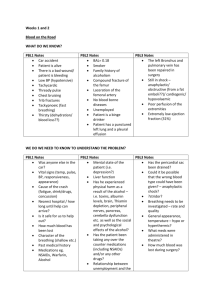
VITAL SIGNS
advertisement

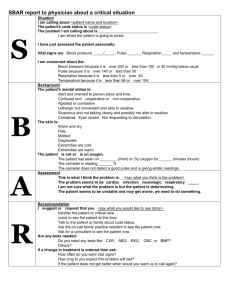
VITAL SIGNS THESE ARE SIGNS USED BY NURSES, PARAMEDICS AND PHYSICIANS to follow-up the patient's condition or to detect any variation in them. The vital signs include: Pulse Respiration Temperature Blood pressure Pupils Colors Level of consciousness Stroke pain Ability to move PULSE Reflects the rate of the heart beat Felt where an artery passes over a bone near the surface (superficial) of the body. Normal heart rate ranges between 60-90/min RESPIRATION It is the means by which oxygen enters the blood through the lungs during breathing in and carbon dioxide is expelled during breathing out. Normal respiratory rate is 12-16/min TEMPERATURE Average body temp is 37 degrees centigrade Take by a clinical thermometer BLOOD PRESSURE It means the force required by the heart to pump blood from the ventricles of the heart into the arteries. It is measured in systolic and diastolic pressure. Systolic- is known as the force to pump blood out of the heart Diastolic- is known as the resting period when the pressure falls, also known as the relaxation period of the heart pump Normal B.P. 120/80 or 100/70 mm/Hg Hypertension: High blood pressure Hypotension : Low blood pressure PUPILS Check the pupils for size, equality and reactivity Examine both eyes COLOUR Color of the skin and mucous membrane, (conjunctiva, inside of the lips) LEVEL OF CONSCIOUSNESS This is used during cardiac arrest, head injuries and any comatose patient to assess responsiveness REACTION TO PAIN in case of cardiac arrest, response to painful stimuli can be tested a pin or sharper object can be used in assessing reaction to pain ABILITY TO MOVE If the patient is conscious and if spinal or neck injury is suspected assess the patient's ability to move his upper and lower extremities. PATIENT ASSESSMENT Assessment is the cornerstone of excellent patient care. The first goal in assessment is to find out the patient's condition. Next, all life-threatening conditions must rapidly be found and urgent intervention and resuscitation must be initiated. Finally, all conditions needing attention prior to moving the patient must be done quickly and efficiently. Scene assessment Look for, identify, or remove any life-threatening hazards if possible so as to avoid any injury to the rescuers and any further injury to the injured. Failure to perform preliminary action may put your life at risk as well as that of your patient. Aspects of Scene Survey: Before you approach the victim: Assess the scene for hazards. "Is it safe to approach the victim?" Note the mechanism of injury Note the number of victims Note special equipment needed "Do you need additional help?" The field of examination consists of: Primary Survey Secondary Survey PRIMARY SURVEY Is a process carried out to detect life-threatening problems This exam should not take over 2 minutes. The emphasis here is on rapid evaluation and movement to the hospital with critical patients. The five types of the primary survey are: Airway and cervical Spine Control Breathing Circulation (Check pulse) and Hemorrhage Control Disability (Neurological Examination) -see if the patient is alert, responds to verbal stimulus, responds to painful stimulus and unresponsive Expose and Examine SECONDARY SURVEY OBJECTIVE: To discover medical and injury-related problems that do not pose an immediate threat to survival but may if allowed to go untreated. Assessment: The secondary assessment is a head-to-toe evaluation of the patient. All related and significant injuries and identified in correlation with the physical findings. This is accomplished on a region-by-region basis beginning with the extremities concluding with the neurological examination EXAMINATION OF THE HEAD AND NECK IN TRAUMA PATIENTS SCALP Check for lacerations and contusions, Is there blood in the hair? Do not move the patient's head during this procedure Check back of the head for blood SKULL Palpate for tenderness or depression Pay attention to the area over the MASTOID BONE for fracture EAR/NOSE Check for discharge of fluids or blood Clear fluid (CSF) from the nose or ears indicative of skull fracture EYES Check for trauma or swelling about the orbit Ecchymoses around the eyes(coon's eyes) without evidence of direct injury are a clue to skull fracture SCLERAE Check for icterus (yellowish discoloration) PUPLIS Note size and shape Equal or unequal Reaction to light? Observe motion of the eyes NECK In the trauma patient, gently palpate the back of the neck for tenderness. If spinal injury is strongly suspected, immobilization of the neck (spine) should precede all other maneuvers of the secondary survey. TRACHEA Inspect and palpate to determine whether it is in the midline The trachea will deviate an obstructed bronchus from a simple pneumothorax The trachea will deviate away from pneumothorax or significant hemothorax a tension CHEST Check and inspect for minor deformities Observe movement check for Contusions and Abrasions Palpate chest cage Feel each rib and the clavicles individually Evaluation of internal structures is best done with the use of a stethoscope. ABDOMEN Look for signs of blunt or penetrating trauma Feel for tenderness If the abdomen is painful to gentle pressure…internal bleeding EXTREMITIES Examination of the extremities should begin with clavicle (collar bone) or pelvis and proceed to the most distal portion of that extremity Each bone should be individually evaluated visually for deformation and surrounding hematoma or ecchymosis X-ray examination …….for fracture NEUROLOGICAL EXAM: Pupil response: Are they equal or unequal? Eye opening: What stimuli are required to make the patient open his eyes? Vocal? Tactile? Pain? Verbal response: Does the patient talk? Speech is the highest brain function Incomprehensible speech or an inability to speak are indications of brain dysfunction Motor response: Extremity responses to stimulation can indicate a number of things about the brain function. These responses are either purposeful or not. Purposeful responses include obeying commands CARE OF UNCONSCIOUS PATIENTS CONSCIOUSNESS: Implies awareness and attention to one's surroundings and to oneself. Consciousness is maintained by impulses mediated via Grey Matter in the Reticular Activating System (R.A.S.) Sleep is a physiological process which is usually accompanied by reduction of impulses in the R.A.S. The individual is easily arousable from sleep and basic protective reflexes are also intact. UNCONSCIOUSNESS Unconsciousness is different from normal sleep in that unconscious subjects are not usually arousable and quite often, there is loss of or interference with basic protective reflexes such as: Maintenance of free airway Coughing and swallowing Withdrawal from noxious stimuli etc. Unconsciousness may be: Partial (semi-coma or stupor) Complete (deep coma) Accurate diagnosis of the cause of Unconsciousness is important for SPECIFIC TREATMENT but for the GENERAL CARE of the patient, level of consciousness is more important. CAUSES OF UNCONSCIOUSNESS INCLUDE: SHOCK ASPHYXIA POISONING HEAD INJURY CEREBRO-VASCULAR ACCIDENTS (STROKE) EPILEPSY HYSTERIA INFANTILE CONVULSIONS HYPOTHERMIA OR HYPERTHERMIA DIABETES MELLITUS – HYPO/HYPER FAINTING/SYNCOPE, VASOVAGAL ATTACKS HEART ATTACKS OTHERS E.G. - MENINGO ENCEPHALITIS - FLUIDS AND ELECTROLYTE DISORDERS CARE Emergency care or first aid Long term care-usually as inpatient 1- EMERGENCY CARE General rules Remove the casualty from any obvious hazard and call for help. Be aware that injury to the spine may be present. Check the breathing and remove any airway obstruction caused by flaccid tongue, food particles, blood clots, denture etc. If subject is not breathing or breathing is inadequate, commence artificial respiration immediately. This is easier with the patient in supine position. Next, check the pulse and out external chest compression if there is no pulse. In the absence of both pulse and breathing, carry out the sequence of onerescuer CPR until help arrives. If both breathing and pulse are present, loosen all tight clothing, and treat any obvious life threatening injury such as profuse bleeding. Give oxygen by mask if available and elevate the legs if the pulse is feeble or fast. Place and support the casualty in the semi-prone or "tonsil" position. Do not leave the patient unattended unless absolutely necessary and constantly watch the breathing and check the pulse. Do not administer any oral fluids or food to an unconscious subject. Keep warm with blanket if necessary but do not apply heat. Remove the subject to medical aid (hospital) as soon as possible and preferable on a stretcher. 2- LONG TERM CARE In order to optimize the care of the unconscious patient in a hospital, it will be helpful to know the cause of the unconsciousness. This will involve the usual steps of history taking, examination, investigations etc. General care is however necessary, no matter the cause of consciousness is important in determining the extent of care required and may involve doctors, nurses, physiotherapists, nutritionists etc. It may also require an intensive care unit.