Making it happen - NHS Education for Scotland
advertisement

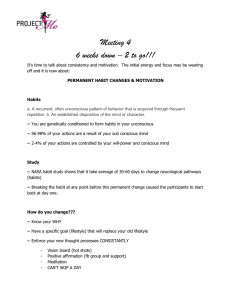
Making it happen Evonne Curran Nurse Consultant Unknown but limited ingredients Variable talent Time limit Goal: Make the best possible output with the above At the end of the day..... It would be good to say.. • I can show that because of me (xxxxxxxxxxxx ) – Is now performed more safely – Has improved the patient experience – Has reduced risks to the organisation – Has resulted in fewer infections – Has resulted in less waste (money, time, resources) LAND MINES Lack of vision Lack of information Lack of inclusion Lack of strategic thinking Lack of strategic alignment Participation as an end Lack of productive conflict Untested assumptions Lack of alignment Lack of communication and accommodation Focus on results – not the steps to the results http://www.rexroundtables.com/showbriefs-yplansfail.php Risk assessment Very high High Moderate Low Devasting Severe Moderate Minor Potential benefits assessment Very likely Reduce harm / risks Improve pt experience Reduce costs Faesible Likely Low likelihood Undetectable Potential topics - what is important to • • • • • • • You Your IPCT Those at the front line The antimicrobial pharmacist Those who hold the purse strings The patients The HAI executive lead What makes hospital infections • Invasive Devices – Urinary Catheter – PVCs • Norovirus • Antibiotics • Contaminated equipment • Failure to comply with SICPs Topic Review • • • • • The problem? How big is it? What is driving the problem? What is achievable? Benefit Assessment? Urinary catheters • • • • • • We use too many of them! We keep them in too long We don’t know about alternatives By pass defence mechanism Perfect culture medium Alternatives – not accessible – Scales to weigh urine – Female slipper pans – Suitable inco pads Habits • Habits emerge because the brain is constantly looking for ways to save effort (system 1 / 2 thinking) • When a habit emerges the brain stops fully participating in decision making. – The order you wash in the morning • Unless you deliberately fight a habit – find new routines – the habit will unfold automatically • Habits work on cues • Habits are driven by ‘cravings’ • Willpower becomes a habit when certain behaviours are chosen ahead of time – routine followed when cue arrives The Power of Habit – why we do what we do and how to change, Duhigg Q How man animals of each kind did Moses take on to the ark? Habits in healthcare just as in life • Serve us well • Allow us to do things swiftly and consistently • But… from time to time we need to break old habits and create new ones Habit Loop Action Buy and drink coffee, eat muffin or sub Cue Reward Job done Smell of coffee, Smell of cinnamon Smell of Subway Feel satisfied (and guilty) Craving: taste, effect of drinking coffee (not hunger)? Habit Loop Action Indwelling foley catheter Cue Reward Job done Urinary retention Fluid balance measurement required No longer in retention Urine measured Craving: to do something good / technical / solve a problem Habit Loop • For success – Need a new habit • Need to know and have access to alternatives – Accurate fluid balance does not always need a catheter – scales and a bottle – Uro-sheaths reduce infection risk – Intermittent catheters – Need to believe that it can be achieved • Some one else has done it – group therapy • Data to show it works • Data to show it matters How do we change habits • Need to learn new habits that overpower the current habit behaviours • Find new routines and rewards from cues • Works for (some but not all) alcoholics • The ingredient that made a reworked habit into a permanent behaviour – Belief • What is our (habit) reaction to: “we are going to introduce a new initiative to……. “ New Habit Loop Action Engage with patient to consider best possible option for patient Cue Reward Job done Urinary retention Fluid balance measurement required Patient centred care & catheter avoidance Our craving needs to be to achieve PCC Social Marketing • A process that applies marketing principles and techniques to create, communicate, and deliver value in order to influence target audiences behaviours that benefit society (public health, safety, the environment and communities) Kolter et al (2006) If not social marketing what else? • Education & Data feedback – Use of rational facts to persuade people to adopt a different behaviour • Coercion – Forces people to adopt a behaviour under threat of penalty for not doing so Social marketing Is • • • • • A social behaviour change strategy Most effective when it activates people Targeted towards those who have a reason to care Strategic and requires efficient use of resources Integrated and works on a plan Social marketing in healthcare, Radha Aras 4ps of Social Marketing • Product: Desired behaviours – Reduction in urinary catheter usage with an increase in safer alternatives – Increase in patient involvement in decision making – Optimisation of clinical decision making • Price: Cost associated with the behaviour changes – Price of CA-UTI (physical and psychological) – Effort – resource required • Place: Make it convenient – to translate the motivation into action. Intervene at the point of decision making • Promotion: Make the new habit acceptable, easy, and desirable to the audiences Social marketing in healthcare, Radha Aras Lets now look at a plan to join our habit knowledge with our social marketing knowledge To modify a habit you need to answer these questions • Location: where are people when the cue happens / decisions are made / first acts? • Time: does it happen at a particular time? • Emotional state: what state are people in when the cue arises? • Other people: who else is around to help with decision making? • Immediate preceding action: what happens just before the decision? Before you start • Identify and prioritise barriers – Don’t have easy access to alternatives – Don’t know what to use when – Don’t consider remove ASACI • What will over come barriers – Get help from continence support – From whoever has the budget – Alternatives and placement of alternatives – Training • Pilot • (We still need education and data) Clear message catheters are dangerous STOP Before you catheterise…. Reason to believe: Limiting urinary catheters is doable and better for patients • 7mth pre period; 4 mth intervention period • Limit criteria set: urinary tract obstruction, hourly output measurement, etc. • Measured – CAUTI – Urinary catheter – Nursing experience • UC usage decreased by 42%,CAUTI by 57% nursing satisfaction improved Rothfeld et al AJIC 2010 38 568-71 What we do in nursing • Are learned behaviours • Habits run by – cue, action, reward • To bring about safer action – Need different habits (that involve patients more) – Need education on safest alternatives for patients to optimise clinical decision making – Need easy access to the safest alternatives – Need data that shows we provide optimal care Habit and social marketing • Social marketing can help deliver the message – Alternatives to catheterisation are suitable and safer in many cases – Here are the alternatives to catheterisation • This messaging will make the case for new habits (create the belief) and make it easier for new habits to become established Need to find out – what are the attitudes to the process to be changed • Is it a settled way of thinking or feeling, typically reflected in our behaviour? • Or are we ready to break a habit? Potential benefits assessment Very likely Reduce harm / risks Improve pt experience Reduce costs Faesible Likely Low likelihood Undetectable Lets do one together • • • • • The problem? How big is it? What is driving the problem? What is achievable? Benefit Assessment?