Introduction to Health Informatics
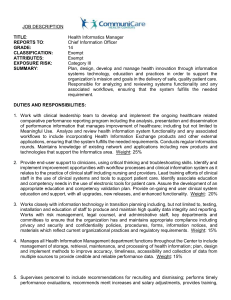
advertisement

Developments in Nursing Practice Introduction to Health Informatics Informatics Informatics includes the science of information, the practice of information processing, and the engineering of information systems. Informatics studies the structure, behavior, and interactions of natural and artificial systems that store, process and communicate information. It also develops its own conceptual and theoretical foundations. Since computers, individuals and organizations all process information, informatics has computational, cognitive and social aspects, including study of the social impact of information technologies. 1. What is health informatics? From the French ‘informatique’ Medical informatics, medical computing, computers in medicine,…. Interdisciplinary field combining health sciences, computer science, statistics, engineering, management sciences,… Many definitions…. Some definitions of health informatics ‘an umbrella term referring to the application of the methodologies and techniques of information science, computing, networking and communications to support health and health related disciplines such as medicine, nursing, pharmacy, dentistry etc……’ WHO ‘ the field that concerns itself with the cognitive, information processing, and communication tools of medical practice, education, and research including the information science and the technology to support these tasks’ (Shortliffe) ‘ Nursing informatics Nursing informatics is the integration of nursing, its information, and information management with information processing and communication technology, to support the health of people world wide . Nursing Informatics is a specialty that integrates nursing science, computer science, and information science to manage and communicate data, information, and knowledge in nursing practice. Who does health informatics serve? Patient Medical Profession Government Bodies Primary Care/GP’s National Agencies Finance/Admin. Management in Hospitals Tax Payers General Population The public Policy makers (strategic management) Regional managers/tactical management Facility management/operational management Health care providers Healthcare researchers Healthcare educators and their students Will one solution suit all? What services does Health Informatics involve? Data processing – (health is a data intense industry) Includes collection, processing, transformation, presentation & use Communication – main emphasis should be on supporting communication between people Knowledge based services Includes computerised bibliographic services, on-line collections on non-numerical information such as practice guidelines, pharmacopoeias, essential drug lists, telephone directories, expert, decision-support and reminder systems What technologies does it employ? Computers and networks…… But don’t forget paper-based information systems, including input to and output from the computer Applications of Health Informatics For recording accurate data To have data available in a timely manner Support and inform managers to make better decisions Resource allocation and planning Email therapy Risk management Training Support for shared care Patient Assessment Evaluation of patient care Monitoring patients Staff coordination Tracking patients in hospital Stock management Tracking sterile supplies Integration engines Mobile computing Applications of Health Informatics contd. Drug control – medication dispensing/ordering Purchasing equipment Payroll Clinical Pathways Labour management Patient scheduling Budget analysis Research Word processing National database Quality Assurance Donor databases Devices Monitors Analysers Imaging equipment Imaging systems in Health Impossible without the use of computers Computers are used to: Construct an image from measurements Obtain an image reconstructed for optimal extraction of a particular feature from an image Present images Improve image quality by image processing Store and retrieve images Ulstrasound, x-rays, computed tomography, MRI, nuclear imaging etc. …. Telehealth Telehealth is the delivery of health-related services and information via telecommunications technologies. Telehealth delivery could be as simple as two health professionals discussing a case over the telephone, or as sophisticated as using videoconferencing to between providers at facilities in two countries, or even as complex as robotic technology. Telehealth is an expansion of telemedicine, and unlike telemedicine (which more narrowly focuses on the curative aspect) it encompasses preventive, promotive and curative aspects. Originally used to describe administrative or educational functions related to telemedicine, today telehealth stresses a myriad of technology solutions. For example, physicians use email to communicate with patients, order drug prescriptions and provide other health services. Clinical uses of telehealth technologies Transmission of medical images for diagnosis (often referred to as store and forward telehealth) Groups or individuals exchanging health services or education live via videoconference (real-time telehealth) Transmission of medical data for diagnosis or disease management (sometimes referred to as remote monitoring) Advice on prevention of diseases and promotion of good health by patient monitoring and followup. Nonclinical uses of telehealth technologies Distance education including continuing medical education, grand rounds, and patient education Administrative uses including meetings among telehealth networks, supervision, and presentations Research Online information and health data management heathcare system integration patient movement and remote admission Telehealth modes Telenursing Telenursing refers to the use of telecommunications and information technology for providing nursing services in health care whenever a large physical distance exists between patient and nurse, or between any number of nurses. As a field it is part of telehealth, and has many points of contacts with other medical and nonmedical applications, such as telediagnosis, teleconsultation, telemonitoring, etc. eHealth eHealth (also written e-health) is a relatively recent term for healthcare practice which is supported by electronic processes and communication. The term is inconsistently used: some would argue it is interchangeable with health care informatics and a sub set of Health informatics, while others use it in the narrower sense of healthcare practice using the Internet. The term can encompass a range of services that are at the edge of medicine/healthcare and information technology Electronic Medical Records: enable easy communication of patient data between different healthcare professionals (GPs, specialists, care team, pharmacy) Telemedicine: includes all types of physical and psychological measurements that do not require a patient to travel to a specialist. When this service works patients need to travel less to a specialist or conversely the specialist has a larger catchment area. Evidence Based Medicine: entails a system that provides information on appropriate treatment under certain patient conditions. A healthcare professional can look up whether his/her diagnosis is in line with scientific research. The advantage is that the data can be kept up-to-date. Consumer Health Informatics (or citizen-oriented information provision): both healthy individuals and patients want to be informed on medical topics. Health knowledge management (or specialist-oriented information provision): e.g. in an overview of latest medical journals, best practice guidelines or epidemiological tracking. Virtual healthcare teams: consist of healthcare professionals who collaborate and share information on patients through digital equipment . 3. Why bother? Information Technology is now an integral and essential part of health delivery IT systems are prevalent in society Training and education in the appropriate application of IT in healthcare essential - Council of Europe 4. Health sector today (citizen-centred care) Health and education are two major consumers of the public purse Situation in the sector Cost containment Information overload (data doubles every five years) Shared care (team based care) Technological push vs. demand pull (users driving it) Clinical focus - Should be driven by supporting clinical needs and not financial management (otherwise solutions in search of problems) Cost containment is major driving force – planning resources (eg. cost of care for diabetes) Improving quality of care equally important Health sector today contd. Distributed organisational structures (independent clinics/labs) – strong local autonomy Accountability Increased dependence on automation Emphasis is moving from administrative to clinical information systems Public has more knowledge about healthcare (NLM, Medline, Web) Tension between demand for increased quality of care vs. reduction in costs Efficiency vs. cost-effectiveness Health sector today contd. Information overload – nos., text, x-rays, ultrasounds Complex (narrative) Distributed Multi-vendor (heterogeneous) – no one vendor can support all the processing needs of all systems, GP, A&E Strong autonomy (need to relinguish a certain amount of automony to share data) Data intensive Implications for healthcare organisations Unnecessary duplication of tests and investigatons Valuable time wasted trying to track down relevant information Studies have shown that at least 20% of healthcare professionals time is spent reading, writing, sorting and searching through notes (up to 70% has been claimed by some) =>Appropriate healthcare not provided as efficiently and cost effectively as possible The strategy to improve the situation should include the following ideas.. Patient care requirements prime Secure, reliable, on-line clinical information systems Facilitate cost-effective use of IT Establish stewardship for implementation of enterprisewide solutions and standards Connect and manage distributed information systems Delivering healthcare today is no longer the sole responsibility of a single professional Movement away from hospital (tertiary) to community (primary) – based shared care (Access to records by GPs) This implies…. Ability to share information between care providers is key The right information in the right place, in the right format and at the right time IT is key-enabling technology for shared care Tension between demand for increased quality of care vs. reduction in costs Efficiency vs. cost-effectiveness The key issue is…… Efficient and cost-effective application of ICT in the health sector 6. Challenges…. Legacy information systems (older systems) Problems – Maintenance 80% of IT costs (eg Y2K problems) Inflexible and brittle (cannot interface with newer systems – can crash/old code not properly documented (cannot interface with new systesm) Fear Challenge Migrate/evolve IT gets in the way sometimes Technical Challenges contd. Complex nature of medical data Alphnumberic (lab results) Text (discharge summary) Signals (monitors) Images (x-rays) Video (endoscopy, ultrasound) User interfaces – data entry Highly reliable, efficient and secure information management Integration of IT into routine clinical practice – paperless hospital Co-operative hospital computing Multi-vendor What are the Organisational Challenges Integrating IT into the business process Understanding the domain to which the application is being applied Training Staff on the new systems Introducing the new systems to patients Maintenance of the systems Resources – location, staff, money