Webinar Transcript
advertisement

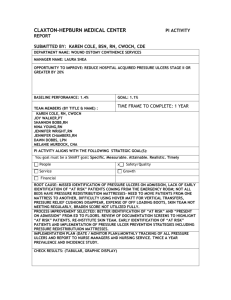
Good morning everyone thank you for joining us for this conference, before turning it over to your moderator, you will be on an open line, any noise will come through, please take this opportunity to turn your microphone is on mute. As I was indicated -- indicating should you need assistance, during the conference please press star zero, and I will come to your aid immediately. You can talk directly to a moderator during question-and-answer time, I will turn it over to Tracy. Welcome to the Affinity Call, we have this speak -- special speaker, who has been doing great work in Minnesota, on the skincare call -- skincare, her name is Julie she is the senior director of the hospital association, she has worked on patient safety and quality for nine years, she collaborates with the Minnesota Department of Health, reporting law activities, she manages reporting agency -- filling out and analyzing events, she is currently managing statewide collaborative to address the top recording adverse advance -- events, please welcome Julie to our call. Thank you so much Tracy. Would you like to go to my first slide. Our work around pressor ulcer started years ago, it has been centered around our save skin program, -safe skin program. The way it is has been structured, when I look at it when we first started our journey, most best practices out there were for long-term care, a short while ago it seems like most best practices are going to acute care, our job was to say what is the best practice for preventing pressure ulcers, we identified best practices. At the same time we did not put out a protocol, we wanted to see about implementing these practices, we implemented the safety and, -- safe skin, it helps get those practices implemented, and sustained those in the long-term. This faith -- SAFE, S stands for identifying champions from I -- all different teams. Having a coordinator is important, you have somebody very passionate about the work, they are leading the work, and they go to a different position or leave the organization, that work falls away. It is important to have a coordinator and a team of people supporting them, so if one person leaves the team does not fall apart. It is the foundation under VS -- under the S. Making sure you have a correct data, when I first started to do this work what I would hear from the organizations, units did not want to share data, they are competitive they do not want to show that, to make that leap was significant back then. Analyzing your data. Getting leadership involved and making sure they are steady and expectations and the support that is needed, that you have good education, for orientation, on an ongoing basis. E is for education, for patients and families, what we have seen in all different initiatives that we worked on, E is where we scored lowest. Which was surprising to me at first, we have not done a good job of education our patients and making them a part of the team, we have done a lot of work around that area. The skin bundle, the Risk Assessment, I earned -- learned pretty early it is not skin assessment, keeping pressure off, that is most important element, we have found over the years we need to re-position our patients and continue to do that consistently. And then optimizing nutrition what we have seen over the years is 40% that is a significant component of the bundle -- we have streamlined them into place, if you put them into place you should have a strong faith -- safe skin program. If you go through how that is structured, at hospitals there is a web-based system, do we have these best practices in place, at the end of the audit, these are your gaps the organization can take that back which are the ones that we can address and what are the priorities for the quarter, they go back on a quarterly basis, did they change any of those guesses, and they can evolve the practice and track those over time. They will get fewer overtime. They like that because they could say here are the things that are the things I can work with the complete list, instead of just having a best practices in not knowing where to start. They really like the structure. The other things we've really learned over the years is how could concurrent pressure, we started out quarterly PNI studies, some of them were doing annual studies, what we have talked about over the years that is only four days out of 365 days, we really need to be looking at them as they occur. What this does is let you intervene quicker. If we are fighting the pressure ulcers as they are happening, you could put a bunch in place, it helps the awareness of the staff, they are looking for pressor -- pressure ulcers. We will report them on an ongoing basis. We hold quarterly webinars, like you are doing today. We also have a group that has been meeting for a number of years, has been very wonderful. What we have found as we done our work, as you delve further, you get to the point where there is not evidence everything you are encountering. For some of the areas we need to have an approach where we bring the evidence together, where it is lacking we use consensus. Next slide. This shows the progress to our calls in action, when we started out, we did not know how we would there, we only had 59% of those practices in place. What I found for all initiatives that is where we start. Only a little half, we have made progress in the first year and a half, and by the end of 2 to 3 years, we were 95% across all hospitals, we had a really good foundation. I think the important art of this is -- part of this is, we didn't just put this out and step away from it, it needs to be a continuous practice of learning, feeding it back into the program. We have learned very interesting things over the years. What we have found not too surprising, there is been attention paid, -- there is not been much out there, the Straits -- stage III and four, we knew we had to address that, there wasn't much out there, we had to bring together wound care nurses, and oh are -- OR specialist then. -This was surprising how high this was to us, we found actually when we started to focus on pressor -- pressure ulcers, we were not experiencing more device pressure ulcers is is known -- ulcers. There weren't very much out there for best part this, we would brought our -- we brought our nurses in, all the respiratory devices, and big areas we seem pressure ulcers under the chin from cervical collars, any kind of device you have you can get a pressure ulcer. We are seeing a lot from the devices. -- We have actually eliminated pressure ulcers in [Indiscernible]. Also in our data, -- can go to the previous slide to -- please. We knew that we had war -- more work to do around a critical patient, the repositioning, the most common reason is patient preference, we were not doing a good job -- I talked about patient education and working with patients and families and helping them to understand the importance of repositioning, even though they have been comfortable, it is important for them to reposition. And also in the ICU, we looked at where they were occurring, 53% were occurring on the backside. We knew the patients in the ICU were laying on their back way too long without repositioning. I just put in here the different recommendations and guidance that came out of the data. We have prevention in the ORs -- and the respiratory devices. Next slide. We have started an initiative around save skin -- safe skin in the ICU, we have asked them to pledge their support, reposition is so important keeping them moving, floating the hills off the bed, that is important. And also to redistribute pressure. Often you had a patient that could not reposition easily, a consult was put in for a wound care nurse to see them, the nurse would come in to see them, they would order another bed, and by that time they were well on the road with developing a pressure ulcer. If you know your patient is critically ill, that it will be difficult to reposition them, or if they are coming out of OR and will not be able to be repositioned for a while, we need to be proactive about that. The fourth one is if a patient is not able to provide documentation, that document of the patient, if they could not be repositioned, the we assumed that, but they could, doesn't mean that they cannot be repositioned tomorrow. This is a newer best practice that hospitals are starting to implement. We can impact, if you cannot reposition that patient at least every two hours, 30°, you reposition them 15° and do it every hour, we have seen critically ill patients that have worked well with this, it has made a big impact. Devices are very significant, making sure that we are looking under devices, and doing skin inspections. What we have done is look at best practices and we have put them into a safe skin 2.0, we are ready to build on that to highlight the practices I just talked about. So now we have a safe skin 2.0 roadmap that incorporates these additional best practices, our roadmap group had a good foundation, it follows that same infrastructure that I mentioned with safe skin, next slide. How does that impact our data? Just a couple data slides. This is our patient safety indicator data, if you know looking at the administrative data, this is one measure. We've been happy to see that we have a very low ratio for her ulcer pressures -- pressure ulcers. And then the importance of that, 83% decrease in our pressor -- pressor office -- pressure ulcer rate. Next slide please. Some of the key learnings, I've mentioned some of these, I will go with them weekly, engaging the full team, we have wonderful culture shifts in the engaging all of the other team members. Respiratory therapy has not been involved looking in pressure ulcers and been a part of that team, the ORs, what I've heard from the wound care nurses is that I cannot get my foot in the door to talk about pressure ulcers. Keeping patients moving, we have found that there are very few patients that cannot be shifted, if not 30 trees, -- if not 30°, then 15. Then the importance of devices. The biggest thing is shifting in culture, prior to working on safe skin, is what I hear staff saying, if I could save their skin, that is secondary to saving life, what I hear now is that we can save the patients, we can also save their skin. There is been a big shift in culture. We have a save our skin recognition program, that would likely have developed a pressure ulcer, the nominations can be nominated by the teams. The first slide here, is a patient that we made hospitalized for 20 months, they were critically ill, so the staff outlined a plan for repositioning. They frequently checked for sign of skin breakdown, they have a consistent core group of nurses, and consistent site care, and that team working together that patient has zero skin related issues, where a couple of years ago that patient would've likely had a pressure ulcer. The next story the patient was in the ICU for two months, there were a lot of morbidities, I cannot list them here, it the staff changed -- the staff changed every two hours, they were working together, or more often, if there were any redness, the shift reporting to address skin issues, continuity of care, that patient has zero skin related issues. The staff was of -- was very proud of the accomplishments there. That is a program in the that shall. I will stop there in see -- in a nutshell. I will stop there and see if there are any questions. Please remember to and mute your phone if you have any questions. -- un mute Your phone if you have any questions. Anybody on the phone from Hamilton? They have done very good things there. Does this sound familiar to the work you've been doing? Yes -- it is not necessary for you to put star zero you may ask your question directly. I am curious this is Julia, has anybody been working on that many chefs less than 30° more often? That is something I initially had pushed back on, it is gaining more acceptance here, that data is very compelling, -- working on the shifts less than 30°. When you're looking up the pressure Paul Ohm's -- pressure problems, did you consider that part of the oh are when you looked at them? We focused in all areas, that work was primarily in the ORs. I think one of the most helpful things that OR has put in place is the communication between the preop, and the PACKU. They were developing in pressure ulcers, each teams communicate to the next stage of care what position the patient was in, so that they could read position them even in PACKU. Those were the type of things they were working on. This is Patty from University Hospital. Do you use cycle prevented if for the oh are -OR, before they go? I would love to hear more about that. We have had very great results with that, we have been using that since many. -- May. We have specific criteria for that we are now fixing to go how wide with that, I was just curious if that was part of you all? Before they go to the OR, we see a dressing on the loved ones cycle area so that they know that they do not have a pressure sore it is just prevented if, it is peeled back every day, changed three days, they just kill it back and replace it -- they just replace it, they pull it back and change it every three days. I have not heard about that I will go back and asked them, thank you. Patty, what product are you using as they prevented if? Is it [Indiscernible] That is the one we used, we tried, text -- we tried Commatext, it was thicker with the silicon foam, it was superb results with that. We are getting ready to trial that, we are getting ready to use another product, not getting great results, we are going to trial that when. What was that? We are getting ready to trial that Monolic product. -Before going into all are, -- OR there was war criteria placed on it, and I was going to say what the for work, they had surgery greater than four hours, the patient was in position, or if they were already in the hospital of course, we know those surgeries that last more than four hours, those automatically were placed on it. Then we did have units in the OR, take it off before the floor, it didn't make sense since we were having such great results, we are just now fixing to go house wide with it. I'm sorry what were the for criteria of? -- Criteria? We have a list of 20, five of more of the following, surgery greater than four hours, if surgery is information, three or more, or code call, or greater pressures than 24 hours, or greater criteria of five or more conditions. Now that we are going house wide we have changed it to five or more. Is there anyway we can get that? We tried cut -- it in ICU, we were putting it on everybody if they did not have a break down, I would love to see how you trialed it. We actually use that house wide now the same product, we see a similar thing, we had criteria for those patients if they meet one criteria, they automatically get in place, we do not use it currently in OR, we trial date in ICU, -- trial it in ICU, the other woman Patty I believe, said that they a trialed other products, we've been tried a Medline product, doesn't stay as well. Also I'd like to throw in there, the one thing we noticed is silicone dressing will rollup somewhat under the patient, if they are moving them around, the way that the process in our minds is, I would mind this -- I would rather the dressing take it then the patient's skin. If you try the monolith that -- if you try this product it did not rollup. I agree they did not stick as well this product does stick well. It is much better, I agree it does rollup a little bit. You're right if it is going to rollup you'd rather that then the friction on the skin. Absolutely. We already currently use it house wide, I am pretty impressed with the fact that you have your door in the or -- in the OR how did you overcome the hurdles? And educating the staff about that? We did not have hurdles at all, I've been doing healthcare for 20 years I have worked closely with the director of OR, anytime we do have a stage II, we have been doing quarterly studies, anytime we have had a pressure ulcer develop, or any type of pressure ulcer, usually we have caught them, we have a tracking tool, at that time we do a drill down, anytime we have a pressure ulcer, and have they been in the ORs, how long, that is one thing we identified. That was one of the things I was able to work with. That is something that moved smoothly. I have a question to the gentleman using a in the are, are you using you as well as when it is prone on their chest or on their chins. We implemented it house wide -We implemented it house wide, we have not gotten it in the oh are yet. That is one thing I was interested in, we wanted to do that. If they are going to have a case longer than four hours or more in the position. This is Julie, we have the same problem, trying to get the foot in the door, and bringing data back, and also sharing stories with them, that was really effective we have just started a pilot program, on our ortho for -- you can actually put a wound or air pressure ulcer with a story behind it and let them know what the patient went through as a result ultimately not taking care of them like we should have that hits home. I hope they take it personally, that is our job to make sure that they leave here in better shape than when they came. I agree. Sometimes it does not mean as much. Absolutely. We are coming to the end of our time here, I appreciate Julie all the work you did and being able to share with us. For you guys on the call, and people in your area, the toolkit, the roadmap was part of the attachment, if you have any questions, we are posting a link to it on my website as well. When you close out the webinar there will be a pop up. There will be a new thing that will take you to a meaning in valuation -evaluation. If you are on call three would start that 1145, you can hang up and dial back in, it is a different part of the webinar. You have a link for that. Any concerns before we and the call? Tracy I apologize this is the operator. They will not have to hang up and dial back in. I can transfer them right into the co-heart meeting. Thank you. Just a closing comment whatever tools we are happy to share I would love to get my wound care together with yours, we are happy to share. This is Patty from university I would be happy to share that cycle. My e-mail should be I could share with anybody. I will get with you and also get with Michael, to send me what you have and I will share with the people on the call and posted on the website. Thank you. We are ended the call now thank you for your call, look for to talking to you, and hearing what you do with the presser -- pressure ulcers and implement roadmap if you decide to do so. Thank you.