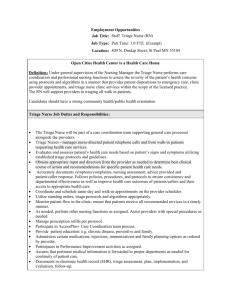
presentation ( format)

Chris Rooney BSN, RN BC
Health Services
Millersville University of Pennsylvania
Located in Millersville, Pa.,
8400 students
3 miles from Lancaster City
1 1⁄2 hours from Philadelphia
2 1⁄2 hours from Washington D.C.
3 hours from New York City
Staffing
◦ Full Time Medical Director - D.O.
◦ NP 1.75 FTE (12 mo and 9 mo)
◦ RNs 4.75 FTE
◦ Clerical Support 1.80 FTE (12 mo and 10 mo)
Visits per year 11,000
Hours 8a-5 p M-F
7 Exam Rooms Built 1968
Health Fee Funding
Define Nursing Triage in the college health setting
Discuss treatment protocols after triage
Identify tools to expedite statistical analysis of triage and treatments small school style
Main Entry: tri·age
Pronunciation: \trē-ˈäzh, ˈtrē-ˌ\
Function:
—triage noun
1 : the sorting of and allocation of treatment to patients and especially battle and disaster victims according to a system of priorities designed to maximize the number of survivors
2 : the sorting of patients (as in an emergency room ) according to the urgency of their need for care transitive verb
Merriam Webster Dictionary
Scope of practice -
•
Direct Nursing Care
•
Collaborative Role
•
Health Educator
•
Research/Consultant
•
Advocacy
Combining Triage with College
Health Nursing
History taking with physical/mental/spiritual assessment with cultural competency
Acute illness and injury care – chronic illness
Health Education and Promotion – disease prevention
Management and leadership of risk reduction, resources, facilities, environment, including safety, infection control, etc
Prioritization of services for individuals based on assessment and triage
Staffing
Staff – provider type
Time – hours of service , time of day
Method of contact
Walk in
Phone interaction
Chief Complaint - Assessment
Appointment/walk-in
Need for ancillary services - immediate lab/x-ray
Other considerations
Transportation
Distance to acute care/ER
State Board of Nursing Law
Standard of Care
◦ National Council of State Boards of Nursing. https://www.ncsbn.org/312.htm
◦ Article 2, chapter 2
Medical Direction – what is your medical director comfortable with?
◦ Protocols/documentation
◦ Expertise of staff
Case 1
◦ Joe, 18 y/o male walks into your Health Center requesting an Albuterol Inhaler in no acute distress. 4:00 p.m. on Friday Afternoon before
Spring Break. Providers – Physician, PA/NP – out of the building. Front Office staff and 2 RN’s
Literature
Review of
Protocols
None specific to college health
2007 JCN -Clinical decision making
2008 IJN - Knowing the patient
2009JCN – Context vs protocols
2008 JTIICC – Triage Tools
2009 IJCN - Expertise
URI Assessment sheet
URI/Respiratory
NAME:_____________________________________________________ Date of Birth____________
Address___________________________________Best Phone # to call________________________________
DATE:_______________TIME_________ Page #___________
Medications
Allergies
PMH
SUBJECTIVE
OBJECTIVE: T P R BP O2 Sat Flu Screen □ Pos □ Neg
□ Not assessed by RN__________________________________
Skin: □ Not Assessed □ Normal: Warm, dry, color normal, no rash □ Hot □ Cold □ Diaphoretic □ Cyanotic □ Pale
□ Jaundice □ Edema/Swelling______________□ Ecchymosis_____________ □Rash __________________________________
Eyes □ Not Assessed □ Normal PERRLA, Conjunctiva normal, normal acuity , no drainage, swelling, or pain
□Abnormal □ R Pupil __mm □ L Pupil __mm □Swelling/edema/__________________
□ Conjunctiva: Pale □ Injected □ Ichteric □ Exudate: ______________ Other
Ears □ Not Assessed □ Normal: Canals patent, +light reflex, TM normal, acuity normal
□ Abnormal TM R L □ Bulging □ Erythema □ Retracted □ Tender to touch R L Both
□ External Ear_______________________ □ Other _______________ □Hearing Deficit
□ Abnormal Canal R L □ Erythema □Cerumen □ Edema □ Other ____________________________________________
Nose □ Not Assessed □ Normal: Sinus nontender, turbinate normal, septum midline, no drainage/congestion
□ Sinus Congestion □ Sinus Tenderness: Maxillary/Frontal □ Rhinnorhea: Clear Yellow Green Other_______________
□ Turbinate Mucosal Color___________ □Other
Throat □ Not Assessed □ Normal: Normal Pharynx, tonsils, mucous membranes
□Tonsils □Normal □Absent Size_____ □Inflammed □Exudate_____________□ Cryptic
Post Phyx □ Normal □ Erythema □ Cobblestone □ PND_____________ □ Ulcers _______________________________
Mucous Membranes □ Normal □ _________________ Dentition □ Normal □ ________________________□Other
Neck/Nodes □ Not Assessed □ Normal No Adenopathy, non tender, neck supple, normal ROM
□ R Ant_________Post_________ □ L Ant_________ Post__________ □ Tenderness
□ Rigidity □ Stiffness □ Vertebral tenderness _________ □ ROM limited / painful _______________□Other
Respiratory □ Not Assessed □ Normal No pain, normal excursion/expansion, no retractions, no SOB, CTA
□ Retractions □ Unequal/↓ BS_______________□Nasal Flaring □ Pain or tightness □ Chest Tender to palpation______________
□ Rales ______ □ Rhonchi ______□Wheezing______ □ Labored □ Stridor □ Cough □Productive _________________□ SOB
□ Peak Flow ______/PN_____ ______% □Other
□ Rapid Strep □ Discussed □ Rapid Mono □Discussed □ Throat Culture Sent □ Discussed T/C □ Rapid Flu
URI/Respiratory
NAME:_____________________________________________________ Date of Birth___________
DATE:_______________Cont’d
Page #___________
Assessment:
Plan:
□
Evaluation by MD/DO/NP Signature:
Plan:
□
Acetaminophen 325 mg 2 or 3 tabs PO Q 4 – 6 hrs.
□
Acetaminophen 500 mg (ES Tylenol) 2 tabs PO Q 4-6hrs
□
Ibuprofen 200mg ____ PO Q 6 hrs with food Pkgs____
□
Hycodan ________________________________
(DROWSINESS)
□
Amoxicillin 500 mg 1 cap PO three times a day #30
(OCP Prec.)
□
Naproxen Sodium 220mg ____ PO q 12 hours Pkgs____
□
Saline Nasal Spray
□
Saline Gargle
□
Throat Spray □ Lozenges
□
Afrin Nasal Spray 2-3 sprays each nostril every
□
Azithromycin (Z-Pack) 250mg as directed
with food. (OCP Prec.)
□
□
Bactrim DS 1 PO BID #20 (OCP Prec.)
Cephalexin (Keflex) 500 mg #40 1cap PO QID
12 hours x 3 Days
(OCP Prec) 2 cap PO BID
□
Doxycycline 100 mg. 1 PO BID #20 (OCP Prec.)
□
Cold Relief Tabs (Acetomenophen 325 mg; Guaifenesin
□
Penicillin VK 500 mg #40 1 tab PO QID
100mg, Phenylphrine 5 mg, Dextromethoraphan 15 mg, )
2 tabs PO Q 4-6 hours #____
□
Pkgs____
Pseudoephedrine 30 mg 60 mg PO Q 6 hrs #______
(OCP Prec.) 2 tab PO BID
□
Albuterol Inhaler 2 puffs every 4-6 hours or as directed
□
Prednisone 5mg #36 Per schedule □
Loratadine 1 PO Q 24 hrs (drowsiness) #______
□
10 mg #12 #18 Per schedule
Chlorpheniramine Maleate 4 mg PO Q 6 hours #______
(DROWSINESS)
□
Guaifenesin DM Plain 10cc PO Q 4 hrs prn cough
□
Mucinex 600 mg 1 Q 12 hours #10 Increase PO Fluids
□
Drink plenty of fluids □ Written instructions
□
Thermometer
□
_______________________________________________
□
_______________________________________________
□
Agrees / Expresses understanding of POC
□ F/U if persists or worsens ____________________
□
Appt with MD/DO/NP_________________
□
Class Excuse □ Social Distancing
□
Home
Signature_____________________________________
□
Agrees/Expresses understanding of POC
□
F/U if persists or worsens ____________________
□
Appt with MD/DO/NP_________________
□
Social Distancing
□
Home
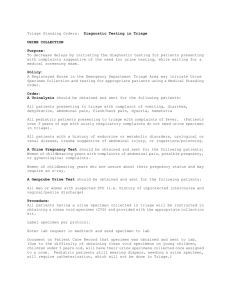
Pandemic Influenza Triage Screening Tool
1.Has there been exposure/contact with anyone else with symptoms?
2.Is there a documented fever of 101 or higher?
3.Does the patient have any of the following: runny nose/nasal congestion, cough, sore throat?
4.Did the illness begin abruptly – how long present
5.Ongoing chronic illness? Diabetes, immunosuppression, asthma organ recipient, gastric bypass?
6.Difficulty breathing, severe N/V dark urine, fever more than 72 hours
7.Pregnant?
8.Does the student believe they need to be seen in person
Yes to 1 and/or 2 – Follow Respiratory Nursing Procedure/Standing
Orders
Yes to 1,2,3, and 4 – less than 48 hours – same day nurse appt – Flu test and referral as appropriate
Yes to 1, 6, 7, or 9 – Same day appt with provider
Yes to 7 – consider immediate or ER Eval – clinical decision/symptoms
Telephone call at 11:00 a.m. from 21 year old female student, LeaAnn, reporting abdominal pain for 3 days.
Slight nausea, right sided lower back pain, denies fever,
(doesn’t have a thermometer.) Hasn’t been to class the last three days.
States pain is so bad - can’t get out of bed.
Can you ambulate? Can you get to
Health Services?
The nurse asks more questions:
Vomiting No
Diarrhea No
Dysuria Yes x 3 days
LMP 2 weeks ago - normal
What other questions are you going to ask before you determine course of action?
Resource: Telephone Triage Protocols for Nurses Julie K Briggs
Lippincott 2006
Appointment scheduled for assessment --- with provider if available/with nurse for triage.
Abdominal Pain
Nursing Management and Standing Orders
Definition: Recent onset of abdominal pain
Pathogenesis:
Major mechanisms of acute abdominal pain include obstruction, distention, peritoneal irritation, mucosal ulceration, vascular compromise, traumatic injury, and referral from an extra-abdominal site
Types of abdominal pain o Visceral pain is deep, dull, crampy, poorly localized o Somatoparietal pain is sharp, well localized, and originates from noxious stimulation of the parietal peritoneum and generally is more intense and more precisely located than visceral pain o Referred pain in pain that is experienced at a distance from the disease
Clinical Presentation
Location of the pain may provide clues to common causes of abdominal pain from both intra-abdominal and extra-abdominal sources (See attached chart)
Nursing Guidelines
The nurse will evaluate the following data
Subjective
- History o Age, gender o Past medical/surgical history o Current medications o Medical allergies o History of alcohol or Tobacco use
- History of Present Illness o Determine onset, location, and quality of pain o Have patient rate pain on scale of 1-10, does it interfere with sleep o Has pain changed since onset o Does pain radiate or refer to other sites o
Is the pain relieved or aggravated by anything o Any vomiting, changes in bowel habits, urinary symptoms o In females – any pelvic symptoms - dyspareunia, abnormal vaginal discharge, irregular menstrual bleeding, any possibility of pregnancy
Objective
Vital signs
General appearance – pallor, perspiration, restlessness, distress
Auscultate bowel sounds
Palpate abdomen, assess for rebound tenderness or guarding
Assess CVA tenderness
Standing Orders
Constipation
Abdominal Pain
Standing Orders
Obtain clean catch urine sample o Dip urine via Clinitec Machine, per laboratory procedure. o If pregnancy suspected/concern – do pregnancy test, per laboratory procedure.
If MD/NP present – refer for evaluation
If MD/NP not present and: o If Temp > 100.5, HR > 120, or RR >24, pain is moderate to severe, localized, associated with nausea, vomiting, back pain, moderate dehydration, vaginal bleeding, hematuria, or if in your clinical judgment referral is needed or patient or parents request a referral
Refer to Emergency Department o If Pregnancy test Positive
Refer to Emergency Department o If Right lower quadrant pain, absent or diminished bowel sounds, abdominal guarding, or positive rebound tenderness
Refer to Emergency Department
If MD/NP not present and patient is: o Afebrile, vital signs normal, normal appetite with unremarkable abdominal exam
Phone consult with physician
Use Cipro if Bactrim DS was previously used and visa versa (prior three months)
Only send cultures in the following circumstances o Suspected Pyelonephritis o Recurrent infections (within 4 weeks) o No improvement in 72 hours after starting antibiotic treatment o Infection symptoms in patients with diabetes, renal stones, pregnancy, tuberculosis, sickle cell, fever > 101, catheters, GU structural abnormalities, female patient is < 16 years old, all male patients o
No Provider available
Follow up urinalysis is unnecessary if symptoms resolve
Expert opinion favors a three day course of Bactrim DS as initial therapy
(Clinics in Family Practice – article March 2004 referenced in the Infectious
Disease Society of America)
According to this data review, nursing care and physician standing orders were developed.
Nursing Guidelines:
The nurse will evaluate the following data:
Subjective
History: o Age, gender o
Past medical/surgical history o Current medications o Medical allergies o Normal voiding patterns, fluid intake o Past history of UTI’s – number in past year, type of treatment o GU abnormalities o LMP o Sexual activity o Contraceptive use o Vaginal/urethral discharge
History of Present illness o Dysuria, frequency, urgency o Hematuria o Abdominal tenderness o CVA tenderness o Nausea/vomiting o Urinary incontinence
Objective
Vital signs
Palpate abdomen
Assess for CVA tenderness
Standing Orders
Perform urine pregnancy test if indicated
Collect clean catch urine
Dip urine via Clinitec Machine, for nitrates, leuk esterase, blood and specific gravity, and record in chart o
If MD/NP present:
Spin urine for microscopic examination. Hold portion for possible culture and sensitivity o If MD/NP not present and patient has fever, moderate to severe symptoms, back pain/CVA tenderness, urine grossly bloody, multiple antibiotic allergies or pregnancy test positive, refer to Urgent Care or ED. o If MD/NP not present, urine dip is + for leuk esterase*, or nitrate* and the patient is non-toxic:
Dispense Bactrim DS (#3) 1 PO BID x 3 days or Cipro 500mg (#3) 1
PO BID x 3 days , if sulfa allergy
Send urine for culture and sensitivity
Obtain telephonic approval from MD/NP
Arrange F/U appointment with MD/NP within 72 hours
Ensure chart review by MD
* Unreliable on dipstick if pyridium has been used
UTI Flow sheet
GI/Abdominal Pain
Flow sheet
Gastrointestinal/Abdominal Pain
NAME:____________________________________ Date of Birth____________
Address_________________________________Best Phone # to call_________________________________
DATE:__________TIME_________ Page #___________
Medications
Allergies
LMP:
Menses Normal Y N
PMH
Last BM Tobacco Use Y N
ETOH Use Y N
OBJECTIVE : T P R BP O2 Sat
General Appearance □ NAD □ Normal: Warm, dry, color normal, no rash, turgor elastic, moist mucus memb.
Ent/Respiratory: □ Not Assessed □ Normal eyes, nose, throat, lungs CTA, no SOB
Abdomen: □ Normal: Soft, nontender, non distended, BS normal, no organomegaly
□ Pain Location_______________ Quality_________________ Severity (1-10)_______
□ Rebound_____ □Guarding____
□ Bowel Sounds: Absent Normal Hypoactive Hyperactive
□Other____________________________________________________________
GYN/GU: □ Normal: No suprapubic or CVA tenderness
□ CVA Tenderness □ R □ L □Suprapubic pain on palpation
□ Abnormal Vag/Penile Discharge _______________________
□ Rash/Sores/lesions_________________________________________________
Pysch: □ Normal: Affect and behavior appropriate
Assessment :
Plan : □ Evaluation by MD/DO/NP □ Admitted for observation
□ Dicyclomine (Bentyl) 10 mg 20 mg 1 tab PO AC and hs (drowsiness)
□ Diotame 2 tabs PO Q 30-60 mins, no more than 16/24hrs
□ Prevacid 30mg PO daily #_______
□ Pepcid 1 cap PO AC #________
□ Zofran 4 mg 1 po/sl now Time______ (drowsiness) □ Zofran 4 mg 1 po/sl Q 6 hours prn _____#
□ Mylanta 10-20cc PO PC HS
□ Acetaminophen 325mg 500 mg #_____ PO Q 4 6 hrs prn pain/fever
□ Loperamine (Imodium AD) 2 cap PO after each loose BM no more than 8/24hrs
□ Diet Instructions ________________________________________________________________________
□ _______________________________________________________________________________________
□ Written instructions □ Expresses understanding of POC □Appt schedules with MD/DO/NP______________
□ F/U if persists or worsens
Signature :
Vital Signs imperative
Policy/Guidelines – follow documentation form
Guideline resources abundant but not specific to college health
Nursing judgment/clinical decision making within the scope of practice of
Registered Nurse if based on assessment findings and nursing guidelines
Nursing Diagnosis?
Staffing?
Time?
Education
Mental Health
Chronic Conditions
Public Health
Threat
Overview :
The Illness/Injury Severity Index is a triage tool which can be used to recommend patient disposition after assessing the severity of traumatic injury.
Parameters:
Copyright (c) 2006-2007, Institute for
Algorithmic Medicine, Houston, TX, USA.
All rights reserved.
(1) pulse
(2) blood pressure
(3) skin color
(4) respiratory condition
(5) consciousness
(6) bleeding
(7) region of injury
(8) type of injury
(9) age of patient
(10) previous history of condition
Parameter pulse blood pressure in mm Hg skin color respiratory condition age consciousness bleeding region of injury type of injury previous history of condition being treated
Finding
60 - 100
< 60, or 100 - 140
> 140 or irregular absent systolic 100 - 150; diastolic 60 - 90 systolic 80 - 100 or 150 - 200; diastolic 90 - 120 systolic < 80 or > 200; diastolic > 120 absent dry and normal reddish coloration ashen and/or moist cyanotic
12 - 20 breaths per minute
>= 20 breaths per minute
< 12 breaths per minute, or labored breathing or chest pain absent respirations alert and oriented incoherent or obtunded difficult to awaken unconscious none controllable hard to control uncontrollable none observed extremities back chest head, neck, abdomen none observed laceration or contusion fracture stab wound blunt trauma or missile
< 2 years of age
2 - 60 years of age
> 60 years of age no yes
3
4
0
1
2
3
0
1
2
3
0
1
2
3
0
1
2
3
4
1
0
1
0
1
3
0
1
2
3
0
1
2
Points
0
1
2
3
0
1
2
Copyright (c) 2006-2007, Institute for Algorithmic Medicine, Houston, TX, USA. All rights reserved. where:
• The scoring of systolic and diastolic blood pressure is unclear; it is presented as a ratio, could be ANDed, but implemented as OR
• The above table differs from the table in Bever and Veenker with the addition of "none" for both region of injury and type of injury. This is explained in the text on page 45.
• Age and previous history are listed as footnotes in the original table. illness/injury severity index =
= (points for pulse) + (points for blood pressure) + (points for skin color) + (points for respiratory condition) + (points for consciousness) + (points for bleeding) + (points for region of injury) + (points for type of injury) + (points for age)
+ (points for previous history)
Interpretation:
• minimum index: 0
• maximum index: 28
Index
<= 3
4 - 6
7 - 11
>= 12
Index
<= 5
6 - 13
14 - 24
25 - 28
Outcome in Illness Group patients can be released from the Emergency Department patient admitted to hospital but non-critical care unit patient admitted to critical care unit or had surgery predicts patient death in the emergency department
Outcome in Injury Group patients can be released from the Emergency Department patient admitted to hospital but non-critical care unit patient admitted to critical care unit or had surgery predicts patient death in the emergency department
NOTE: The table in Ford differs from the original data in Bever and Veenker for (a) points for region of injury, (b) points for type of injury, and (c) interpretive breakpoints.
<>
References:
Bever DL, Veenker CH. An illness-injury severity index for nonphysician emergency medical personnel. EMT Journal.
1979 (March); 45-49.
Ford EG. Chapter 4: Trauma Triage. pages 95-117 (page 101). IN: Ford EG, Andrassy RJ. Pediatric Trauma - Initial
Assessment and Management. W.B. Saunders Company. 1994.
Create an assessment check list that when completed gives a numeric score that determines disposition.
Utilize the guide to determine disposition or treatment per standing order.
Does nursing already do that – mentally/experientially?
Do we have tools that are part of that system
Centor Score –
Pharyngitis
Exudate
Tender Nodes
Fever >101
Absence of Cough
None or 1 – symptomatic TX
2,3,4 – do Rapid Step
+ treat/- Consult
Provider
Ottawa Ankle Rules
Pain in malleolar zone and one of:
Pain posterior 1/3 distal tibia/med malleolus
Pain distal
Fibula/lateral malleolus
Inability to take 4 steps
Institute for Clinical Systems Improvement www.icsi.org
Flow charts and algorithms for triage
Rapid Assessment A Flowchart Guide to Evaluating Signs and
Symptoms Lippincott 2004 $45
Adult Telephone Protocols: Office Version (Spiral-bound)
~ David A Thompson $85 (Amer. Acad. Of Peds)
Telephone Triage Protocols for Nurses Julie K Briggs Lippincott
3 rd Edition $50
Emergency Severity Index, Version 4: Implementation Handbook
Chapter 2. Triage Acuity Systems http://www/ahrg.gov/research/esi/esi2.htm
(Adaptable ED acuity systems with Practice Cases)
Assessment needs to include cultural/ethnic variations
Example: Muslims may believe that sickness is a test from God, seen as a purification from sins and require a cure from God
Students’ limitations in ambulation and communication and differentiation between acute and chronic neurological conditions are the main challenges in the triage of students with special needs and disabilities.
Language Barriers – Use of interpreters – Time – use internet translators Google’s Language tools AltaVista
Translator TTY/Deaf
Document calls and the triage decision in the medical chart, indicating the protocol used and the advice provided. Use the caller’s own words to describe the reason for the call.
Develop triage algorithms to assist the RN, NP/PA/Physician in appropriate documentation of telephone conversations.
Develop a written policy defining the role and limitations of non-clinical or unlicensed staff, as well as specific symptoms requiring immediate attention.
Review all telephone triage decisions for appropriateness of actions taken.
Review all scheduling encounters for appropriateness and timeliness of appointments.
Allow only qualified staff to provide telephone advice.
Examples of nurse initiated interventions to expedite care at triage may include:
Administration of analgesia; antipyretics; oral rehydration; oxygen therapy
Diagnostic testing: Rapid Strep or Flu, Blood glucose measurement; Urinalysis
First aid (BLS, splinting, RICE, eye irrigation) wound management
Self Care – OTC’s, Discharge instructions, education
F/u care recommendations – when, why, with whom
All nurse-initiated interventions should be in accordance with organizational guidelines and policies.
General lack of evidence based research in terms of Nursing Triage and Treatment outside of emergency rooms.
Non existent in College Health
No financial reimbursement for nurse visit
Variety of scope of service across campuses
Centrality to mission and goals of Health Services
What information
How to gather
What to do with it
Paper and pencil spreadsheet by the night nurse who “counted” the days activities.
Monthly total/Yearly total
Penetration rate?
Utilization by individual students?
Justification for resources?
Encounter form
Demographic data
Diagnosis
Interventions and Disposition
SCANABLE PAPER FORMS
Pros:
Equipment on campus for test scoring
Accurate data
Included Penetration
Good snap shot of Health Services
Easy for staff to complete at end of visit
Cons:
Data – Scanned monthly – reports at end of term
IT – physically cumbersome – carried across campus to scan
Cost of Printed sheet/paper/HIPAA
Change form – new form design/retool scanner/
Students hated completing the demographic portion of bubble sheet -
Excel Spread Sheet – Concurrent use in Fall
09 with bubble sheets.
Outlook Scheduling – Started in Fall 2009 – prior had paper and pencil schedule
◦ No reporting capability
◦ Appt and treatment – not connected
Interested in looking under the hood?
Customized Scheduler with database - Asset management system
IT department configured Database with Open
Source EMR
Web based – accessible from any PC on HS
Intranet
Link the appt with treatment
Cost – IT support to configure/debug
Discussion
◦ How do you quantify your nurse triaged patients?
◦ Do you evaluate effectiveness of your protocol?
◦ Satisfaction of students?
◦ Learning Outcomes?
Other comments?
Nurses – Assessment and triage of students in college health settings is within the scope of registered nursing practice.
Develop simple easy to use algorithms and base documentation on their use.
Alter in the event of significant medical occurrence – Pandemic – create tools
Maintain cultural competency
Quantify and evaluate effectiveness
Need to research and publish evidence based data in College Health Nursing Triage
Encourage collaboration with Nursing Staff in creating Triage Protocols
Chris Rooney, BSN RN BC
Millersville University Health Services chris.rooney@millersville.edu
Thank you!