Nutrition Support in Critical Illness
advertisement

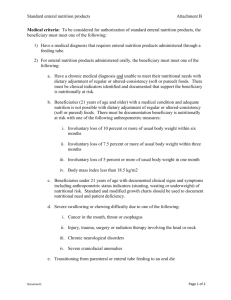
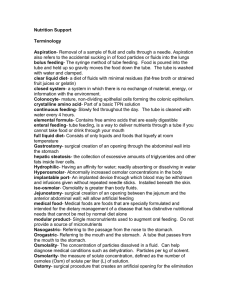
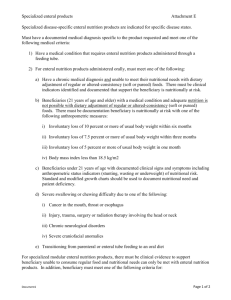
Nutrition Support of the Hospitalized Patient METABOLIC RESPONSE TO INJURY Ebb Phase Flow Phase “Catabolic” INJURY 0 12 HOURS 24 1 2 WEEKS 3 Severe Injury Moderate Injury Mild Injury Severe Injury Moderate Injury Mild Injury HYPERMETABOLISM GLUCOSE METABOLISM • Glucose production ’d (lactate, alanine, glycerol) • Peripheral uptake/use ’d (non-insulin based) • Entrance into Kreb’s cycle ’d • Lactate, pyruvate ’d • Insulin resistance • Exogenous glucose can’t suppress GNG GLUCOSE CORI CYCLE LACTATE GLUCONEOGENIC AMINO ACIDS PYRUVATE Pyruvate dehydrogenase inhibition ACETYL COA TCA CYCLE LIPOGENESIS KETONES HYPERMETABOLISM GLUCOSE METABOLISM • Glucose production ’d (lactate, alanine, glycerol) • Peripheral uptake/use ’d (non-insulin based) • Entrance into Kreb’s cycle ’d • Lactate, pyruvate ’d • Insulin resistance • Exogenous glucose can’t suppress GNG Glucose Appearance Rate (GNG) (mg/kg-min) 14 12 10 8 6 4 2 0 Control Non-oxidized Oxidized Skeletal Trauma Sepsis Burns Glucose Appearance Rate (GNG) (mg/kg-min) 6 5 Basal 4 Glucose Infusion 3 2 1 0 Normal Septic HYPERMETABOLISM FAT METABOLISM • ’d preference as fuel source • 30-40% non-protein calories • Ketone body production ’d • Lipolysis, TG, FA-TG cycle ’d • Hepatic stetatosis HYPERMETABOLISM PROTEIN METABOLISM • Acute phase reactants ’d • ’d efflux from periphery • ’d oxidation amino acids (30%) PROTEIN TURNOVER IN HYPERMETABOLISM 8 6 Gram/kg/day 4 2 0 -2 -4 -6 -8 -10 Vo lun tee rs Tra um aB asa l Tra um aT PN Protein Catbolism Net Protein Loss Protein Synthesis Basal Metabolic Rate (BMR) Basal Energy Expenditure (BEE) Resting Energy Expediture (REE) ENERGY EXPENDITURE Activity Level Thermic Effect of Food Components of Total Energy Expenditure Diet Other Induced 2-7% 7-13% Physical Activity 15-30% Basal Metabolic Rate 60-75% Malnutrition and Critical Illness • CLASSICAL - Months to years • STRESSED - Days to weeks TPN Terminology TPN - Total Parenteral Nutrition PPN - Peripheral Parenteral Nutrition IVN - Intravenous Nutrition IVH - Intravenous Hyperalimentation “Hyperal” What is the effect of EN vs TPN on infectious outcome? Septic Complications in Trauma Patients Enteral vs Parenteral Nutrition Major Infections TEN (n=29) 1 (3%) TPN (n=30) 6 (20%) p<0.03 4 (14%) 5 (17%) NS 5 (17%) 11(37%) NS (abdominal abscess, pneumonia) Minor Infections (wound, catheter, UTI miscellaneous) Total Complications Septic Complications in Trauma Patients Enteral vs Parenteral Nutrition ENTERAL N Calories/kg/d N Balance (mg/kg/d) 51 16 TPN * -171 45 19 -190 Pneumonia Intraadbominal Abscess Line Sepsis 12 2 * * 31 13 2 * 13 Infections/pt 0.4 * 1.2 * p<0.05 More severely injured patients (ATI>40, >20 units blood, reoperation) benefited most What is the effect of EN vs TPN on infectious outcome? EN is preferred when possible How does the timing of administration of EN affect infectious m/m in critically ill patients? How does the timing of administration of EN affect infectious m/m in critically ill patients? Begin early at low rates What’s the down-side to aggressive enteral feeding in the critically ill? Duodenal feeding during PEEP Ventilation 12 10 8 Hepatic Gut Systemic 6 4 2 0 Baseline Injury Oxygen consumption Fed AJS 1993:165:189 What’s the down-side to aggressive enteral feeding in the critically ill? Begin early - at low rates Membrane Energy Consumption • Ion Transport – Na-K ATPase – Ca-ATPase – K-H ATPase – H leakage mitochondria • Organic Compound Transport – AA, Nucl Ac ,Protein, glucose • Macromolecular Transport – Membrane proteins, Phospholipids Protein Related Energy Consumption • Protein Turnover – Formation initiation complex – Peptide bond synthesis – Protein degradation • RNA turnover: rRNA, tRNA • Amino Acid transport • Regulation and integrity – 2nd messengers, ion pumps, protein translocation • Nitrogen Metabolism – Glutamine/glutamate; glu/ala; urea Malnutrition and Critical Illness • Hypermetabolism is not abolished simply by providing nutrition Malnutrition and Critical Illness - Objectives “Cut Your Losses” What to Give? Enteral or Parenteral Nutrition Intravenous Nutrition Components • • • • Water Glucose Nitrogen (A.A.) Lipids • Electrolytes • Trace Minerals • Vitamins • Additives Route of Administration ENTERAL • Less Expensive • Delivery Problems – Diarrhea – Ileus – Access problems • Efficacy Metabolic Rates of Specific Organs Miscellan's 20% Liver 29% Kidney 11% Muscle 11% Heart 8% Brain 21% Energy Expenditure Fick Principle • Caloric Expenditure ~ Oxygen Consumption • O2 consumption measured - PA Catheter • Need to know – Hemoglobin – Arterial Oxygen content – Venous Oxygen content – Cardiac Output Energy Expenditure Fick Principle (VaO2 - VvO2) x C.O. x 0.06 x 4.83 = kcals/hr dl/min kcal/l 60 min/hr x 1L/1000 ml 1.34 x Hb x Sat ml/dl Impact vs Osmolite HN in ICU Patients • • • • 326 enrollled (trauma, surgery, sepsis) Age 60 +/-; sepsis or IRS Fed within 48 hrs Post Hoc stratification – >1150 ml in 96 hrs – > 7 days fed – >5 days fed at 1150 ml – cumulative fed 5750 ml Crit Care Med 1995;23:436-49 Impact vs Osmolite HN in ICU Patients • Both tolerated = well, N2 Balance • Mortality: 15.6% Imp vs 7.6% Osm (ns) • In selected groups: • Hosp stay reduced (only survivors) • Acquired infections/pt reduced Crit Care Med 1995;23:436-49 TEE=1.32 x REEm 4500 TEE REEm 4000 3500 3000 2500 2000 1500 1000 500 0 A C G I MEAN Ann Surg 1996;23:395-405 Growth Hormone • 191 aa polypeptide secreted by anterior pituitary • Anabolic rather than anti-catabolic effects on skeletal muscle • Increases sysnthesis w/o affecting catabolism What is the preferred method of delivering EN ? What is the preferred method of delivering EN ? Stomach or small bowel either acceptable Does the composition of EN effect the infectious morbidity and mortality in critically ill patients Does the composition of EN effect the infectious morbidity and mortality in critically ill patients Elemental vs polymeric -> polymeric Fiber - no benefit Imune enhancing - uncertain Membrane Maintenance ENERGY EXPENDITURE Protein Metabolic Transport Turnover Cycles Components of energy expenditure in patients with severe sepsis and major trauma: A basis for clinical care TEE TEE/Bwt Indirect Harris(kcal/d) (kcal/kg/d) calorimetry Benedict SEPSIS Week 1 Week 2 1927 ± 370 3257 ± 370 25 ± 5 1.0 ± 0.2 1.3 ± 0.2 47 ± 6 1.7 ± 0.2 2.3 ± 0.3 2380 ± 422 4123 ± 518 31 ± 6 1.1 ± 0.2 1.4 ± 0.3 59 ± 7 1.8 ± 0.2 2.5 ± 0.3 TRAUMA Week 1 Week 2 Crit Care Med 1999; 27:1295-1302 Enteral tube feeding in the intensive care unit: Factors impeding adequate delivery TABLE 1 -- Reasons for cessation of enteral tube feeding Reasons for Cessation Proced RV Tube Diag Nurs Other Patients affected (%) 39 45 41 27 30 32 Infusion time lost (%) 6.4 2.8 1.4 0.8 0.3 6.6 Cessation time (%) 35 15 7.7 4.6 1.4 36 Avoidable (%) 80 70 67 52 99 52 RV, residual volume; Tube, tube displacement; Diag, diagnostic tests; Nurs, nursing care. Crit Care Med 1999; 27:1252-1256 TABLE 1 -- Reasons for cessation of enteral tube feeding Reasons for Cessation Proced RV Tube Diag Nurs Other Patients affected (%) 39 45 41 27 30 32 Infusion time lost (%) 6.4 2.8 1.4 0.8 0.3 6.6 Cessation time (%) 35 15 7.7 4.6 1.4 36 Avoidable (%) 80 70 67 52 99 52 RV, residual volume; Tube, tube displacement; Diag, diagnostic tests; Nurs, nursing c Enteral tube feeding in the intensive care unit: Factors impeding adequate delivery Physicians ordered a- 65.6% of goal requirement Only 78.1% of the volume was actually infused 339 days of infusion pts received 51.6% of goal (range, 15.1% to 87.1%) Only 14% of patients reached 90% of goal feeding (for a single day) Crit Care Med 1999; 27:1252-1256 Components of energy expenditure in patients with severe sepsis and major trauma: A basis for clinical care Crit Care Med 1999; 27:1295-1302 Critically Ill ? In the ICU Apples and Oranges Trauma CCU Pancreatitis CHF COPD Post-op Abdominal Abscess CVA MI SICU Pneumonia ARDS Hepatic Failure Urosepsis MICU Nutrition Support in Critical Illness