Local Anesthetics
advertisement

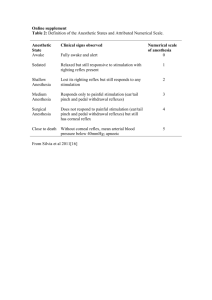
Local Anesthetics Lab. 4 Local Anesthetics (LA) • L.A. reversibly block impulse conduction along nerve axons and other excitable membrane. • A local anesthetic is a drug that causes reversible local anesthesia and a loss of nociception. When it is used on specific nerve pathways (nerve block), effects such as analgesia (loss of pain sensation) and paralysis (loss of muscle power) can be achieved. Mechanism of action of LA • They act by blockade of sodium channels so that: 1- The threshold for excitation increase 2- Impulse conduction slow 3- The rate of rise of the action potential declines, and 4- The ability to generate an action potential is abolished or canceled. Mechanism of action of LA • When the influx of sodium is interrupted, an action potential cannot arise and signal conduction is inhibited. LA drugs bind more readily to sodium channels in activated state, thus onset of neuronal blockade is faster in neurons that are rapidly firing. This is referred to as state dependent blockade. Effect of PH • Local anesthetics are weak bases and are usually formulated as the hydrochloride salt to render them water-soluble. At the chemical's pKa the protonated (ionized) and unprotonated (unionized) forms of the molecule exist in an equilibrium but only the unprotonated molecule diffuses readily across cell membranes. Once inside the cell the local anesthetic will be in equilibrium, with the formation of the protonated (ionized form), which does not readily pass back out of the cell. This is referred to as "ion-trapping". Effect of PH (cont.) • LA are weak bases and their activity increases by increasing PH • This because if large amount of a drug is unpolar, it will facilitate its penetration through the cell membrane • Once the drug has penetrated the lipid barrier and reach its site of action it ionized and the ionized form is responsible for LA activity • Acidosis such as caused by inflammation at a wound partly reduces the action of local anesthetics. This is partly because most of the anesthetic is ionized and therefore unable to cross the cell membrane to reach its cytoplasmic-facing site of action on the sodium channel. • Local anesthetics block conduction in the following order: small myelinated axons (e.g. those carrying nociceptive impulses), non-myelinated axons, then large myelinated axons. Thus, a differential block can be achieved (i.e. pain sensation is blocked more readily than other sensory modalities). Methods of Administration • 1- Surface anesthesia: direct application of the drug on the surface such as skin and wounds. • 2- Infiltration anesthesia: injection of LA in subcutaneous tissue in order to paralyze nerve endings at the site of action. • 3- Nerve block: LA is injected in the vacinity of major nerve such as teeth Methods of Administration • 4- Epidural anesthesia: injection of LA into the epidural space. • 5- Sympathetic block: inject LA around sympathetic nerves • 6- Spinal anesthesia: injection of LA into subarachnoid space in the lumber region Clinical use • 1- Systemic use as antiarrhythemic agents e.g. Lidocaine • 2- Locally use to produce anesthesia Clinical LA • Clinical local anesthetics belong to one of two • • classes: 1- aminoamide and 2- aminoester Synthetic local anesthetics are structurally related to cocaine. They differ from cocaine mainly in that they do not produce hypertension or local vasoconstriction, with the exception of Ropivacaine and Mepivacaine that do produce weak vasoconstriction. Classification of LA 1-Esters A- esters of P- amine benzoic acid e.g. Procaine B- Esters of benzoic acid e.g. Cocaine • Benzocaine • Chloroprocaine • Cyclomethycaine • Dimethocaine/Larocaine • Propoxycaine • Procaine/Novocaine • Proparacaine • Tetracaine/Amethocaine Classification of LA 2- • • • • • • • • • • • Amide e.g. Lidocaine Articaine Bupivacaine Cinchocaine/Dibucaine Etidocaine Levobupivacaine Lidocaine/Lignocaine Mepivacaine Piperocaine Prilocaine Ropivacaine Trimecaine Classification of LA 3- Combinations • Lidocaine/prilocaine (EMLA) 4- Natural local anesthetics e.g. Saxitoxin and Tetrodotoxin • Naturally occurring local anesthetics not derived from cocaine are usually neurotoxins, and have the suffix -toxin in their names. Unlike cocaine produced local anesthetics which are intracellular in effect, saxitoxin & tetrodotoxin bind to the extracellular side of sodium channels. Potency LA • The potency of LA is vary from one to another where the potency and duration of action are increased with decreased water solublility of the agent for example • Procaine ˃˃˃˃ 1 more water soluble • Lidocaine ˃˃˃˃ 4 • Tetracaine ˃˃˃˃ 16 Frog’s plexus method • “Foot withdrawal reflex of frog” • Principle: • The skin of the frog is very sensitive to diluted HCL and will reflex by withdrawing its leg when immersed in HCL Procedure 1- Decapitaion the frog (avoid pithing the spinal cord) 2- Make a transverse incision in the abdominal wall just below the xiphoid cartilage and eviscerate the abdomen carefully to form abdominal sac and expose the lumbar plexus without damaging it 3- suspend the frog in a stand and test the withdrawal reflex with 0.1 N HCL by immersing one foot in HCL and avoid touching the bottom of the beaker. 4- remove the acid and wash immediately with tap water N.B. the withdrawal reflex time should not exceed 10 seconds and the contact with HCL too. 5- Administer 1 ml of LA solution in the abdominal sac of the frog and observe the zero time. 6- Test the withdrawal reflex at 3 minutes interval and wash with tap water after each exposure to the acid, observe the time at which the absence of withdrawal reflex occurs Onst time: is the time from adding LA untill the acid fails to provoke withdrawal of the foot Recovery time: is the time in minutes from washing the LA till the appearance of the withdrawal reflex in response to HCL. 7- Tabulate your results and determine which of LA is more rapid in its action than the other. The time interval Procaine Lignocaine 3 - - 6 - + 9 - 12 - 15 - 18 + • Negative (-)= means the presence of the withdrawal reflex (the drug has no activity). • Positive (+)= means the absence of the withdrawal reflex (the drug has activity and blocks sodium channels) • Conclusion: From the table we conclude that lignocaine is more rapid in inducing local anesthesia than procaine