CV Assessment
advertisement

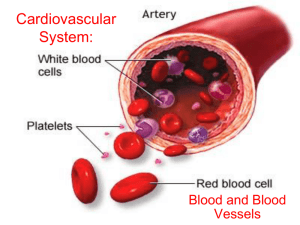
ASSESSMENT OF CARDIOVASCULAR FUNCTION NUR240 Lecture 1 J. Borrero 9/10 1 LECTURE OBJECTIVES 1. Review anatomy & physiology of the cardiovascular system. 2. Discuss relevant aspects of the patient history. 3. Describe physical assessment of cardiovascular status. 4. Review diagnostic procedures, tests and medications relative to the cardiovascular system. 2 Anatomy & Physiology (What makes it “tick”!) Functions of the heart & CV system • Pumps blood to tissues to supply O2 & nutrients • Remove CO2 & metabolic wastes 3 Anatomy & Physiology CARDIAC CELLS HAVE UNIQUE PROPERTIES • AUTOMATICITY CELLS CONTRACT INDEPENDENTLY (THEY INITIATE THEIR OWN IMPULSE) • EXCITABILITY ION SHIFT • CONDUCTIVITY TRANSMIT IMPULSE TO ANOTHER CARDIAC CELL • CONTRACTTILITY HOW WELL THE CELL CONRACTS 4 Anatomy & Physiology PERICARDIUM / PERICARDIAL SAC • Protects heart from trauma • Serous fluid lubricates and prevents friction • Prevents heart from over filling 5 CIRCULATION PATHWAY HEART IS DIVIDED INTO TWO SIDES RIGHT & LEFT ALL BLOOD RETURNS TO THE HEART THROUGH THE ATRIA ALL BLOOD LEAVES THE HEART FROM THE VENTRICLES 6 CORONARY ARTERIES • Supply blood to MYOCARDIUM • BRANCHES: LEFT MAIN CORONARY ARTERY L ANTERIOR DESCENDING (LAD) L CIRCUMFLEX (LCX) RIGHT CORONARY ARTERY POSTERIOR MARGINAL 7 CORONARY ARTERIES (L) ARTERY CIRCUMFLEX (R) LAD ARTERY 8 CONTRACTION OF CARDIAC MUSCLE The heart can’t pump unless an electrical stimulus occurs Action Potential (AP) – electrical change (depolarization = contraction) Brought about by release of calcium (+ charge) into cells Intrinsic Pacemakers – depolarize and generate the AP 9 CONTRACTION OF CARDIAC MUSCLE The pacemaker with the fastest rate of depolarization stimulates the AP • SA node (60-100 bpm)- Upper R atrium • AV node (40-60 bpm)- Lower R atrium • Other pacemakers ( 40) 10 DISRUPTION IN SERUM ELECTROLYES CAN RESULT IN ALTERATION IN CARDIAC CYCLE • K, Ca & Mg lead to dysrhythmia, weakness • Ca leads to strength of contraction • Na leads to general weakness & less Na to initiate action potential • K leads to dysrhythmias 11 MONITORING MOVEMENT OF THE CRDIAC ACTION POTENTIAL (AP) • EKG – monitors the movement of the AP, the electrical changes NOT the mechanical changes that follow • Auscultating heart sounds, palpating pulses and measuring pressures monitor the mechanical changes 12 CARDIAC CYCLE CARDIAC CYCLE – all the activities occurring in the heart during one contraction, and subsequent period of relaxation. Graphically represented on an EKG (ECG) 13 CARDIAC CYCLE EKG – A 12 lead EKG is a graphic record of the electrical forces produced by the heart 14 CARDIAC CYCLE Part of Cycle Representation P wave PR Interval QRS Complex ST Segment T Wave R-R Interval 15 CARDIAC CYCLE Polarized (resting) cell – represented on EKG as baseline or isoelectric line Depolarization – impulse over specialized cardiac cells (not neuromuscular impulse) Repolarized cell – returns to normal. Na moves out of cell, K moves in – requires ATP Note: ischemic tissue may cause problem 16 ELECTRODE POSITIONS “LEADS” • Leads measure electrical activity between 2 points • Movement toward electrode causes positive deflection • Movement away from electrode causes negative deflection 17 ELECTRODE POSITIONS A 12 Lead EKG shows electrical activity from 12 different positions in the heart, concentrating on (L) ventricle A 14 Lead EKG includes (R) ventricle activity 18 STROKE VOLUME (SV) & CARDIAC OUTPUT (CO) • SV – amount of blood ejected by 1 ventricle in 1 beat • CO – volume ejected in 1 min Control of SV and HR = SV&HR are continually adjusted by the body, and are affected by the return of blood from the tissues (think of exercise) CO = SVxHR 19 STROKE VOLUME (SV) & CARDIAC OUTPUT (CO) Extrinsic control of HR is a more powerful way of controlling CO than changing SV 1. CVP causes stretching of (R) atrial muscle which stimulates SNS & HR (to help pump all the blood returned to it) 2. Remember “Starling’s Law” 20 STROKE VOLUME (SV) & CARDIAC OUTPUT (CO) 2. Stretch baroreceptors (aorta & carotid) detect in pressure which stimulates SNS & HR (to ensure adequate blood supply to heart/ brain) 3. If pressure detected, then PSNS is stimulated & HR is slowed (vagus nerve) (prevents excess arterial pressure which can damage organs) 21 CARDIAC LOAD Preload = degree of myocardial fiber stretch at the end of diastole and just before contraction Afterload = pressure against which ventricles must eject blood. This pressure is affected by systemic vascular resistance (SVR) 22 23 CARDIAC ASSESSMENT Cardiac status of all patients should be routinely assessed. Everyone has a 1. Subjective CP Dyspnea Fatigue 1. Objective 24 IMMEDIATE NURSING INTERVENTIONS FOR ACUTE CARDIAC EVENT MOVIE Acronym M- Monitor for pain O- O2 and pulse ox V- Vital signs I- Intravenous fluids E- EKG monitoring Anything else?? 25 Pain Assessment SLIDA or Precipitating/alleviating factors Quality Radiation Severity Timing 26 OTHER ELEMENTS OF CARDIAC ASSESSMENT • Previous cardiac hx • Other medical conditions that may affect heart function • Chest injury • Previous heart surgery • Past medical hx • Medications: prescribed, OTC, herbals • Activity tolerance • Health habits • Family hx 27 EXAMINATION • • • • Inspection Palpation Percussion-? Auscultation = S1, S2 at PMI Aortic Pulmonic Tricuspid Mitral 28 Heart Rhythm Regular, Irregular, Regular Irregular Abnormal Sounds: Gallops Murmurs Bruits S3 ventricular gallop – heard in early diastole S4 atrial gallop – generally abnormal 29 Assessment of Murmurs Turbulent blood flow in valvular disorders and septal defects Timing of murmurs is a must! Systolic murmurs occur between S1 & S2 Diastolic murmurs occur between S2 & S1 Grade 1 – 6 identifies intensity of murmur 30 31 Other assessments • Jugular vein pressure – assess JVD which reflects increased filling volume and pressure on (R) side of heart JVD associated with (R) HF, SVC obstruction (Normal is 3-10cm H20) • Pulse deficit – the difference between apical HR and peripheral pulse-associated with Afib, and heart blocks • Pulse pressure – the difference between systolic & diastolic pressure 32 Other assessments • Respiratory: Lung sounds = rate, rhythm, quality, sputum • GI-Abdomen • Peripheral Vascular:Lower extremities 33 Diagnostic Procedures 1. EKG 12 Lead continuous cardiac monitoring holter monitor 2. Chest x-ray – detects enlargement of heart & pulmonary congestion 34 Diagnostic procedures 3. Echocardiography – ultrasound that reveals size, shape and motion of cardiac structures Evaluates heart wall thickness, valve structure, differentiates murmurs 4. TEE – transesophageal echocardiography provides a clearer image because less tissue for sound waves to pass through 35 Diagnostic procedures 5. Angiography / cardiac catherization determines coronary lesion size, location, evaluate (L) ventricular function, measures heart pressures 6. Exercise tolerance test 7. Radionuclide Imaging 36 Lab Studies Cardiac enzymes = enzymes are released when cells are damaged (MI). Enzymes are found in many tissues/muscles, and some are specific to cardiac tissue. Serial measurement can aid in dx, and monitor course of MI Cardiac enzymes = CPK – MB (CK-MB),myoglobin, Troponin In general, the greater the rise in the serum level of an enzyme, the greater the degree or extent of damage to the muscle. LDH 37 Blood studies 2. 3. 4. 5. 6. Electrolytes Lipid panel CBC C – Reactive Protein BNP- Human B-Natriuretic Peptide 7. Blood coags-PT/PTT/INR 38 Lipid Panel Desirable Total Under 200 Cholesterol LDL Under 130 HDL 30-80 Triglycerides 40-150 Borderline High 200-239 High 130-159 160 or > 240 or > Elevated levels neg correlated with CAD and may be protective 39 C Reactive Protein Hs-CRP Level Risk < 1.0mg/L Low risk of CVD 1.0-3.0 mg/L Average risk of CVD >3.0 mg/L High Risk of CVD 40 NCLEX TIME Mary is attending a sophomore level nursing class on anatomy and physiology. Which statement, if made by Mary, demonstrates a good understanding of the anatomy and physiology of the heart? A."The heart is encapsulated by a protective coating called the endocardium.“ B."The SA node is considered the main regulator of heart rate.“ C."The left atrium receives deoxygenated venous blood from all peripheral tissues.“ D."Stroke volume is the amount of blood ejected by the right ventricle during each diastole 41 NCLEX TIME Kirsten is completing her graduate clinical rotation in a large urban teaching hospital in a medical coronary care unit (CCU). Which observation demonstrates a good understanding of completing a thorough cardiac examination? • A. In an obese client, an adult cuff size of 12 to 14 cm is preferable. • B.The carotid artery on the neck is auscultated to assess for the presence of a bruit. • C.The apical impulse is auscultated over the fifth intercostal space in the midclavicular line. • D.Palpation is used to determine cardiac size. 42 NCLEX TIME Edward is a 40-year-old white male. He is an accountant who works on average 11 hours per day. He reports feeling stressed each day, even with mundane things such as a traffic jam. His father had a massive myocardial infarction at the age of 48. His mother has a history of congestive heart failure. He seldom has time to exercise, but does eat balanced meals when possible, although he does not get to eat three meals a day. Select all factors that place Edward at risk for heart disease. • A.Family history • B.Age • C.Coping-stress tolerance • D.Race 43 • E.Occupation