Chapter 14: Psychological Diagnosis and Disorders
advertisement
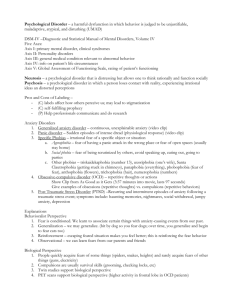
Chapter 14: Psychological Diagnosis and Disorders Rob Cramer, M.A. Department of Psychology & Psychology TraineeThe Counseling Center Psychological Diagnosis and The Medical Model –Medical Model categorizes behavior as abnormal –What is abnormal? (3 criteria) • Deviant • Maladaptive • Causing personal distress –Behavioral continuum from abnormal-normal • Diagnostic Schemes: The Diagnostic and Statistical Manual – Current version is DSM-IV-TR – 1980: DSM-III added multi-axial assessment scheme Axis I: Clinical Syndromes Axis II: Personality Disorders and Mental Retardation Axis III: General Medical Conditions Axis IV: Psychosocial and Environmental Problems Axis V: Global Assessment of Functioning • What do you think about diagnosis? – Do disorders exist? – Stigma? “She’s depressed” “He’s on medication” “He was hospitalized for schizophrenia” What comes to your mind? • Anxiety Disorders – Generalized anxiety disorder – Phobic disorder – Social Phobia – Panic disorder and agoraphobia – Obsessive compulsive disorder – Post-Traumatic Stress Disorder Causes of Anxiety Disorders • Biological factors – Genetic predisposition, anxiety sensitivity – GABA circuits in the brain • Conditioning and learning – Acquired through classical conditioning or observational learning – Maintained through operant conditioning • Cognitive factors – Judgments of perceived threat • Personality – Neuroticism • Stress – A precipitator • Example of Maintenance of Anxiety: Phobia Activity Time!!! • The good doctor is still locked away!! Help his patients out by identifying the type of anxiety they have. Case 1 • Johnny is a 20-year-old college student who has had recent problems with grades and friends. He has reported feeling nervous and fearful about taking exams, making his friends happy, and many other areas of his life. Johnny sought therapy for his problem. During early therapy sessions, Dr. Relax learned that Johnny’s symptoms began several months ago after a musical performance in which he froze and was laughed off stage. Since that time, Johnny avoids playing his guitar or going on stage. He also told Dr. Relax that his grades began to drop and friendships suffered because of trouble concentrating, trouble sleeping, and feeling tired. What type(s) of anxiety disorders does Johnny have? Case 2 • Lisa was involved in a plane crash more than six months ago. Shortly after the crash, she began having nightmares and flashbacks about the event. Since that time, Lisa has also become easily startled by any loud sound and she often wakes during the night. Lisa presented for therapy with Dr. Relax because her job requires her to fly to a conference in Florida next week, but she is experiencing tremendous anxiety and trying to avoid having to fly. What type(s) of anxiety disorders does Lisa have? • Depression and Suicide • What do you know? • What do you want to know? Depression Facts 1. 3rd most common disorder 2. 1 in 5 people will suffer an MDD episode across the lifetime 3. Almost twice as common in women 4. Costs businesses an estimated $33 billion in salary productivity per year 5. Most common in young adults and older adults 6. Expressed differently by culture and age • E.g., Chinese – somatic complaints • E.g, Children – anger/irritability Major Depressive Disorder Two weeks of 5 or more of the following: 1. Depressed mood and/or 2. Loss of interest 3. Weight loss or gain 4. Insomnia or hypersomnia 5. Psychomotor agitation or retardation (e.g., restless) 6. Loss of energy 7. Worthlessness/guilt 8. Concentration/indecision 9. Recurrent thoughts of death Dysthymia Two or more of the following are present or at least 2 years: 1. Poor appetite or overeating 2. Insomnia or hypersomnia 3. Low energy 4. Low Self-esteem 5. Poor concentration/indecision 6. Feelings of hopelessness - MDD episode cannot be present in these 2 years Differences between MDD and Dysthymia 1. Intensity 2. Time requirements 3. Symptom presentation • • • Thoughts of death Weight issues psychomotor effects 4. Presentation for treatment • MDD more likely Factors Associated with Depression 1. Cognitive Styles • • • Locus of Control Learned Helplessness Hopelessness Theory 2. Stress • • Chronic stress Major life events – can precipitate both types 3. Personality • Five-Factor- associations 4. Biological underpinnings • Neurotransmitter dysfunction Treatments: 1. Cognitive/Cognitive-behavioral Therapy • • Belief testing Thought Record 2. Dynamic Therapy • • Bibliotherapy Assertiveness training 3. Psychopharmacological Therapies • SSRIs Warning signs • • • • 1. Changes in activity level 2. Physical changes (e.g., weight) 3. Emotional pain 4. Mood change (e.g., irritable, down, selfcritical) • 5. Changes in thought patterns (concentration, decision making) • 6. Thoughts/mention of death Scenario: Fred is your roommate. Lately, he has been sleeping a lot more, feeling down, and pulling away from others. He makes statements like “it would be better if I wasn’t here” and “I don’t care about anything anymore.” 1. What is wrong with Fred? 2. How would you handle this situation? 3. What if he has a plan? Suicide Facts 1. 8th leading cause of death overall, 3rd for adolescents and young adults 2. Most prevalent in adolescents and older adults 3. Twice as common in college students than non-college counterparts 4. Accounts for 30,000 deaths annually 5. Women more likely to attempt, men more likely to complete 6. Suicidal thoughts and attempts difficult to count Associated Risk Factors/Causes • • • • • • • • 1. Mood disorder 2. Gender 3. Negative Life Event 4. Neuroticism 5. Low self-esteem 6. Low social support 7. Personality Disorder **Most likely completed when mood is improving Warning Signs 1. Talking about dying 2. Recent loss 3. Depressive symptoms 4. Talking about loss of control/harming self or others 5. Withdrawal from relationships 6. Hopelessness 7. Previous attempt** 8. “Finalizing behavior” (e.g., Giving things away, tying up relationships, making out wills) Suicide Assessment • Question: Imminent risk of death vs. non-fatal attempts? • 1. Allow person to discuss their problem for 5-10 minutes • 2. Assess negative psychological effects of problem (e.g., hopeless, depressed) • 3. Assess thoughts of suicide uninterrupted thoughts at the moment, plan, means • 4. Assess thoughts of death- active or passive? • 5. Ask about carrying out plan/taking other with them What should you do to help? • • • • 1. Educate yourself on warning signs 2. Be direct 3. NEVER leave the person alone 4. Assess immediacy of threat – plan and means? Remove if needed • 5. GET HELP!!! – University Counseling Center • 348-3863 – University Psychological Clinic • 348-5000 – 1-800-SUICIDE – 1-800-273-TALK – DIAL 911 A helping hand for Fred… Recall that Fred has exhibited depressive symptoms and talked about death. How might you go about helping him? I need a volunteer for a role play!!!





![This article was downloaded by:[University of Pittsburgh] On: 6 August 2007](http://s2.studylib.net/store/data/012007452_1-a2e31ba32f7cff00511d31912057db37-300x300.png)