabsorbed osmole (other than Na and Cl) Does not cease with fasting Ceases with fasting or when the offending osmole is not ingested Stool osmotic gap: normal Measured osmolality of stool is 50 mOsm / Kg H20 than the expected (or calculated) osmolality of stool. Question 6 • Based on your knowledge of the cellular mechanisms of secretion of Na and Cl and water by intestinal epithelial cells, propose a pharmacologic strategy for controlling secretory diarrhea. • In the Small Intestine: Note distinction between the functions of villus cells vs. those in crypts. • In the Large Intestine: There are no villi; note the distinction between surface epithelial cells and cells in crypts. • Crypt cells – predominantly secretion of Na and Cl • Villus cells; surface epithelial cells – primarily reabsorption of electrolytes Mechanism of Na and Cl secretion by intestinal crypt cells for details, see the next 2 slides ClTight junctions Na+ H2O GI Lumen __ CFTR ++ PKA enterocyte cAMP Na-K-2Cl Basolateral m. Na+ H2O Intestinal capillary +++ Description for the schematic on the previous slide; note the following: 1. Tight junctions linking apical membranes of enterocytes; 2. PKA activates CFTR (cystic fibrosis transmembrane regulator - a chloride ion channel in the apical membrane of crypt cells); 3. Chloride enters enterocytes from interstitium by NaK-2Cl symporter; Continued.. 4. Chloride passes down a transepithelial gradient through chloride ion channels (CFTR) in the luminal membrane and into the GI lumen; 5. This makes lumen in the crypts about 10 mV negative (transepithelial potential difference) with respect to interstitial fluid; 6. Na+ leaks via tight junctions (they aren’t really as “tight”) because the lumen is negative with respect to interstitial fluid. 7. Water enters lumen from interstitial fluid (driven by the NaCl rich luminal content in the crypt lumen; i.e. driven by osmotic gradient) Question 7 • Your patient is a 60 year old woman with clinical evidence of malabsorption – a chronic history of bulky, malodorous, greasy stool, and documented steatorrhea. • Prothrombin time is elevated (INR – 2). • Results of the D-xylose test are normal. • There is no histologic evidence of villous atrophy in the duodenum. • The patient is not on any medication. • He has not undergone any surgeries in the past. • What further investigations will allow us to identify the mechanism of malabsorption? • Since D-xylose does not require digestion before absorption in the small intestine, a ‘normal D-xylose test’ makes extensive mucosal disease of the small intestine test less likely. Evaluating bile sufficiency; sufficiency of bile salts and conjugated bile acids in bile • Do clinical and radiologic data provide evidence suggestive of extrahepatic cholestasis? • Is there evidence for cholestasis such as a combination of 3-4 fold ALP, γ-glutamyltranspeptidase; conjugated hyperbilirubinemia; lack or of urobilinogen in urine? Causes Mechanisms Extensive liver cell disease Decreased synthesis of bile acids and bile salts Specific defects in hepatocyte excretion of bile acids and salts Intrahepatic cholestasis; biliary cirrhosis Excessive deconjugation of bile salts and bile acids in the jejunum Bacterial overgrowth in small bowel; jejunal diverticulosis Disease or resection of terminal ileum Diminished bile salt pool in the long run Evaluating exocrine function of the pancreas Test Description Secretin Test Hormone(s) given IV; pancreatic juice – volume, HCO3 & or trypsin output assessed by duodenal intubation; sensitive to mild, moderate or severe exocrine pancreatic dysfunction. CCK Test Secretin – CCK Test Lundh test meal Measurement of duodenal trypsin after oral ingestion of a liquid test meal. Fecal fat Insensitive for detecting mild-moderate exocrine dysfunction Fecal chymotrypsin Fecal elastase N-benzoyl tyrosyl p- Oral ingestion of NBT-PABA with a meal followed aminobenzoic acid by measurements of PABA in serum or urine; cleavage of NBT-PABA requires chymotrypsin Question 8 • Does severe (NYHA class IV) heart failure predispose to invasive infections of the intestine? Explain. Decreased cardiac output Decreased blood pressure (perfusion pressure) Decreased mesenteric blood flow; also sympathetic activation in heart failure reduces splanchnic blood flow If splanchnic autoregulation overwhelmed Then Mucosal hypoxia Contd. Villus necrosis (tips of villi are most susceptible to hypoxia) Entry of luminal pathogens & toxins into blood stream Septicemia Teaching point: • Importance of splanchnic blood flow illustrated • Importance of defense function of intestinal mucosal barrier illustrated 31 Question 9 • A 65 year old man presents with a history of loose stools since the past 2 years. Other symptoms included flushing, weight loss and severe weakness. • Until then, his bowel habits have been essentially normal. He denies taking laxatives. • He has been previously hospitalized at least on three occasions over the past 4 months for management of acute renal failure. Question 9 (contd.) • Further findings of note were: – – – – – diarrhea did not cease with fasting; plasma [K+] = 2.8 mM (normal 3.5-5.5 mM); basal acid output = 1 mmol/h (normal avg. 3 mmol/h) osmotic gap in stool was normal. colonoscopy did not reveal any abnormality. • Further investigations revealed the presence of a tumor in the pancreas. Additionally there were metastases in the liver. • What is the most likely etiology of the diarrhea? Propose a pharmacologic strategy for alleviating it. • VIP secreting tumor (VIPOma; Verner – Morrison Syndrome; pancreatic cholera) Effects of VIP (in large doses) • Increases blood flow to the intestine • Increases secretion of Na, Cl and water by the intestine (watery diarrhea) • Relaxes intestinal smooth muscle • Peripheral vasodilation (flushing) • Inhibition of gastric acid secretion (achlorhydria) Question 10 • An 65 year old man has had to undergo near-total colectomy as part of management of colorectal cancer. Based on our knowledge of the functions of the small intestine and large intestine, what would would you expect the short-term and long-term consequences of extensive resection of the large intestine to be? Functions of the colon • Length of colon: approx 3.5 ft (in living humans, measured by intubation); contrast – small intestine is about 9.5 ft long. • In the healthy adult, the colon is presented with about 2 liters of fluid per day; its capacity for absorption of Na, Cl and H2O is greater than this [about 4 L/day]… • Normal water output in stool? • Normally, there is net secretion of K and HCO3 in the colon. • Undigested or unabsorbed carbohydrate escaping into colon are metabolized to short-chain fatty acids (SCFA) by colonic bacteria; • Examples – acetate, propionate, butyrate • These are absorbed by colonic epithelial cells • SCFA somehow are said to increase Na and Cl absorption by colonic epithelial cells. • This may be affected when colonic bacteria are altered by antibiotic therapy, and may be one mechanism of antibiotic associated diarrhea. • Intestinal adaptations following colectomy – If fluid balance and electrolyte balance is maintained, – volume of ileal discharge decreases over time.