L 2 Tubular transport_1
advertisement

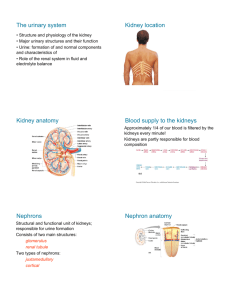
Urinary System L 2, 3 Tubular Reabsorption & secretion Prof. Madaya Dr Than Kyaw 1, 8 October 2012 Tubular Reabsorption & secretion Reabsorption • For reabsorption a substance - must pass from tubular lumen through tubular epithelial cells - diffuse through interstitial fluid (ISF) - enter the capillary Secretion • For secretion a substance - must leave the capillary - diffuse through ISF - pass thru tubular epithelial cells into the lumen Reabsorption and secretion Reabsorption of Na+, Cl-, glucose and A/A • Substances important for body functions (e.g. glucose, a/a) enter tubular fluid by filtration at the glomerulus • Due to their relatively small molecular size - pass easily thru’ glomerular membrane • Concentration in the filtrate and plasma the same • If they are not returned (not reabsorbed) to blood – they are excreted in the urine and lost from the body Proximal convoluted tubules Proximal convoluted tubules - the longest part; make up most of the renal cortex - cuboidal cells with a luminal border modified with microvilli (brush border) providing large surface area - important substances like glucose and amino acids - 100% reabsorption Glucose or A/A in Tubular lumen Diffuse into peritubular capillary Transport coupled with transport of Na Carrier protein No additional energy needed for glucose or A/A Na+ + glucose or Na+ +A/A Active transport (energy used Na+ -K + -APTase) Reabsorption and secretion • Once inside the tubular cell – A/A or glucose uncoupled from the carrier • Diffuse basal or lateral border to ISF → capillaries • Na+ – actively transported from tubular epithelial cells to ISF and then to capillaries • The carrier protein return to its previous conformation to transport more glucose /amino acids/ Na+ • Unlike other tissues, glucose in the renal tubules and instestine is actively and continually transported even though its concentration in the lumen is minute; thereby loss of glucose from the body is prevented by active transport (uphill) • Active transport needs both carrier and energy Reabsorption and secretion Transport of Na+ from tubular lumen into the tubular epithelial cell and its co-transport with glucose. Energy requirement is provided by the Na+ -K + -APTase (sodium pump) Protein channel (carrier protein): Protein channel: - pores; contain a single or a cluster of proteins; - specificity for certain substances or restrictive due to the size. - Water easily diffuses through protein channel. - Transported molecule enters the carrier protein channel and bind with the receptor. After binding the carrier protein undertakes conformational change to open the channel on the opposite side. - Then transported molecule is released and carrier protein returns to original conformation for transport of another molecules. Reabsorption and secretion Some low molecular weight substances - bound to plasma proteins - retained in the blood plasma E.g. - calcium, iron, hormones (e.g. thyroxine) - only a small fraction of them that are unbound pass through Reabsorption of Water and Urea Removal from lumen into ISF and capillaries • • • • • Na+, Cl- , 65% water, 85 – 90% HCO3 100% glucose, amino acids Other substances Concentration of water in the lumen Absorption favoured by Low HP Water reabsorbed by osmosis into the ISF and capillaries Colloidal osmotic Pressure Tubular secretion Some substances are removed (secreted) - from blood through the peritubular capillary network - into the distal convoluted tubules or collecting ducts. - These include: H+ ions, K+, NH3 , creatinine, and drugs. - H+ ions – secreted throughout the length of nephron tubule (except thin loop of Henle); - coupled with reabsorption of - K+ - secreted at DCT and CT and CD; - coupled with reabsorption of Na+ - NH3 - its secretion rate depends on acid-base equilibrium of body fluid - Urine is a collection of substances that have not been reabsorbed during glomerular filtration or tubular secretion. Tubular Transport Maximum (TM) TM = Substances associated with membrane transporters (carrier or active transport) for reabsorption have a maximum rate at which they can be removed – e.g. glucose Renal threshold = the plasma concentration of a substance when it first appears in the urine - TM for the substance is exceeded its limit. Renal threshold of gucose and diabetes mellitus Deficient or lack of insulin 1 Impaired movement of glucose from plasma into body cells Above renal threshold 2 ↑plasma concentration of glucose Glucose in the tubules & urine (Glucosurea) ↑ Plasma and tubular load exceeds availability of carrier 3 molecules for glucose transport and reabsorption Renal threshold of gucose and diabetes mellitus Glucose contributes effective osmotic pressure of the tubules Osmotic diuresis Water in the tubules & hence in the urine ↑ Volume of water in the tubules & hence in the urine Frequent urination Drink more water Glycosuria (glucosuria): presence of glucose in urine Polyuria: frequent urination Polydipsia : increased thirst Polyphagia : increased hunger Renal counter-current mechanisms 1. Countercurrent multiplier system 2. Countercurrent exchanger system Countercurrent multiplier system: It is the process by which a progressively increasing osmotic gradient is formed as a result of countercurrent flow. Parts involved in countercurrent multiplier system 1. Descending limb of loop of Henle 2. Thin segment of ascending limb 3. Thick segment of ascending limb 4. Cortical collecting duct 5. Outer medullary collecting duct 6. Inner medullary collecting duct Countercurrent multiplier system 1 • Impermeable to solutes but permeable to water • Water diffuses by osmosis to the higher osmotic pressure of ISF • Solute conc. (mainly NaCl) increasing while approaching hair-pin turn of loop of Henle 2 • Thin segment of ascending limb – permeabe for NaCl but impermeable to water • Water remains in the tubule and NaCl difuses (due to concentration gradient) to ISF Countercurrent multiplier system 3 • Thick segment of ascending limb – active transport of NaCl to the ISF • Water continues to be retained • Osmolality of tubular fluid entering descending limb is 300 mOsm/kg H2O • Tubular fluid leaving ascending limb and entering distal tubule – diluted (osmolality 185 mOsm/kg H2O Countercurrent multiplier system Vertical osmotic gradient in ISF Is lower in outer medulla and higher in inner medulla and at hair-pin turn; established and maintained by a) continued active transport of NaCl by thick segment of ascending imb b) conc of tubular fluid in the descending limb c) passive diffusion of NaCl from the lumen of thin segment of ascending limb into the inner medullary ISF Countercurrent exchanger system – It is a countercurrent system in which transport between inflow and outflow is entirely passive. – Vasa recta - is a countercurrent exchanger - Permeable to water and solutes throughout their length Countercurrent exchange in vasa recta 1. Blood enter with 300 mOsm/kg water 2. Descends through increasingly hypertonic peritubular fluid in medulla. 3. Water diffuses out. Solutes diffuses in until hair-pin turn is reached. 4. Blood then ascents through decreasing hypertonicity and water diffuses in and solute diffuses out. 5. Blood returns to the cortex. Milliosmolality is only slightly higher than when it entered Vasa recta. Countercurrent exchanger system In descending limb – water drawn by osmosis from vasa recta to ISF (hyperosmotic created by countercurrent multiplier) – Solutes diffuse from ISF to vasa recta In ascending limb – solutes diffuse back into ISF - Water is drawn by osmosis back into vasa recta - The function of countercurrent exchange - to retaine solutes in the ISF of medulla - Increase rate of blood flow in vasa recta – reduce time for diffusion of solute from ascending limb back to ISF – gradual loss of solute from medulla – medullary washout - This is prevented by low blood flow - 10 to 20% of kidney blood flow Role of urea Urea - Contributes high solute concentration in ISF - Recirculation of urea assists countercurrent multiplier system and osmotic gradient - Urea excretion is maintained almost at the same level whether the urine is dilute or concentrated. Concentration of Urine ADH and Osmoregualtion - Epithelial cells of CT, CD – variable permeability depending on ADH amount (Post Pit) - ADH - permeability of these cells for water - ADH secretion - significant in 2% changes in plasma osmolality - Degree of ECF dehydration – Osmoreceptor cells in hypothalmus - Hyperosmolality - secretion of ADH - ADH acts on cortical and medullary CDs - water reabsorption Thirst center in hypothalamus - also stimulated by hyperosmolality Relationship among hypothalamus, posterior pituitary and kidney in the regulation of extracellular dehydration Control of hyperosmolality Hypothalamus regulated Thirst – predominant factor for correction of hyperosmolality Diabetes insipidus - Water is not reabsorbed in the CTs and CDs – excreted as urine - Hypotonic tubular condition – absence or severely decreased amount of ADH - k/s diabetes insipidus - Animal with this condition - polyuria ( excess amount of water in urine) - polydipsia (excessive thirst and excessive water intake) - urine formed - dilute, lower than normal specific gravity What are the differences between diabetes melitus and diabetes insipidus Diabetes insipidus and diabetes mellitus What are the differences and similarities between diabetes mellitus and diabetes insipidus Particular Diabetes insipidus Diabetes mellitus cause Lack or deficient ADH +ce of glucose in urine Osmotic diuresis -ce +ce Polyuria + + Polydipsia + + Thirst + + Specificiific gravity ow High Urine content No glucose glucose Urine concentration Normally • Urine concentration may vary depending on multiple factors • In extreme cases in domestic animals – urine-to-plasma osmolal ratio may approach (2400:300); the urine concentration is 8 times that of plasma • In desert rodents – urine-to-plasma ratio (16:1) -- extreme adaption for body water conservation -- water - not available; mostly gained water – metabolic -- water loss minimized for survival Renal failure and reduced urine concentration Acute renal failure - Normal : high O2 supply and high O2 use in renal tissue - Persistently low renal perfusion (low renal blood supply as in shock or renal damage) = decrease in GFR over hours or days = causes acute renal failure Chronic renal failure - If renal failure (impaired GFR) remains for months Renal failure and reduced urine concentration Reduced urine concentration Concentration failure Mostly found in chronic renal diseases - ↓ concentrating ability • More solute remained in functional nephrons - contribute osmotic diuresis • Hypertonicity in medullary ISF not maintained due to - loss of medullary t/s or ↓ blood flow in the vasa recta - ↓Na and Cl transport from the thick segament of ascending limb of loop of Henlen • Damage to cells in CTs and CDs – making less responsive to ADH