An exploration of the process of pressure ulcer prevention
advertisement

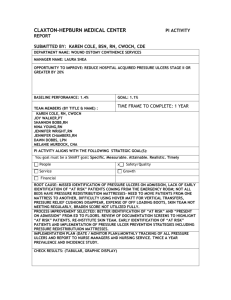
1 An exploration of the process of pressure ulcer prevention and management in acute and community NHS Trusts in order to understand contextual issues which promote or inhibit adherence to national guidelines and Trust policies. BACKGROUND Much of the published research about pressure ulcers has to do with understanding how pressure ulcers occur and so look at interventions such as special mattresses and frequent repositioning of patients to minimise the occurrence1,2. Qualitative research has explored what it is like for patients to live with pressure ulcers and for carers caring for people with pressure ulcers3. The National Institute for Clinical Excellence4 provide best practice guidance on the prevention and treatment of pressure ulcers. The information should be the underpinning for good clinical practice. There is local monitoring of the number of pressure ulcers occurring in NHS and private organisations and also National monitoring that is reported through Commissioning for quality and innovation5 2013/14 and 14/15. So there is published research on the causes and prevention of pressure ulcers as well as the incidence and prevalence of them. There are financial rewards for NHS providers by linking a proportion of their income to the achievement of quality improvement goals4. The goal is to provide harm free care. The NHS safety Thermometer is a tool developed by4 to track four quality improvements, one of which is to track the number of pressure ulcers occurring in an organisation. The request is to record the number of pressure ulcers at a given point in time, (point prevalence), currently once a month. The idea is to show an improvement in the prevalence of pressure ulcers occurring at each grade. If this improvement does not happen then the organisation will have contract funding withheld at source4. Some organisations also collect incidence data which shows how many ulcers occur based on how many people are in beds on a daily basis. This means that there is a plethora of data about the numbers of ulcers occurring but we might question what is being learnt to reduce the numbers. 2 It is plausible to claim that the rationale behind providing harm free care is essential to providing good care. However realising a reduction in the prevalence of ulcers across the grades might not be so achievable. It could be argued that different targets should be awarded to each grade, depending on the results in each organisation and even in each clinical setting. To add meaning to the data collected each clinical area could examine the prevalence of ulcer grades’ and investigate the causes. Making changes in local practice to improve outcomes. It should be noted that twenty years ago staff caring for patients in a 20 bedded ward may have been caring for 4 highly dependent patients, with the other 16 being in various stages of rehabilitation and able to provide self-care. Together with new technologies, a reduction in staffing numbers and early discharge the likelihood is that all 20 patients are now highly dependent. This in turn puts pressure on community services to provide care for a much sicker population. This study will explore the process of pressure ulcer prevention and management in acute and community NHS Trusts within North West London in order to understand local contextual issues which promote or inhibit adherence to National guidelines and trust policies via the perceptions amongst Band 4 Health Care Assistants and Band 5 and Band 6 Registered Nurses. These are the staff that has daily contact with people at risk of pressure ulcer development. And the cross boundary scope is recommended by4. The NHS Trusts who chose to participate in the project do not currently share patient specific data for the process of learning from individual cases moving through the services. It could be argued that time spent evaluating the route cause could change prevention initiatives and improve outcomes for the future. By sharing the results with neighbouring organisations such as social care there could be an improvement made in cross boundary communications, hopefully reducing the ‘blame culture’. METHODS Design/sample 3 A qualitative study design to discover junior staff nurses and healthcare assistants’ perspectives on the management and prevention of pressure ulcers in both primary and secondary care Trusts. The recruitment process included local advertising via posters for an online survey (n=61) or interview (n=11). The sample was self-selected and there was a £30 gift voucher for the interview participants’ time and a £100 gift voucher for a randomly drawn name from the survey. The participants all had a similar context, that of managing and prevention of pressure ulcers but ranged between Acute Hospital Trusts and Primary Care Trusts. Six of the interviews were conducted at a university and five at a Trust, all in a private room and lasting up to one hour. The online survey could be accessed from computers, IPads and IPhones. Settings The study was conducted in four NHS Trusts in England UK. Two were community and two acute hospital Trusts, which were in close enough proximity for the patients to potentially move between them all. Data collection After gaining university research ethics committee approval and research and development approval from each Trust the online survey was opened and consent was presumed to have been given by completion and a participant information sheet was included at the start of the survey. The recruitment to the online survey lasted eight months. A patient information sheet was given and written consent gained from all participants interviewed. The interviews were all recorded and held between April and July 2014. The survey and questionnaire were developed via a Delphi study with senior tissue viability nurses from each of the participating Trusts. The same four open ended questions were asked in each. There were help buttons on the survey which gave prompts to the open questions and there was a list of prompts that could be potentially asked during the interview. Data analysis 4 The recordings of the interview were all transcribed verbatim and the results of the survey were printed as hard copies. The two researchers independently analysed all of the data each. One researcher did so directly from the hard copies and the other used NVivo 10 a software programme to manage the data and facilitate the coding process which was initially numbers correlating to the four questions with sub codes developing from the data. The two researchers met to discuss the initial coding and analysis and then agreed the codes into broader categories and finally agreed themes organised according to the four questions. FINDINGS Pressure ulcer prevention and management over the last eighteen to twenty four months has become a major priority for Trusts Pressure ulcers have become a high priority in healthcare politically and thus managerially. The time frame often mentioned was the last eighteen – twenty four months. But it is one thing amongst several that have such a high profile. The impression often seemed to be one of being forcefully kept as a high profile, being ‘hammered’ into staff or of staff being ‘bombarded’ with the need to prevent and manage pressure ulcers. The maintenance of the importance is being externally and forcefully imposed upon staff. It is something massively that I would say because I have been with the district nurses now 5 years and I would say over the last 2 years alone it has been hammered into us. By whom? By management… So are management banging home incontinence, nutrition and everything else or not so much? Probably mal-nutrition, nutrition not so much, but malnutrition definitely. Incontinence they do spates of it... (C.SN) Yes – it is very much drilled in - no pressure ulcers on the ward – if you get one, there are so many things that we have to do and then if it is not being done we are having another audit and we are having another – why is it not done etc. (H. SN) 5 But we are bombarded by so much all of the time one thing, I wouldn’t say gets missed,[pressure ulcers] but it’s like what is the next thing, and next thing, so there is always something that we have got to deal with, a course to go on and something (C.SN) There is an implication of staff being told to keep a high profile for certain aspects of care and that they seem to come in phases and staff feel they are running to stand still. I often say this job is like spinning plates, so you get that one going and then you have got to do that, and just keep coming back and forward,… (C. SN) However many participants suggest that there is also an internal perspective to the management and prevention of pressure ulcers. That it has always been a priority for nursing. The ‘big fuss’ mentioned below was made by ward managers [senior nurses] grounded in the idea of good nursing care and prevention of harm to the patients. No cos ever since I can remember, since I have done my training, [much more than 2 years ago] it has always been a big deal, a big fuss (H. SN) We thought that other things about incontinence and other issues, and with dementia these days as well. How much of a priority is pressure ulcers do you think. Very much so, because if they don’t know that they have got a pressure area, it could turn out to a grade 4 and then we are years getting it back to normal. And its comfort for them, quality of their life, it’s so demoralising for these patients, and it's more now than it ever was. (C. HCA) 6 It is a top priority for the service. There are investigations of bad cases. I know there are national initiatives and I know there is a CQUIN but really it is seeing them which motivates me. (H. SN) The imposition has perceived good effects. There is evidence that the political and managerial imposition of pressure ulcer prevention and management has resulted in improved patient outcomes of reduced incidence of pressure ulcers via more standardisation or reduced fragmentation of practice in some organisations. There has been a new protocol out now for about a year and we do check everybody that we – a new patient comes on, we are the district nurses check for them. And that is quite a recent protocol to check every patient. The last 18 months I would say, we have to ask their permission if we can have a look at their pressure areas. Some people won’t, they won’t let us look at their bits, whether we are a nurse or not. Especially if they are dressed I suppose. Yes. So it is quite a performance, but yes we are getting there with them – we have less now than we used to have. (C. HCA) Yes actually occurred. Because we are a district nurse we very rarely go in, unless we are going in to do a different kind and then we do check their pressure areas. We could be going in for about 3 weeks and not even know that the persons got a pressure area because she has not said anything. But we do check now when we go in. There has been a new protocol out now for about a year and we do check everybody that we – a new patient comes on, we are the district nurses check for them. (C. SN) 7 The reduced fragmentation was almost wholly applicable to individual NHS community Trusts. In addition the multifactorial causes of pressure ulcers has meant that a more holistic assessment of a patient’s needs is carried out. The assessment of skin for an ulcer is but one part. Yes – I think in the last year it has really changed a lot – it is more – everything seems to be covered now. And it is not so fragmented, everyone is doing the same or similar. Everybody is getting the same information with pressure sores, and everybody should be singing from the same hymn book (C. SN) Aiming for no pressure sores puts a greater emphasis on basic nursing care, including turn regimes, meeting hygiene needs and patient comfort (H. SN) Fragmentation between primary and secondary care Although there seems to be much less fragmentation of care within primary care trusts it remains a concern between primary and secondary care, though there is some indication that this is improving. The community staff felt they were a separate department whereby information about patients as well as equipment needed for continuity of care for the patient was the responsibility of just that department rather than a national service. The reasons given for the improvement is the external imposition via the high political and thus managerial profile of pressure ulcer prevention. Well because sometimes they move in-between health care providers, from the community to a hospital, things get lost along the way and people, I am not blaming anyone else, I am sure we are guilty at times as well, but we all work in groups, so as someone goes into a hospital, whatever, I am not saying anything as I used to work in a hospital, so there is that. (C. SN) 8 No they wouldn’t bring it here we would have to sort all that out when they come here because it is our department then – it’s like two separate areas – which I didn’t really realise – when you work in a hospital you are borrowing from this ward, that ward, this wards – you don’t think you just say have you got a pressure mattress – yes here is a clean one – it was very much – this is all a bit sad, we are our own very little department really. (C. SN) I think the hospitals now are much more aware of letting the districts know of the discharge of a patient with pressure ulcers or who are at risk of pressure sores – where in the past – it would be the carer that would call you and you would see this and they would have come out of hospital 2 weeks ago . So I think now again people are being made much more aware and they are. The quicker off the mark now catching things Why do you think that might be? I think because of all the publicity and everything (C. SN) But even with the optimism of advanced notice being given to primary care of patients in secondary care with pressure ulcers who are planned for discharge there is perception by some that certain equipment directly related to or made for pressure relief seem to be prioritised over other equipment essential for pressure sore healing and management. That a mattress can be relatively easily and quickly put in place but a patient who had a certain wound management piece of equipment in hospital cannot not be discharged with it to the community and the community struggles more with finding an alternative than it does so with a mattress. It is to be recognised that financial and procurement services in primary and secondary care, with care homes a separate element again are funded separately. This means equipment, dressings etc. cannot be transferred between organisations. Waiting times for resources can result in difficulties with providing best practice care or lead to delayed transfers. 9 In addition it seems that at least sometimes, in the community, there is fragmentation in knowledge of such aids. Lack of knowledge on how to use the aids they know they have access to but also lack of knowledge of what aids are accessible for them to use. So with possible plans in advance shouldn’t delay No shouldn’t delay anything – shouldn’t – but things like that [pressure relieving mattresses] are priorities – I think other things are perhaps not – maybe something like the vac pump [wound management system] – I don’t know. (C. SN) There are days that we find ourselves with gadgets and tools to manage/ avoid pressure ulcers without any trainings or teachings on how to operate them, or sometimes, we do not even know that these gadgets or tools exists because no one has ever mentioned anything about it (C. SN) The need for time There is a perception that a lack of time is now a particular barrier to quality care generally and thus has direct impact on the prevention and management of pressure ulcers but it is expressed in slightly different ways. To be honest with you, I would say it is about the time you spend with your patient. And that would mean potentially another one or two nurses just to help. Because when I first started here you were able to go in and spend time checking your patients from head to toe, now it is just come on let’s go and get on with this – you are like a blue bottle flying around. It didn’t used to be that way (C. SN) 10 We don’t have time to sit and have a cup of tea with them anymore. We don’t have time – we could be the only person they see within a week, no-one else but else, and when we come in they are so excited and or maybe they wait for us to come and make them a cup of tea (which we shouldn’t be doing) but we do, and they just want to talk for half an hour, and we are clock watching. It’s unfair that we should have to do things like this. (C. HCA) Relatedly the idea of time management was discussed as a type of characteristic, personal or professional is not clear, that could impinge adversely on the management and prevention of pressure ulcers. I don’t think it will ever be achievable because everybody works differently; everybody has got different goals when they come to work and care for patients. Some people are more like time management oriented no matter what is going on with the patient; they just want to get everything done on time. That might mean not rolling your patient a lot, you know, doing the necessary things to care for your patient. Do you think the people that focus on time management then, just – so it wouldn’t just be pressure ulcers – they just focus on getting anything done on time? Yes I think so, that is certainly in intensive care that can be a problem. You are just so pushed for time, getting everything done on time - going for your break on time – making sure and helping others, and you want to go home on time. It’s just all of that will impact on things like pressure ulcer care. (H. SN) And the issue of time arose for some in that more patients require a greater number of staff to facilitate care in general so including pressure ulcer prevention or management which takes planning and time to manage. ……Though it might be another matter with morbidly obese patients who are bed bound. We had to care for a male patient weighing more than 400 kg before it would take literally the whole unit to be there to give him a wash!(H. SN) 11 The importance of education There was a great emphasis on the need for or importance of education in the prevention and management of pressure ulcers ranging from education for staff nurses to healthcare assistants and carers who may be relatives and patients. Lack of education particularly for carers and relatives was a common reason given for not being able to prevent some pressure ulcers from occurring. NICE4 emphasise the importance of offering advice to people at risk of developing a pressure ulcer, their family and carers. It is to be noted Health Education North West London have funded an App ‘Preventing Pressure Ulcers’ available to all four Trusts, to enable staff to provide the education. , so one reason you think that they cant be prevented is other people care for the patient, i.e., relatives, other than yourself. Yes, who don’t understand pressure area care. Why would you – they are not trained to look for, maybe carers could be a bit more informed maybe on signs and symptoms and how they could help – if they are going in daily, and to know what to look for. It isn’t rocket science. It can be in the initial stages, because you might think it’s just a little bit red, bit sore and then the next thing, it’s gone. So, I think carers and relatives maybe when we are not in there, if there was a bit more information maybe. (C. HCA) Carers come in, wipe their bottoms. The carers and the district nurses do not communicate. That is the worst bit. So the carers come in they get a bit of sudocream and they have got a whole handful and they slap it on and it is everywhere. Cream doesn’t work with a pad and it don’t matter how many times you tell the carers they are still doing it. We have big notices up please do not cream this patient and you’re back in and there is another load of cream on them…(C. SN) 12 So I sat down with the senior carer there, explained it to her, this is why we want this to happen, going down to the nitty gritty saying that if a patient is on one side for so long it increases pressure there but then back again so those simple aspects of describing what we want to happen and what happens to the patient, I think made that situation a bit better and compliance now is actually 100% from the carers, but previously before it was no we don’t want to do this and why do we need to. I don’t think anybody ever answered those questions before. (C. SN) The need for the education of health care assistants was a recurring theme in the data from staff nurses. And one health care assistants in secondary care would like to take on a sort of pressure ulcer champion in his areas of practice to both help the ‘busy’ staff nurses and improve the quality of care for patients. The healthcare assistant recognised the need to report concerns to the registered nurse. I think this is an achievable idea, however if only more training is provided to all healthcare staff not just nurses. More training should be provided to HCA's and Student Nurses (H. SN) I was working with a HCA who passed some of her pressure ulcer competencies and yet didn’t reposition an at risk patient for six hours the exact same day which. Education needs to emphasise the importance of repositioning. (H. SN) I think, I know I shouldn’t do it, but as HCAs sometimes we should develop ourselves by giving ourselves extra responsibilities, so for example if I was on the first floor I would be the HCA wound care and pressure sore manager if you look. Not that I want a title, but give it to somebody that feels like they are always busy to do stuff, and want to do stuff, give them something to do, give them that responsibility and say by the way you are going to be in charge of pressure ulcers, when you are off the HCA who is in charge, you will pass this 13 information on to him/her that you must check all patients and give them that responsibility. It is not, they are not doing anything out of their job scale…(H. HCA) Audits of pressure ulcer management were often being done by very senior nurses. And the need for education amongst all staff, including staff nurses of band 6 was highlighted. …– she said it is not just me – but everybody needs to make this a point of getting this done, but also people are not documenting properly. They were putting things like 100% granulation for unstageable pressure ulcer or a grade 4 pressure ulcer which obviously doesn’t make sense at all. (H. SN) And patients attending a clinic in primary care received information about pressure ulcers whether at risk or not. This was how the protocol was being interpreted. We try - if we have got enough time we sit down and try and explain it to them, what causes it, how you can prevent it, we actually give everybody an ulcer prevention form which we have got in the clinic which we give to every single patient that’s new or comes on. Even if they are capable we give them it because that is what we have to do – its protocol. (C. SN) Perceptions as to why some pressure ulcers will occur Aiming for zero pressure ulcers is not realistic. This is especially so because of reactionary care in the community and due to underlying co morbidities and nutrition. It may be more acceptable to be specific about which grades to reduce. …it is easy to set such a high standard for others, especially when it is not yourself that has to implement this strategy. I should imagine it to be near impossible to prevent all pressure ulcers in patients receiving care. I think striving for 0 pressure ulcers is a nice target but when people working in care are aware that this in unattainable it may not be as appealing to strive to meet this target. Also with the variety of different grades of pressure ulcers I 14 think that statement needs to be more specific in order to elucidate what is fully meant. (C. HCA) There are patients within our unit for whom it is extremely difficult to prevent developing a single grade one pressure ulcer or worse. These may be patients who are grossly oedematousparticularly infants, those who are so unstable that they do not tolerate repositioning without having a deterioration in their respiratory or cardiovascular status…(H. SN) There was a notable number of primary care responses that focussed on the issue of patient concordance or the lack of such. And some suggest that patients who do not develop pressure ulcers take more pride in themselves than ones who do, evidenced by walking around rather than ‘just’ sitting in chairs. Right the ones who got pressure ulcers have either refused to have the seats, cushions, the beds any equipment that we have tried to put in their they have refused it or they have got it and they are using it wrong or they have go it and it is sitting in a corner. We have go quite a few patients that you see, you have ordered them a lovely cushion to sit on and its over there in the corner because it’s too high for the chair. It don’t matter what you say. Or the worst ones are you get a cushion and they put two towels on it and they are sitting on the towels which then rucks up and gives them a bed sore or a chair sore and it don’t matter what you say to them it’s too cold to sit on. (C. SN) Cos they do as they are told or they take more pride in themselves. They walk around a little bit. Most people with pressure sores are people stuck in a chair all day. (C. SN) 15 The difficulties of knowing which pressure ulcers are preventable is compounded by the fact that it now becomes a potential safeguarding issue for patients presenting with pressure ulcers with the involvement of social workers. …and I was speaking to a social worker and she was saying to me is this preventable or not and in one sense it could have been for her. The reason being she is attending a chemo suite as an in-patient originally and as an outpatient. So potentially along those lines it could have been spotted. (C. SN) DISCUSSION The findings from this study reveal that band 4 healthcare assistants and bands 5 and 6 staff nurses feel that national guidance and local policies in the prevention of pressure ulcers have over the last eighteen months or so a major priority that are externally imposed by Trusts and managers and thus, ultimately, senior nursing staff and that overall it seems to be a good thing in practice at least in the sense that the perception is that the incidence and prevalence seems to be reducing. And at least for primary care, a more standardised and less fragmented approach but this may reflect the fact that secondary care generally may have a more standardised approach and so was not mentioned explicitly as a reason for improved management of pressure ulcers. It could be suggested that financial rewards for NHS providers drives initiatives for change, that the external imposition of CQUIN Safety Thermometer and the need to show a reduction in the prevalence of pressure ulcers has focused executive boards to insist on improvements in care. Staff agree that pressure ulcer prevention is an important aspect of care. However they do not seem to be aware of the rationale behind the current push to improve. It could be argued that with all the pressures on staff to provide the many elements of care, explaining the political agenda and financial implications might provide staff with a forum to discuss how this can be achieved. This may assist staff to feel included in the decision making and improve morale. 16 Though it was very clear that staff are feeling bombarded by external change and protocols what did not come out from this study in any strong form was any indication that they saw this as a failing on the part of nursing; that the presumed need for such top down imposition reflected poorly on nursing. However the ‘fuss’ being made now about pressure ulcer management and especially prevention has facilitated essential nursing care in the many related aspects that can all play a potential part on pressure ulcer development though each aspect seems on its own to have been driven by the same political and thus managerial drive. There is the impression that such imposition comes in waves and about different aspects of nursing care such as malnutrition, incontinence and infection prevention and control. But again, the reason behind the need for such imposition and its reflection on nursing as a profession was not explicitly addressed by participants in this study. As well as the external imposition there was some evidence of an internal perspective on the need for prevention of pressure ulcers. This could be as a profession or as an individual nurse and perhaps even as a person. The idea of a distinct role from the person seems to be blurred when it comes to wanting to prevent pressure ulcers, especially in relation to harm. Frequently it was the sight of grade three and four pressure ulcers that motivated staff to focus on pressure ulcer prevention and management. But it was healthcare assistants who seemed to see things explicitly from the patient perspective, the staff nurse whose comment reflected concern for patients’ dignity had recently qualified after being a healthcare assistant for many years. Staff nurses seemed to focus explicitly on meeting protocols and recommendations4, 5. It is not clear from the participants’ responses if there is an understanding of what the initiative4 is trying to achieve. The sharing of information between the executive and the nurses at the bed side seems to be lost in translation somewhere within middle management. The nurses saw preventative care as essential in the sense that harm free care is a given but that the pressure put upon them to provide the care was not necessarily realistic due to so many other priorities. It could be suggested that the nurses providing the care are not valued or listened to 17 as good care is rarely praised. If a change in practice is required the information may not be relayed with a positive attitude. Though a lack of time was an underlying theme in this study, it is unclear if there is a lack of time to carry out the skilled task of physical assessment which as well as for pressure ulcer risk included many other assessments from ‘head to toe’ or whether it was a lack of time to enable the nurse or healthcare assistant to do these assessments well, where well is to be understood as including time for social interaction, to listen and chat with the patient. In this study the idea of sitting and chatting as social interaction and that the lack of it was an injustice was voiced by healthcare assistants. But also the need for time for social interaction can be pragmatic in order to gain trust and concordance by the patient to allow further care and assessment to progress. In primary care nurses are entering patients’ homes as a guest. Without time to gain their trust patients can rightly refuse care. This will reflect negatively on the team trying to provide the care if a pressure ulcer occurs. Plus an additional increased cost of treatment. Suggestions that Trusts should not be seeing pressure ulcers occur was thought to be a nice ideal to strive towards though in reality unachievable, even in areas of 1-1 care such as ITU. This raises a need to base staff numbers on a shift based on patients’ needs rather than on patient numbers. It was also thought that by setting such an ideal it may make it less appealing for practitioners to try and reach. Rather than such an ideal, it may be that stipulating which grade of pressure ulcer is to be fully preventable may be better. There has been a shift in some areas of making a clinical incident of all pressure ulcers of grade two and above instead of a grade three adding to the concerns of the unrealistic aim. However it can be suggested that by focusing on ways to reduce the number of grades1 and 2 ulcers there will be a natural reduction in grades 3 and 4 ulcers as a result. 18 Detection of pressure ulcers in certain patients has become an issue of safeguarding. And nurses are being asked by social workers whether the pressure ulcer was preventable. This in itself is a more difficult question to answer than it seems, with nurses having to make inferences (or speculations) about for example patients having been an inpatient or attending clinics as well as multifactorial risk factors. From this it can be suggested that the ‘blame culture’ influences responses as no clinical area wants the ulcer to be attributed to their care. Nurses report only negative feedback when reporting any grade of ulcer, even if the ulcer was not preventable. NICE4 discuss incidences where patients’ physiological resources may be lacking so prevention or even healing of an ulcer may not be an option. This maybe the agreed outcome from an analysis of the finding but in the interim period nurses may feel they are the target for providing poor care which may influence morale and team working. There is still a lack of training in the prevention and management of pressure ulcers particularly for patients looked after at home, resulting in reactionary care, after the ulcer has developed. The need for the education of patients and carers was a relatively strong theme in the findings of this study at least from a primary care perspective where the carers and patients do not see healthcare professionals much of the time during which a pressure ulcer could develop, there was less emphasis within secondary care. The education seems to be required to explain the potential risks to patients who are labelled as non-compliant or non-concordant, perhaps this is for their benefit but also to cover professional, policies and legal duties of care. The education is required in addition for carers regarding specific tasks that seem to being carried out incorrectly. In secondary care the need for education of healthcare assistants was a theme within the staff nurses interviewed and weakly it was suggested that all staff need education in wound care generally and specifically pressure ulcer management. The impression from the data is that patients attending outpatient clinics were given information in the form of leaflets on pressure ulcers whether they were at risk or not because it was understood as being policy to do so. 19 There was a very heavy reliance on the tissue viability nurses to provide education to staff much of it seemed to be about fundamental wound care issues that could lead one to question whether a reasonable standard of care was being met. There was weak evidence to suggest that ‘apps’ for education on mobile telephones would not be useful, though posters were referred to in order to guide dressing options. NURSING IMPLICATIONS The results of this study suggest a number of actions that nurses and managers can use to improve the management and prevention of pressure ulcers. First, the political and managerial input needs to be internalised by nurses so that the care continues long after the political priority has abated. Nurses need to stop the waves of political and thus managerial imposition of aspects of nursing care and take control of what they do, which may mean being more involved at getting their needs and concerns across at executive level to address the causes of the problems. The strong focus on the management and prevention of pressure ulcers needs to recognise the inevitability of some pressure ulcers occurring. And that numbers of patients alone may not be a good indicator of staffing levels especially where patients need frequent turns. But it is of note that with such a strong emphasis from senior staff managerial and nursing measurable outcomes were improved. LIMITATIONS Although this study began with four Trusts, despite frequent requests and follow-up and an extension to the time for data collection, one Trust had a zero response rate. The qualitative, open ended survey varied in the amount of response given from a couple of sentences to each of the four questions to several paragraphs of text. 20 CONCLUSION AND NEXT STEPS The findings from these interviews and survey underpin the known complexities for the prevention and management of pressure ulcers. It gives an up to date account of perceived improvements in care both within and between different Trusts. REFERENCES 1.Coleman, S; Gorecki, C; Nelson, A; Closs, J; Defloor, T; Halfens, R; Farrin, A; Brown, J; Schoonhoven, L; Nixon, J. Patient risk factors for pressure ulcer development: systematic review. International Journal of Nursing Studies. 2013; 50: pp. 974-1003. 2.Soban, L; Hempel, S; Munjas, B; Miles, J; Rubenstein, L. Preventing pressure ulcers in hospitals: a systematic review of nurse focused quality improvement interventions. The Joint Commission Journal on Quality and Patient Safety. 2011; Vol. 37, No. 6: pp. 245-252 3.Fox, C. Living with a pressure ulcer: a descriptive study of patients’ experiences. British Journal of Community Nursing. 2002; Vol., 7 (Supplement 1): pp. 10-22. 4. National Institute of Clinical Excellence. Pressure ulcers: prevention and management of pressure ulcers [CG179]. 2014; http://www.nice.org.uk/guidance/CG179 5.Institute for Innovation and Improvement. Delivering the NHS Safety Thermometer CQUIN 2013/14 NHS Institute for Innovation and Improvement. 2013; http://harmfreecare.org/wpcontent/uploads/2012/06/NHS-ST-CQUIN-2012.pdf