The insurance
advertisement

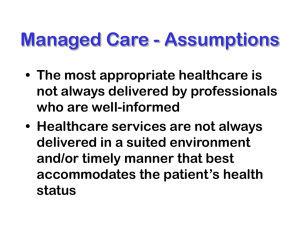
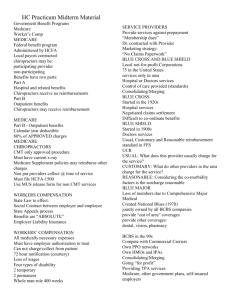
MANAGED CARE MANAGED CARE PLANS COMBINE THE DELIVERY OF HEALTH CARE WITH THE FINANCING OF THAT CARE. IN A MANAGED CARE PLAN, SUCH AS A HEALTH MAINTENANCE ORGANIZATION (HMO) OR A PREFERRED PROVIDER ORGANIZATION (PPO), YOU RECEIVE YOUR HEALTH CARE FROM A GROUP OF PHYSICIANS, HOSPITALS, AND OTHER SERVICE PROVIDERS SELECTED BY THE PLAN. IN EXCHANGE, YOU PAY A SET MONTHLY FEE FOR THE SERVICES YOU RECEIVE. Goals of Managed Health Care Plans Provide high quality care in an environment that controls cost Care is medically necessary and appropriate Goals (Continued) Care is rendered by the most appropriate provider Care is rendered in the most appropriate, least-restrictive environment TYPES OF MANAGED CARE PLANS HEALTH MAINTENANCE ORGANIZATION GROUP AND STAFF MODEL HMO’S ARE THE MOST RESTRICTIVE AND PROVIDE FEWER CHOICES OF PROVIDERS TO CONSUMERS. ON THE OTHER HAND, THIS MODEL OFTEN OFFERS ONESTOP CARE WHICH MEANS THAT ALL YOUR DOCTORS, AS WELL AS LABORATORY AND X-RAY SERVICES ARE X-RAY SERVICES ARE LOCATED IN ONE MEDICAL FACILITY. IN A GROUP OR STAFF HMO, YOU MUST CHOOSE A PRIMARY PHYSICIAN. IF YOU DON’T, THEY WILL CHOOSE ONE FOR YOU. – INDIVIDUAL PRACTICE ASSOCIATONS (IPA’S) INDIVIDUAL PRACTICE ASSOCIATIONS (IPA’S) ARE A LESS RESTRICTIVE FORM OF HMO THAN THE GROUP OR STAFF MODEL. INDIVIDUAL PHYSICIANS PRACTICING IN THEIR OWN OFFICES ARE UNDER CONTRACT TO A SEPARATE GROUP, CALLED AN “IPA” THAT, IN TURN, CONTRACTS WITH AN HMO. THE HMO PROVIDES YOU WITH A LIST OF PARTICIPATING PHYSICIANS FROM WHICH YOU MAY CHOOSE YOUR PRIMARY CARE DOCTOR. VISITS TAKE PLACE IN THE DOCTOR’S OFFICE. IF YOU REQUIRE SPECIALITY CARE, YOUR PRIMARY CARE DOCTOR REFERS YOU TO A PARTICIPATING SPECIALIST. BY FAR THE LARGEST NUMBER OF HMO MEMBERS ARE ENROLLED IN THE IPA MODEL. PHYSICIANS MAY BELONG TO MORE THAN ONE HMO AND ALSO MAY CONTINUE TO SEE FEE-FOR-SERVICE PATIENTS IN THEIR OFFICE. POINT OF SERVICE (POS) POINT OF SERVICE (POS) PLANS PERMIT MEMBERS GREATER CHOICE AND FLEXIBILITY BY ALLOWING YOU THE OPTION OF GOING “OUT OF PLAN” TO USE NON-HMO PROVIDERS. IF YOU GO “OUT OF PLAN,” YOU MUST PAY MORE, TYPICALLY IN THE FORM OF HIGH COINSURANCE AND DEDUCTIONS. – PREFERRED PROVIDER ORGANIZATION (PPO) PREFERRED PROVIDER ORGANIZATION (PPO) ARE NETWORKS OF DOCTORS AND HOSPITALS THAT HAVE AGREED TO GIVE THE SPONSORING ORGANIZATION DISCOUNTS ON THEIR USUAL RATES. (USUALLY AN EMPLOYER OR INSURANCE COMPANY). SOME PPO’S USE PRIMARY CARE PHYSICIANS AS GATEKEEPERS. IN OTHERS, YOU MAY CHOOSE YOUR OWN DOCTORS AND VISIT SPECIALISTS WITHOUT PERMISSION FROM A GATEKEEPER. PPO’S OFFER YOU THE GREATEST FREEDOM AMONG MANAGED CARE PLANS IN SELECTING HEALTH CARE PROVIDERS BUT PPO PREMIUMS ARE USUALLY SOMEWHAT HIGHER THAN HMO PREMIUMS AND THERE IS LESS COORDINATION OF CARE. DEFINED CARE Employer sponsored Defined Contribution Health plans. Provides an allowance that empowers consumers to purchase and select from a wide menu of benefit options •MANAGED CARE VS. TRADITIONAL HEALTH INSURANCE •RECEIVING CARE GATEKEEPERS UNDER FEE-FOR-SERVICE INSURANCE OR TRADITIONAL HEALTH INSURANCE, YOU CAN CHOOSE ANY LICENSED PHYSICIAN TO BE YOUR PERSONAL DOCTOR AND YOU CAN THE SERVICES OF ANY HEALTH CARE FACILITY OR SERVICES. UNDER MANAGED CARE, MEMBERS RECEIVE CARE THAT IS PROVIDED DIRECTLY OR AUTHORIZED BY THE MANAGED CARE PLAN. THE PRIMARY CARE DOCTOR YOU CHOOSE BECOMES YOUR PERSONAL PHYSICIAN AND COORDINATES YOUR CARE. THE DOCTOR ACTS A “GATEKEEPER,” TREATING YOU DIRECTLY OR AUTHORIZING YOU TO HAVE TESTS, SEE A SPECIALIST, OR ENTER A HOSPITAL. THE “GATEKEEPER” ARRANGEMENT IS DESIGNED TO PROVIDE THE NECESSARY CARE AT THE LOWEST COST AND TO AVOID GIVING UNNECESSARY CARE. – QUALITY REVIEW UNDER TRADITIONAL HEALTH INSURANCE PLANS, DOCTORS PRACTICE INDEPENDENTLY WITH LITTLE OR NO ASSESSMENT OF THEIR PERFORMANCE BY THEIR PEERS OR GOVERNMENT REGULATORS. MANAGED CARE PLANS USUALLY HAVE QUALITY REVIEW PROCEDURES THAT MAY INCLUDE INTERNAL AND EXTERNAL QUALITY ASSURANCE PROGRAMS. PLANS “FEDERALLY QUALIFIED” TO PROVIDE HEALTH CARE TO MEDICARE OR MEDICAID ENROLLEES, UNDER LAW MUST HAVE QUALITY ASSURANCE PROGRAMS. THE OVERALL PERFORMANCE OF THE PLAN IS MONITORED THROUGH GOVERNMENT OVERSIGHT, PATIENT SATISFACTION SURVEYS, DATA FROM GRIEVANCE PROCEDURES, AND INDEPENDENT REVIEWS. –UTILIZATION REVIEW MANAGED CARE PLANS REVIEW THE MEDICAL CARE PROVIDED BY YOUR DOCTORS TO DETERMINE WHETHER OR NOT IT IS APPROPRIATE AND NECESSARY. WHEN HOSPITAL CARE IS INDICATED, OTHER FACTORS AND SAFEGUARDS IN THE UTILIZATION REVIEW INCLUDE: CARE IN ADVANCE. WITHOUT IT, THE PLAN MAY PREADMISSION CERTIFICATION: APPROVAL FOR NOT PAY FOR NONEMERGENCY SERVICES. CONCURRENT REVIEW: MANAGED CARE PLANS MONITOR YOUR HOSPITAL STAYS TO BE SURE THEY ARE NO LONGER THAN ABSOLUTELY NEEDED AND THAT ALL TESTS AND PROCEDURES ORDERED ARE MEDICALLY NECESSARY. DISCHARGE PLANNING: PLANS WANT TO KEEP HOSPITAL STAYS TO THEIR SHORTEST APPROPRIATE LENGTH. IF NECESSARY, THE PLAN WILL ARRANGE POST-HOSPITAL CARE, INCLUDING NURSING HOME OR HOME HEALTH CARE. CASE MANAGEMENT: CASE PLANS ARE DEVELOPED FOR COMPLICATED CASES TO BE SURE CARE IS COORDINATED AND PROVIDED IN THE MOST COST-EFFECTIVE MANNER. SECOND SURGICAL OPINIONS: PLANS MAY REQUIRE A SECOND OPINION BEFORE SCHEDULING ELECTIVE SURGERY. THE SECOND PHYSICIAN MAY BE ASKED TO JUDGE THE NECESSITY OF THE SURGERY AND ALSO TO EXPRESS AN OPINION ON THE MOST ECONOMICAL, APPROPRIATE PLACE TO PERFORM THE SURGERY. –PAYING FOR CARE FOR MOST PEOPLE WITH TRADITIONAL HEALTH INSURANCE, PREMIUMS ARE ONLY ONE PART OF THE COST. CONSUMERS ALSO PAY DEDUCTIBLES, COINSURANCE, AND THE COST OF SERVICES THAT ARE NOT COVERED. WITH MANAGED CARE, OUT-OFPOCKET COSTS ARE GENERALLY LOWER, AND THERE IS FAR LESS PAPERWORK FOR PLAN MEMBERS TO CONTEND WITH. –THE PROS AND CONS HMO STAFF MODEL: PROS: CENTRALIZED FACILITY WHERE CARE IS PROVIDED AND COORDINATED; LOW COPAYMENTS; PREVENTATIVE CARE; NO CLAIM FORMS. CONS: MUST USE DOCTOR IN THE HMO; PLAN MUST APPROVE TREATMENT AND MAKE REFERRALS. HMO INDIVIDUAL PRACTICE ASSOCIATION: PROS: PROVIDERS USE THEIR OWN OFFICES; LOW COPAYMENTS; PREVENTATIVE CARE; NO CLAIM FORMS. CONS: MUST USE DOCTORS IN THE HMO; PLAN MUST APPROVE TREATMENT AND MAKE REFERRALS. HMO POINT OF SERVICE: PROS: MORE CHOICE OF PROVIDERS OUTSIDE THE NETWORK; LOWER COST WITHIN THE NETWORK; PREVENTIVE CARE COVERED. CONS: HIGHER COST OUTSIDE THE NETWORK; OUT-OF-NETWORK COVERAGE MAY BE LIMITED; PLAN MUST SOMETIMES APPROVE TREATMENT AND MAKE REFERRALS. PREFERRED PROVIDER ORGANIZATION (PPO): PROS: CHOICE OF STAYING IN OR GOING OUT OF THE NETWORK FOR CARE. LOWER COST IF PROVIDERS WITHIN NETWORK ARE USED. CONS: HIGH COST OUTSIDE THE NETWORK; ADDITIONAL PAPERWORK TO SECURE APPROVAL FOR SOME SERVICES; LIMITED COORDINATION TRADITIONAL HEALTH INSURANCE: PROS: UNRESTRICTED CHOICE OF PROVIDER. CONS: USUALLY MORE EXPENSIVE; LITTLE OR NO COORDINATION OF CARE; PREVENTIVE CARE USUALLY NOT COVERED; CLAIM FORMS TO FILE. KEY TERMS AND CONCEPTS – MEMBERS: IN MANAGED CARE EACH PATIENT WITH INSURANCE COVERAGE UNDER A HEALTH PLAN IS CALLED A MEMBER. OTHER TERMS INCLUDE ENROLLEES AND COVERED LIVES. PER MEMBER PER MONTH IS A RELATIVE MEASURE, THE RATIO, BY WHICH MOST EXPENSE AND REVENUE, AND MANY UTILIZATION COMPARISONS ARE MADE. MEDICAL MANAGEMENT TERMS QUALITY MANAGEMENT INVOLVES ENSURING MEMBERS ARE GETTING ACCESSIBLE AND AVAILABLE CARE, DELIVERED WITHIN COMMUNITY STANDARDS; AND ENSURING A SYSTEM TO IDENTIFY AND CORRECT PROBLEMS, AND TO MONITOR ONGOING PERFORMANCE. UTILIZATION MANAGEMENT INVOLVES COORDINATING HOW MUCH OR HOW CARE IS GIVEN FOR EACH PATIENT, AS WELL AS THE LEVEL OF CARE. THE GOAL IS TO ENSURE CARE IS DELIVERED COSTEFFECTIVELY, AT THE RIGHT LEVEL, AND DOESN’T USE UNNECESSARY RESOURCES. OUTCOMES MANAGEMENT DETERMINES THE CLINICAL END-RESULTS ACCORDING TO DEFINED VARIOUS CATEGORIES AND THEN PROMOTE USE OF THOSE CATEGORIES WHICH YIELD IMPROVED OUTCOMES. DEMAND MANAGEMENT A PROGRAM ADMINISTERED BY THE PROVIDER ORGANIZATION TO MONITOR AND PROCESS MANY TYPES OF INITIAL MEMBER REQUESTS FOR CLINICAL INFORMATION AND SERVICES. DISEASE MANAGEMENT INVOLVES ASPECTS OF CASE AND OUTCOMES MANAGEMENT, BUT APPROACH FOCUSES ON SPECIFIC DISEASES, LOOKING AT WHAT CREATES THE COSTS, WHAT TREATMENT PLAN WORKS, EDUCATING PATIENTS AND PROVIDERS, AND COORDINATING CARE AT ALL LEVELS. HOSPITAL, PHARMACY, PHYSICIAN, ETC. SHARING FINANCIAL RISK CAPITATION CAPITATION MEANS PAY A FIX AMOUNT OF MONEY PER PERSON (PER CAPITA). CAPITATION PUTS A LID ON PAYMENTS PER PERSON THAT OTHERWISE MIGHT CHANGE UNDER A FEE-FOR-SERVICE SYSTEM. PROVIDERS ARE AT FULL FINANCIAL RISK FOR THE SERVICES CAPITATED. THE PROVIDER IS PAID A FIX AMOUNT PER MEMBER ENROLLED, REGARDLESS OF THE NUMBER OF SERVICES DELIVERED TO THAT MEMBER. WHAT THE FUTURE HOLDS RIGHT AROUND THE CORNER Managed Care Backlash will become a permanent fixture, without producing radical reform. However, pharmaceutical costs may surpass managed care backlash in the number one health care public “hot seat.” PPO and Point of Service enrollment gains will continue. HMO’S will continue to soften management techniques Plan premium & provider costs increases will continue Provider clout over health plans will continue to solidify. Employers will grudgingly accept price increases as long as the labor market is tight. Medicare HMOs won’t disappear despite pundit’s warnings to the contrary. LONGER TERM.. When the economy diminishes, more proactive changes will occur. Defined Care and consumerism will become a major factor. New medical technology advancements will dictate future medical management techniques. Legislative reform will remain incremental, not radical, unless there is a devastating recession where uninsured numbers swell. End of lecture for Monday, October 17th, 2011, 6th Period Questions? MANAGED CARE FACTS, TERMS, AND DEFINITIONS FACTS ABOUT MANAGED CARE NUMBER OF HMOS IN THE UNITED STATES = 574 NUMBER OF PPOS IN THE UNITED STATES = 1036 NUMBER OF AMERICANS IN HMOS = 79.3 MILLION NUMBER OF AMERICANS IN PPOS = 89.1 MILLION NUMBER OF AMERICANS IN ALL MANAGED CARE PROGRAMS = 206 MILLION PERCENTAGE OF INSURED EMPLOYEES IN MANAGED CARE HEALTH PLANS = 66% PERCENTAGE OF MEDICARE ENROLLEES IN HMOS = 9% PERCENTAGE OF MEDICAID ENROLLEES IN HMOS = 19.4% PERCENTAGEOF MDS WITH AT LEAST ONE MANAGED CARE CONTRACT = 75% PERCENTAGE OF MDS WITH AT LEAST ONE HMO CONTRACT = 48% PERCENTAGE OF HMOS THAT ARE FORPROFIT = 69% PERCENTAGE OF HMOS THAT ARE NOT-FORPROFIT = 42.2 % PERCENTAGE OF HMOS WITH LISTS OF APPROVED PRESCRIPTION DRUGS – 100% OrganizationManaged Care enrollment WellPoint, Inc. 27,236,851 UnitedHealth Group, Inc. 21,684,629 Aetna, Inc. 14,172,723 Health Care Service Corporation 12,262,905 CIGNA Health care, Inc. 9,064,024 Kaiser Permanente 8,825,581 Humana, Inc. 7,699,106 Blue Cross Blue Shield of Michigan 4,937,591 Highmark, Inc. 4,739,178 HIP Health Plan of New York 4,285,194 Total (for US) 206,226,739 MANAGED CARE TERMS AMBULATORY CARE ALL TYPES OF HEALTH SERVICES THAT ARE PROVIDED ON AN OUTPATIENT BASIS, IN CONTRAST TO SERVICES PROVIDED IN THE HOME OR TO PERSONS WHO ARE HOSPITAL INPATIENTS. CASE MANAGEMENT THE PROCESS BY WHICH ALL HEALTH RELATED MATTERS OF A CASE ARE MANAGED BY A PHYSICIAN OR NURSE OR DESIGNATED HEALTH PROFESSIONAL. PHYSICIAN CASE MANAGERS COORDINATE DESIGNATED COMPONENTS OF HEALTH CARE, SUCH AS APPROPRIATE REFERRAL TO CONSULTANTS, SPECIALISTS, HOSPITALS, ANCILLARY PROVIDERS AND SERVICES. CASE MANAGEMENT IS INTENDED TO ENSURE CONTINUITY OF SERVICES AND ACCESSIBILITY TO OVERCOME RIGIDITY, FRAGMENTED SERVICES, AND THE MISUTILIZATION OF FACILITIES AND RESOURCES. COPAYMENT A COST-SHARING ARRANGEMENT IN WHICH A MEMBER PAYS A SPECIFIED CHARGE FOR A SPECIFIED SERVICE. THE MEMBER IS USUALLY RESPONSIBLE FOR PAYMENT AT THE TIME THE SERVICE IS RENDERED. COST SHARING A GENERAL SET OF FINANCING ARRANGEMENTS IN WHICH A COVERED MEMBER MUST PAY A PORTION OF THE COSTS ASSOCIATED WITH RECEIVING CARE, E.G., CO-PAYMENT, COINSURANCE OR DEDUCTIBLE. DIAGNOSIS RELATED GROUPS (DRG) A SYSTEM OF CLASSIFICATION FOR INPATIENT HOSPITAL SERVICES BASED ON DIAGNOSIS, AGE, SEX, AND PRESENCE OF COMPLICATIONS. IT IS USED AS A MEANS OF IDENTIFYING COSTS FOR PROVIDING SERVICES ASSOCIATED WITH THE DIAGNOSIS AND AS A MECHANISM TO REIMBURSE HOSPITAL AND SELECTED OTHER PROVIDERS FOR SERVICES RENDERED. FEE-FOR-SERVICE A PAYMENT SYSTEM BY WHICH DOCTORS, HOSPITALS AND OTHER PROVIDERS ARE PAID A SPECIFIC AMOUNT FOR EACH SERVICE PERFORMED AS IT IS RENDERED AND IDENTIFIED BYA CLAIM FOR PAYMENT. FORMULARY A LIST OF SELECTED PHARMACEUTICALS AND THEIR APPROPRIATE DOSAGES FELT TO BE THE MOST USEFUL AND COST EFFECTIVE FOR PATIENT CARE. IN SOME MANAGED CARE PLANS, PROVIDERS ARE REQUIRED TO PRESCRIBE FROM THE FORMULARY. GROUP OR NETWORK HMO A MANAGED CARE ORGANIZATION IN WHICH THE MANAGED CARE ORGANIZATION CONTRACTS WITH MORE THAN ONE PHYSICIAN GROUP, AND MAY CONTRACT WITH SINGLE AND MULTISPECIALITY GROUPS THAT WORK OUT OF THEIR OWN OFFICE FACILITY. THE NETWORK MAY OR MAY NOT PROVIDE CARE EXCLUSIVELY FOR THE MANAGED CARE ORGANIZATION’S MEMBERS. CENTER FOR MEDICARE AND MEDICAID CMS IS THE FEDERAL AGENCY THAT ADMINISTERS THEMEDICARE AND MEDICAID PROGRAMS, AND WORKS TO ASSURE THAT THE BENEFICIARIES ENROLLED IN THESE PROGRAMS HAVE ACCESS TO HIGH QUALITY CARE. INDEMNITY PLAN A PLAN WHICH REIMBURSES PHYSICIANS FOR SERVICES PERFORMED, OR BENEFICIARIES FOR MEDICAL EXPENSES INCURRED (RETROACTIVE PAYMENT). SUCH PLANS ARE DIFFERENT FROM GROUP HEALTH PLANS, WHICH RECEIVE A SPECIFIC AMOUNT IN ADVANCE TO COVER ALL OR CERTAIN HEALTH CARE SERVICES FOR A SPECIFIC POPULATION (PROSPECTIVE PAYMENT). INDIVIDUAL PRACTICE ASOCIATION (IPA) MODEL A MANAGED CARE ORGANIZATION THAT CONTRACTS WITH INDIVIDUAL PRACTITIONERS OR AN ASSOCIATION OR INDIVIDUAL PRACTICES TO PROVIDE HEALTH CARE SERVICES IN RETURN FOR A NEGOTIATED FEE. THE INDIVIDUAL PRACTICE ASSOCIATION, IN TURN, COMPENSATES ITS PHYSICIANS ON A PER CAPITA, FEE SCHEDULE, OR OTHER AGREED-UPON BASIS. LOCK-IN A CONTRACTUAL PROVISION BY WHICH MEMBERS, EXCEPT IN CASES OF UNFORESEEN OUT-OF-AREA URGENTLY NEEDED CARE OR EMERGENCY CARE, ARE REQUIRED TO RECEIVE ALL THEIR CARE FROM THE MANAGED CARE PLAN’S NETWORK OF HEALTH CARE PROVIDERS. MANAGED CARE ORGANIZATION AN ENTITY THAT INTEGRATES FINANCING AND MANAGEMENT WITH THE DELIVERY OF HEALTH CARE SERVICES TO AN ENROLLED POPULATION. AN MCO PROVIDES, OFFERS, OR ARRANGES COVERAGE OF DESIGNATED HEALTH SERVICES NEEDED BY MEMBERS FOR A FIXED, PREPAID AMOUNT. MEDICALLY NECESSARY SERVICES OR SUPPLIES WHICH MEET THE FOLLOWING: • THEY ARE APPROPRIATE AND NECESSARY FOR THE SYMPTOMS, DIAGNOSIS, OR TREATMENT OF THE MEDICAL CONDITION; • THEY ARE PROVIDED FOR THE DIAGNOSIS OR DIRECT CARE AND TREATMENT OF MEDICAL CONDITIONS; • THEY MEET THE STANDARDS OF GOOD MEDICAL PRACTICE WITHIN THE MEDICAL COMMUNITY OF THE SERVICE AREA; • THEY ARE NOT PRIMARILY FOR THE CONVENIENCE OF THE PATIENT OR PROVIDER; • THEY ARE THE MOST APPROPRIATE LEVEL OR SUPPLY OF SERVICE WHICH CAN SAFELY BE PROVIDED. MEDICARE MANAGED CARE MEDICARE MANAGED CARE IS A HEALTH CARE OPTION YOU CAN CHOOSE TO RECEIVE YOUR MEDICARE BENEFITS. MANAGED CARE PLANS HAVE CONTRACTS WITH THE GOVERNMENT, SPECIFICALLY THE HEALTH CARE FINANCING ADMINISTRATION, TO PROVIDE YOUR MEDICARE BENEFITS. MEDICARE SUPPLEMENT INSURANCE PRIVATE HEALTH INSURANCE THAT PAYS CERTAIN COSTS NOT COVERED BY FEE-FORSERVICE MEDICARE, SUCH AS MEDICARE COINSURANCE AND DEDUCTIBLES. POINT-OF-SERVICE (POS) OPTION A MEMBER’S OPTION TO CHOOSE TO RECEIVE A SERVICE FROM OUTSIDE THE PLAN’S NETWORK OF PROVIDERS FOR AN ADDITIONAL FEE SET BY THE PLAN. GENERALLY, THE LEVEL OF COVERAGE IS REDUCED FOR SERVICES ASSOCIATED WITH THE USE OF NON-PARTICIPATING PROVIDERS. PREFERRED PROVIDERS PHYSICIANS, HOSPITALS, AND OTHER HEALTH CARE PROVIDERS WHO CONTRACT TO PROVIDE HEALTH SERVICES TO PERSONS COVERED BY A PARTICULAR HEALTH PLAN. PREFERRED PROVIDER ORGANIZATION (PPO) A HEALTH CARE DELIVERY SYSTEM THAT CONTRACTS WITH PROVIDERS OF MEDICAL CARE TO PROVIDE SERVICES AT DISCOUNTED FEES TO MEMBERS. MEMBERS MAY SEEK CARE FROM NON-PARTICIPATING PROVIDERS BUT GENERALLY ARE FINANCIALLY PENALIZED FOR DOING SO BY THE LOSS OF THE DISCOUNT AND SUBJECTION TO COPAYMENTS AND DEDUCTIBLES. PRIMARY CARE NETWORK (PCN) A GROUP OF PRIMARY CARE PHYSICIANS WHO SHARE THE RISK OF PROVIDING CARE TO MEMBERS OF A GIVEN HEALTH PLAN. PRIMARY CARE PHYSICIANS (PCP) THE PHYSICAN THAT SERVES AS THE INITIAL CONTACT BETWEEN THE MEMBER AND THE MEDICAL CARE SYSTEM. THE PCP IS USUALLY A PHYSICIAN WHO IS TRAINED IN ONE OF THE PRIMARY CARE SPECIALITIES, AND WHO TREATS AND IS RESPONSIBLE FOR COORDINATING THE TREATMENT OF MEMBERS ASSIGNED TO HIS OR HER PANEL. PROVIDER A HEALTH CARE PROVIDER OR FACILITY THAT IS PART OF THE MANAGED CARE PLAN’S NETWORK USUALLY HAVING FORMAL ARRANGEMENTS TO PROVIDE SERVICES TO THE PLAN’S MEMBERS. QUALITY ASSURANCE A FORMAL METHODOLOGY AND SET OF ACTIVITIES DESIGNED TO ASSESS THE QUALITY OF SERVICES PROVIDED. QUALITY ASSURANCE INCLUDES FORMAL REVIEW OF CARE, PROBLEM IDENTIFICATION, AND CORRECTIVE ACTIONS TO REMEDY ANY DEFICIENCIES AND EVALUATION OF ACTIONS TAKEN. STAFF MODEL THIS MANAGED CARE ORGANIZATION MODEL EMPLOYS PHYSICIANS TO PROVIDE HEALTH CARE TO ITS MEMBERS. ALL PREMIUMS AND OTHER REVENUES ACCRUE TO THE MANAGED CARE ORGANIZATION, WHICH COMPENSATES PHYSICIANS BY SALARY. End of lecture for 6th Period, October 19th - 2011 Questions?