Management of Malaria – Dr M Ridwanur Rahman
advertisement

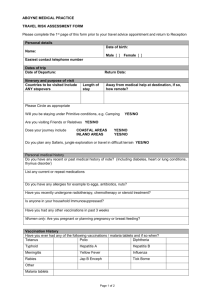
Management of Malaria Dr M Ridwanur Rahman Professor (Medicine), ShSMC, Dhaka Member, Malaria Research Group, Ctg THE BURDEN OF MALARIA >100 countries in the world are malarious >2 billion people are exposed to the risk of malaria infection annually. Residents of non-endemic areas also have, Travel malaria Airport malaria High Risk Groups Young children (6 months - 5 years) -Pregnant women (primigravids) -Non-immune migrants (Military personnel, expatriates, tourists, refugees). High Risk Malaria Areas in Bangladesh Case Load: Malaria in Bangladesh, 1963 – 1998 Clinical Malaria - Treatment Non falciparum malaria- Uncomplicated Uncomplicated Malaria (falciparum) Severe (Complicated) Malaria Malaria Case Fatality Rates Severe malaria 10-40% Moderately severe malaria 3% Uncomplicated malaria <1% Relationship between life cycle & clinical features Cycle/feature Vivax/ovale Malariae Falciparum Incubation 8-25 days 15-30 days 8-25 days Asexual cycle 48 hrs, synchronus 72 hrs, synchronus <48 hrs, asynchronus Periodicity of fever Tertian Quartan Aperiodic Exoerythrocytic Persist as hypnozoites None None Delayed onset common rare Rare Relapses Common upto 2 years Recrudescence many years Recrudescence upto 1 year Clinical Features Fever- classically intermittent & periodic 3 stages described Asymptomatic apyrexial intervals Malaise, Headache, bodyache & vomiting Cough & mild diarrhoea- children Jaundice relatively common- falciparum No specific physical sign Liver & spleen- enlarge & tender Anaemia frequent in falciparum D/D in uncomplicated disease Flue like illness’ Enteric fevers RTI’s UTI Dengue SSTI Others Diagnosis High index of suspicion- H/O chance of contact, absence of symptom/signs of other disease, characteristic C/F Blood slide examination Dipstick Tests Other tests- to exclude other D/D, e.g., urine R/M/E, CBC, CXR etc. Classification of antimalarial drugs based on chemical structures 4-aminoquinolines e.g. chloroquine, hydroxychloroquine, amodiaquine 8-aminoquinolnes e.g. primaquine 2,4-diaminopyrimidine e.g. pyrimethamine Arylaminoalcohols e.g. quinine, mefloquine, lumefantrine Acridine derivatives e.g. quinacrine, mepacrine, pyronaridine Biguanides e.g. chloroguanide, chloroproguanil Suphonamides and sulphones e.g. sulphadoxine and dapsone respectively Phenanthrene methanols e.g. halofanthrine Naphthoquinones e.g. atovaquone Artemisinins e.g. dihydroartemisinin, artesunate, artemether, arteether, e.t.c. FACTORS THAT GOVERN CHOICE OF DRUGS Parasite species Local Level of resistance to drugs Patient’s general health and medical history. Availability of medication in the country of prescription. Intended use (prophylactic or therapeutic). Drug resistant Malaria Resistance is the ability of an organism to survive or multiply despite presence of the drug – exhibited by falciparum only CQ, S/P resistance in Bangladesh May have reduced sensitivity to Q & M Bangladesh is a multi-drug resistant falciparum area Factors aiding Resistance in malaria parasites. Indiscriminate drug use Sub-optimal dosages Non compliance with treatment course Low quality drugs Fake and substandard drugs WHO Treatment Guidelines Artemisinin-based Combination Therapies (ACTs) should be first line treatment for falciparum malaria everywhere. This should ideally be formulated in fixed dose combinations when possible. Therapeutic options for ACT -Artesunate-SP -Artemether-lumefantrine -Artesunate-amodiaquine -Artesunate-mefloquine -Dihydroartemisinin-piperaquine What are Artemisinins ? Artemisinin derivatives Dihydroartemisin Qinghaosu ("ching-how-soo") Ethyl Ether Methyl Ether Arteether Artemether Hemisuccinate Artesunate First demonstration project in Thailand Treatment efficacy at Thai-Burmese border Cured (%) 100 Mefloquine + artesunate 80 Mefloquine25 Mefloquine15 60 19 Year 99 19 98 19 97 19 96 19 95 19 94 19 93 19 92 19 91 19 90 19 85 -8 6 40 Artemisinin-based combination therapy in uncomplicated malaria Widespread use of 1st line Rx with Artemisinin-based Combination Therapy Improve clinical cure rates Delay emergence of resistance Reduce transmission Cost effective Treatment of Uncomplicated Malaria Non-Falciparum- - Chloroquine 25 mg/kg over 3 days, (Tab 4-4-2, adults) - & primaquine 15 mg/d, 14 days Falciparum- ACT Co-artem - 6 doses 2nd line- Alternative ACT, Q7T7 or Q7D7 What to give in pregnancy ? In 1st trimester Quinine + Clindamycin 7 days In 2nd and 3rd trimesters Any ACT combination as per rec. or Artesunate + Clindamycin 7 days or Quinine + Clindamycin 7 days Lactating women same ACT CLASSIFICATION OF THERAPEUTIC RESPONSE (WHO 2004) 3 Categories Early treatment failure (ETF) Late treatment failure (LTF) Late clinical failure Late parasitological failure Adequate clinical and parasitological response (ACPR) Severe & Complicated Malaria (SCM) Falciparum malaria Children, pregnant & short term travel/resident – endemic zones Severe symptoms Life threatening in the absence of early effective treatment Medical emergency Table-1 Types of Severe Manifestations (n=829) Type SCM (Major) Full Recovery Death N (%, CFR) Others 2 Total N (%) CNS Manifestations 304 39 (31) 19 362 (44) 36 (27) 10 132 (16) 2 (1) 8 195 (24) 1 (3) 1 35 (4) Unrousable Coma 86 Impaired Consciousness 185 Convulsion 33 Severe Prostation 193 0 4 197 (24) Hyper-parasitaemia 172 0 6 178 (22) Severe Anamia 51 0 16 67 (8) Hyperpyrexia 14 1 (7) 0 15 (2) Others 7 0 3 10 Total n (row%) 741 (89) 40 (4.8) 48 (6) 829 SCM – Other Manifestations Acute renal failure Pulmonary Oedema Haemoglobinuria Hypoglycaemia DIC Jaundice Multi-organ involvement/failure May occur singly, often in combination Management (SCM) • Medical Emergency • Appropriate anti-parasitic Treatment • Crucial General Management • Identification & management of complications Treatment of severe falciparum malaria Any of the following antimalarial medicines are recommended – Artesunate i.v. or i.m – artemether i.m. – quinine (i.v. infusion or i.m. injection). Full course of ACT or quinine + clindamycin or doxycycline when patient can tolerate oral treatment Artemisinins parenteral αβ Arteether – 150 mg (2ml) i.m od x 3 days or 3 mg/kg od i.m. x 3 days Artesunate 2.4 mg/kg i.v. or i.m. given on admission (time = 0), then at 12 h and 24 h, then once a day Artemether 3.2 mg/kg i.m. given on admission then 1.6 mg/kg per day is an acceptable alternative to quinine i.v infusions Rectal artemisinins are not as effective Quinine parenteral A loading dose of quinine of 20 mg salt/kg bw. 10 mg/kg 8th hrly i.v infusion Rate-controlled i.v. infusion is the preferred route of quinine admin. If this cannot be given safely, then i.m. injection is a satisfactory alternative. Rectal admin. is not effective Quinidine can substitute quinine Quinine vs Artemesinin’s • Artemesinins are more effective than Quinine in terms of survival (MRG, contributed) • No significant difference in coma resolution time & fever clearance time • Parasite clearance time faster with A’s • Hypoglycaemia & cardiotoxicity less A’s • ? Uterine contractions more with Q’s • ? Neurologic sequelae more with A’s (animals) Cerebral Malaria – D/D Meningitis Encephalitis Sepsis Fever in CNS Disease Fever in Organ failure Typhoid encephalopathy Metabolic/Toxic encephalopathy Severe Anaemia • More in children & pregnant population • Transfuse if Hb <6.0 g/dl • Fresh whole blood or packed cells • Include the transfusion volume in I/O calculation • Use frusemide if volume over load Acute Renal Failure • • • • Continuous Catheter Correct dehydration Use bolus frusemide 20-40 mg IV Monitor hourly urine output, if <17 ml/hr established ARF • Control fluid input if established ARF • Referral to renal replacement facility • Pt. Unlikely to die if dialysis facility available Hypoglycaemia • Frequent in young children, pregnant women & during quinine Rx • Intervened on suspicion- most important being deterioration of consciousness & convulsion • Bolus 25% glucose 50 cc • Follow with IV infusion of 5%/10% glucose • Continue monitoring for recurrence Metabolic Acidosis • • • • Look for dehydration & hypovolaemia Isotonic IV infusion, avoid fluid overload Monitor BP, urine volume & JVP Improve oxygenation by - clearing airway - oxygen inhalation - support ventilation, if necessary Pulmonary Oedema • Very serious, mortality >50% • Frequent in ARF, pregnancy, severe anaemia, & at extremes of ages • Prop up position & oxygen inhalation • Stop IV fluid & give IV frusemide (40-200 mg) • Sequential torniquette application • Haemofiltration • Mechanical ventilation • Withdraw blood by venesection Circulatory Collapse • Often associated with gm –ve septicaemia • Common sites- lung, urinary tract, meningitis, IV lines & injection sites • Take blood culture, start broad-spectrum antibiotics (Amoxy + Genta) • Maintain adequate hydration & output • Dopamine may be given Spontaneous bleeding & DIC • Spontaneous bleeding from DIC is uncommon but serious complication • Thrombocytopenia is common but rarely causes bleeding • Transfuse fresh blood, clotting factors or platelets as required • If PT or PTT prolonged, Inj. Vit. K 10 mg may be given Haemoglobinuria • G6PD deficiency or malaria itself- not quinine • Continue appropriate antimalarial if parasitaemia present • Transfuse fresh whole blood to Hct >20% • Monitor JVP/CVP to avoid fluid overload & hypovolaemia • Give frusemide 20 mg IV • Monitor renal function & consider dialysis if required Nursing Care • As important as anti-parasitic Rx • Meticulous nursing care to - maintain clear airway - prevent aspiration pneumonia - prevent pressure sores • Careful intake-output chart • Rate of infusion checked frequently • Temperature >1020F reduced by tepid sponging & fanning • Change in level of consciousness, behaviour & occurrence of convulsion reported SCM Management – Common errors Misjudgement of severity Delay in starting treatment Failure to provide nursing care Inappropriate rate of infusion Delay in correcting hypoglycaemia Failure to control convulsions Unnecessary continuation of treatment Failure to evaluate con-comitant conditions Prevention of Malaria death Pre-hospital treatment - IM Quinine - Artesunate Suppository (MRG received BMJ group award for Best Research Paper of the Year 2010) Chemoprophylaxis / IPT Malaria Vaccine DRUGS FOR CHEMOPROPHYLAXIS Pyrimethamine – Limited efficacy Proguanil – 200mg daily- Limited efficacy Doxycycline – Travelers 200mg daily. Not in children or pregnant women Malarone (Atovaquone/proguanil) – very effective, good safety margin but expensive ($32 – 35 USD/dose) Mefloquine – 250mg weekly (T1/2 too long, neuro-psychiatric AE) Chloroquine/Amodiaquine Not recommended as it is used in Rx Resistance emerged Bone marrow suppression with amodiaquine Conclusion Malaria has no characteristic clinical feature High index of suspicion is the key Early diagnosis & Prompt & appropriate treatment (EDPT) – 1st contact Death is avoidable with early effective treatment & meticulous followup