PowerLecture: Chapter 11
advertisement

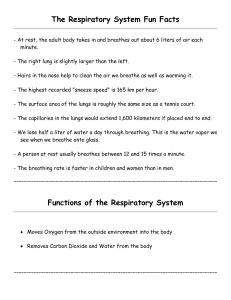
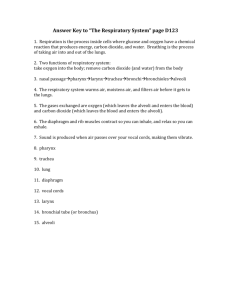
PowerLecture: Chapter 11 The Respiratory System Learning Objectives Understand how body processes generate a need to acquire oxygen and dispose of carbon dioxide. Describe the gradients that the respiratory gases follow in their routes into and out of the body. Understand how the human respiratory system functions and how it works in coordination with other systems of the body. Learning Objectives (cont’d) Explain the controls over the breathing processes. List some of the things that can go wrong with the respiratory system and explain the mechanisms through which the breakdown in the system occurs. Impacts/Issues Down in Smoke Down in Smoke Smoking poses a threat to human health and survival. Cilia that line the respiratory airways and normally sweep away pollutants and microbes are immobilized for hours. Smoke kills white blood cells that defend the respiratory tract. Smoking puts the body at increased risk for cancer, high blood pressure, and elevated levels of “bad” cholesterol. Down in Smoke The respiratory system functions to bring oxygen into, and carbon dioxide out of, the body. Fig. 11.14a, p. 206 How Would You Vote? To conduct an instant in-class survey using a classroom response system, access “JoinIn Clicker Content” from the PowerLecture main menu. As tobacco use by its citizens declines, should the United States encourage international efforts to reduce tobacco use? a. Yes, tobacco use is costly both in terms of personal health and societal financial burden. The United States should encourage international efforts to reduce tobacco use. b. No, the United States should not encourage international efforts to reduce tobacco use. Tobacco use, though deleterious to health, is a personal choice that individuals have a right to make on their own. Section 1 The Respiratory System— Built for Gas Exchange The Respiratory System – Built for Gas Exchange Airways are pathways for oxygen and carbon dioxide. The respiratory system brings in oxygen that each body cell requires and takes away carbon dioxide that every cell generates. Through the nasal cavities of the nose, air enters and leaves the respiratory system; the nasal cavities are separated by a septum of cartilage and bone. The Respiratory System – Built for Gas Exchange • Hair and ciliated epithelium filter dust and particles from the air. • • Blood vessels warm the air and mucus moistens it. The paranasal sinuses lie just above the cavities and are linked to them by channels. Figure 11.2 The Respiratory System – Built for Gas Exchange Air moves via this route: nasal cavities >>> pharynx >>> larynx >>> vocal cords (the gap between the cords is the glottis) >>> trachea >>> bronchi (one bronchus goes to each lung). • • The trachea leads from the larynx downward to branch into two bronchi, which are lined with cilia and mucus to trap bacteria and particles. The vocal cords at the entrance of the larynx vibrate when air passes through the glottis, allowing us to make sounds; during swallowing, the glottis is closed to prevent choking. vocal cords glottis (closed) glottis (open) epiglottis tongue’s base © 2007 Thomson Higher Education Fig. 11.3, p. 197 The Respiratory System – Built for Gas Exchange Lungs are elastic and provide a large surface area for gas exchange. Human lungs are a pair of organs housed in the rib cage above the diaphragm; the two lungs are separated by the heart. Each lung is enclosed by a pair of thin membranes called pleurae (singular: pleura); the pleural membrane is folded in a manner that forms a pleural sac leaving an intrapleural space filled with a lubricating intrapleural fluid. The Respiratory System – Built for Gas Exchange Inside the lungs, bronchi narrow to form bronchioles ending in respiratory bronchioles. • • Tiny clustered sacs called alveoli (singular: alveolus) bulge out from the walls of the respiratory bronchioles. Together the alveoli provide a tremendous surface area for gaseous exchange, with the blood located in the dense capillary network surrounding each alveolar sac. bronchiole alveolar sac (sectioned) alveolar sac alveolar duct alveoli pulmonary capillary Fig. 11.1bc, p. 196 Nasal Cavity Oral Cavity (mouth) Pharynx (throat) Epiglottis Larynx (voice box) Pleural Membrane Trachea (windpipe) Intercostal Muscles Lung (one of a pair) Bronchial Tree Diaphragm bronchiole alveolar duct alveolar sac (sectioned) alveolar sac alveoli pulmonary capillary Fig. 11.1, p. 196 Section 2 Respiration = Gas Exchange Respiration = Gas Exchange Respiration is the overall exchange of inhaled oxygen from the outside air for exhaled carbon dioxide waste. This exchange occurs in the alveoli; afterward, the cardiovascular system is responsible for moving gases in the body. O2 O2 CO2 CO2 Cellular respiration in mitochondria Whole body respiration In-text Fig., p. 198 food, water intake oxygen intake DIGESTIVE SYSTEM nutrients, water, salts RESPIRATORY SYSTEM oxygen elimination of carbon dioxide carbon dioxide CARDIOVASCULAR SYSTEM URINARY SYSTEM water, solutes elimination of food residues rapid transport to and from all living cells elimination of excess water, salts, wastes Fig. 11-4, p. 198 Section 3 The “Rules” of Gas Exchange The “Rules” of Gas Exchange Respiratory systems rely on the diffusion of gases down pressure gradients. Air is 78% nitrogen, 21% oxygen, 0.04% carbon dioxide, and 0.96% other gases. • • Partial pressures for each gas in the atmosphere can be calculated; for example, oxygen’s is 160 mm Hg. Oxygen and carbon dioxide diffuse down pressure gradients from areas of high partial pressure to areas of low partial pressure. Total atmospheric pressure = 760 mm Hg 78% N2 Partial pressure of N2 = 600 mm Hg 21% O2 Partial pressure of O2 = 160 mm Hg 760 mm Hg 1% CO2, other gases Fig. 11.5, p. 198 The “Rules” of Gas Exchange Gases enter and leave the body by diffusing across thin, moist respiratory surfaces of epithelium; the speed and extent of diffusion depends on the surface area present and on the partial pressure gradient. The “Rules” of Gas Exchange When hemoglobin binds oxygen, it helps maintain the pressure gradient. Hemoglobin is the main transport protein. Each protein binds four molecules of oxygen in the lungs (high oxygen concentration) and releases them in the tissues where oxygen is low; by carrying oxygen away from the lungs, the gradient is maintained. The “Rules” of Gas Exchange Gas exchange “rules” change when oxygen is scarce. Hypoxia occurs when tissues do not receive enough oxygen; at high altitudes the partial pressure of oxygen is lower than at sea level, so that hyperventilation may occur. Figure 11.6a The “Rules” of Gas Exchange Underwater, divers must breathe pressurized air from tanks and avoid nitrogen narcosis, where nitrogen dissolves into the body, including the brain; divers must also ascend to the surface slowly to prevent nitrogen bubbles in the blood—the “bends” or decompression sickness. Figure 11.6b Section 4 Breathing— Air In, Air Out Breathing When you breathe, air pressure gradients reverse in a cycle. The respiratory cycle is the continuous in/out ventilation of the lungs and has two phases: • • Inspiration (inhalation) draws breath into the airways. Expiration (exhalation) moves a breath out of the airways. Breathing During the cycle, the volume of the chest cavity increases, then decreases, and the pressure gradients between the lungs and outside air reverse. • • This works because the air in the airways is the same pressure as the outside atmosphere. Pressure in the alveoli (intrapulmonary pressure) is also the same as the outside air. INWARD BULK FLOW OF AIR Inhalation Diaphragm contracts and moves down. The external intercostal muscles contract and lift the rib cage upward and outward. The lung volume expands. OUTWARD BULK FLOW OF AIR Exhalation Diaphragm and external intercostal muscles return to the resting positions. Rib cage moves down. Lungs recoil Fig. passively. 11.7, p. 200 Breathing The basic respiratory cycle. • • • To inhale, the diaphragm contracts and flattens, muscles lift the rib cage upward and outward, the chest cavity volume increases, internal pressure decreases, air rushes in. To exhale, the actions listed above are reversed; the elastic lung tissue recoils passively and air flows out of the lungs. Active exhalation involves contraction of the abdominal muscles to push the diaphragm upward, forcing more air out. Breathing Another pressure gradient aids the process. • • The lungs are stretched to fill the thoracic cavity by a slight difference between the intrapulmonary pressure (higher) and the intrapleural pressure (lower). In a collapsed lung (pneumothorax), air enters the pleural cavity, disrupting the normal expansion and contraction of the lungs. Breathing How much air is in a “breath”? About 500 ml of air (tidal volume) enters and leaves the lungs with each breath. • • A human can forcibly inhale 3,100 ml of air (inspiratory reserve volume) and forcibly exhale 1,200 ml (expiratory reserve volume). The maximum volume that can be moved in and out is called the vital capacity (4,800 ml for males, 3,800 ml for females). 6,000 Lung volume (milliliters) 5,000 4,000 inspiratory reserve volume tidal volume vital capacity total lung capacity 3,000 2,000 expiratory reserve volume 1,000 residual volume 0 time Fig. 11.8, p. 201 Breathing A residual volume of about 1,200 ml remains in the lungs and cannot be forced out. Sometimes food enters the trachea rather than the esophagus; it can be forced out by the Heimlich maneuver, which forces the diaphragm to elevate, pushing air into the trachea to dislodge the obstruction. a Place a fist just above the choking person’s navel, with the flat of your thumb against the abdomen. Fig. 11.9a, p. 201 b Cover the fist with your other hand. Thrust both fists up and in with enough force to lift the person off his or her feet. Fig. 11.9b, p. 201 Section 5 How Gases Are Exchanged and Transported How Gases Are Exchanged and Transported Ventilation moves gases into and out of the lungs; it is different from respiration, which is the actual exchange of gases between the blood and cells. In external respiration, oxygen moves from the alveoli to the blood; carbon dioxide moves in the opposite direction. In internal respiration, oxygen moves from the blood into tissues and vice versa for carbon dioxide. How Gases Are Exchanged and Transported Alveoli are masters of gas exchange. Each alveolus is only a single layer of epithelial cells surrounded by a thin basement membrane and a net of lung capillaries, also with thin basement membranes. • • • Between the two basement membranes is a film of fluid. Together the system forms the respiratory membrane. The partial pressure gradients are sufficient to move oxygen in and carbon dioxide out of the blood, passively. How Gases Are Exchanged and Transported Pulmonary surfactant is a secretion produced by the alveoli that reduces the surface tension of the film to prevent collapse of the alveoli; infant respiratory distress syndrome occurs in premature babies who lack the ability to make the surfactant. alveolar epithelium respiratory membrane capillary endothelium pore for air flow between adjoining alveoli space inside alveolus a Surface view of capillaries associated with alveoli b Cutaway view of one alveolus, showing the respiratory membrane red blood cell fusedtogether basement membranes of both epithelia c Closer view of the respiratory membrane’s structure Fig. 11.10, p. 202 pore for air flow between adjoining alveoli a. Surface view of capillaries associated with alveoli Fig. 11.10a, p. 202 pore for airflow between adjoining alveoli respiratory membrane (see next slide) space inside alveolus red blood cell b. Cutaway view of one alveolus, showing the respiratory membrane Fig. 11.10b, p. 202 alveolar epithelium capillary endothelium fused-together basement membranes of both epithelia c. Closer view of the respiratory membrane’s structure Fig. 11.10c, p. 202 How Gases Are Exchanged and Transported Hemoglobin is the oxygen carrier. Blood cannot carry sufficient oxygen and carbon dioxide in dissolved form as the body requires; hemoglobin helps enhance its capacity to carry gases by transporting oxygen. • • Oxygen diffuses down a pressure gradient into the blood plasma >>> red blood cells >>> hemoglobin where it binds at a ratio of four oxygens to one hemoglobin to form oxyhemoglobin. Hemoglobin gives up its oxygen in tissues where partial pressure of oxygen is low, blood is warmer, and pH is lower; all three conditions occur in tissues with high metabolism. O2 160 DRY INHALED AIR CO2 0.3 O2 120 MOIST CO2 27 EXHALED AIR alveolar sacs O2 104 CO2 40 pulmonary O2 40 arteries CO2 45 O2 100 pulmonary veins CO2 40 start of systematic capillaries O2 100 CO2 40 start of systematic veins O2 40 CO2 45 cells of body tissue O2 less than 40 CO2 more than 45 © 2007 Thomson Higher Education Fig. 11.11, p. 203 How Gases Are Exchanged and Transported When tissues are chronically low in oxygen, red blood cells produce DPG (2,3diphosphoglycerate), which decreases the affinity of hemoglobin for oxygen, allowing more oxygen to be released to the tissues. Hemoglobin and blood plasma carry carbon dioxide. Because carbon dioxide concentration is higher in the body tissues rather than in blood, it diffuses into the blood capillaries. How Gases Are Exchanged and Transported • Seven percent remains dissolved in plasma, 23% binds with hemoglobin (forming carbaminohemoglobin) and 70% is in bicarbonate form. • Bicarbonate and carbonic acid formation is enhanced by carbonic anhydrase, an enzyme located in the red blood cells. Reactions that make bicarbonate are reversed in the alveoli where the partial pressure of carbon dioxide is low. Section 6 Homeostasis Depends on Controls over Breathing Homeostasis Depends on Controls Over Breathing A respiratory pacemaker controls the rhythm of breathing. Automatic mechanisms ensure a regular cycle of ventilation. • • Clustered nerve cells in the medulla coordinate the signals for the timing of exhalation and inhalation; the pons fine tunes the rhythmic contractions. The nerve cells are linked to the diaphragm muscles and the muscles that move the rib cage; during normal inhalation, nerve signals travel from the brain to the muscles causing them to contract and allowing the lungs to expand. Homeostasis Depends on Controls Over Breathing Normal exhalation follows relaxation of muscles and elastic recoil of the lungs. When breathing is deep and rapid, stretch receptors in the airways send signals to the brain control centers, which respond by inhibiting contraction of the diaphragm and rib muscles, forcing you to exhale. neurons (pacemaker for respiration) brain stem (pons and medulla) vagus nerve motor pathways via spinal cord phrenic nerve to diaphragm intercostal nerves to rib muscles stretch receptors in alveoli of lungs diaphragm © 2007 Thomson Higher Education Fig. 11.12, p. 204 Homeostasis Depends on Controls Over Breathing CO2 is the trigger for controls over the rate and depth of breathing. The nervous system is more sensitive to levels of carbon dioxide and uses this gas to regulate the rate and depth of breathing. • • Sensory receptors in the medulla detect hydrogen ions produced when dissolved carbon dioxide leaves the blood and enters the cerebrospinal fluid bathing the medulla. The drop in pH in the cerebrospinal fluid triggers more rapid and deeper breathing to reduce the levels of carbon dioxide in the blood. Homeostasis Depends on Controls Over Breathing Changes in the levels of carbon dioxide, oxygen, and blood pH are also detected by carotid bodies, located near the carotid arteries, and aortic bodies, located near the aorta; both receptors signal increases in ventilation rate to deliver more oxygen to tissues. brain-stem (pons and medulla) receptors detect decreases in pH of cerebrospinal fluid (due to rising CO2 in blood) carotid bodies (CO2, O2 receptors) aortic bodies (O2 receptors) heart lungs spinal cord © 2007 Thomson Higher Education Fig. 11.13, p. 205 Homeostasis Depends on Controls Over Breathing Chemical controls in alveoli help match air flow to blood flow. When the rate of blood flow in the lungs is faster than the air flow, the bronchioles dilate to enhance the air flow and thus the rate of diffusion of the gases. When the air flow is too great relative to the blood flow, oxygen levels rise in the lungs and cause the blood vessels to dilate, increasing blood flow. Homeostasis Depends on Controls Over Breathing Apnea is a condition in which breathing controls malfunction. Apnea is a brief interruption in the respiratory cycle; breathing stops and then resumes spontaneously. Sleep apnea is a common problem of aging because the mechanisms for sensing changing oxygen and carbon dioxide levels gradually become less effective over the years. Section 7 Disorders of the Respiratory System Disorders of the Respiratory System Tobacco is a major threat. Smoking has both immediate effects (for example, loss of cilia function) and long term effects, such as lung cancer. Even one cigarette can cause you damage as well as hurt those around you through secondhand smoke. A variety of pathogens can infect the respiratory system. Figure 11.17 Fig. 11.14b, p. 206 Disorders of the Respiratory System Pneumonia occurs when inflammation in lung tissue and the buildup of fluids makes breathing difficult; pneumonia can sometimes occur when infections that start in the nose and throat, such as from influenza, spread. Tuberculosis arises from infection by the bacterium Mycobacterium tuberculosis; the disease destroys patches of lung tissue and can cause death if untreated. Histoplasmosis is caused by a fungus; treatment is possible, but the infection can sometimes spread to the eyes, causing impairment or blindness. Disorders of the Respiratory System Irritants cause other disorders. Bronchitis, caused by air pollution, cigarette smoke, or infection, leads to increased mucus secretions, interference with ciliary action, and eventual inflammation and possible scarring of the bronchial walls. Figure 11.18 Fig. 11.18a, p. 210 Disorders of the Respiratory System If bronchitis progresses so that more of the bronchi become scarred and blocked with mucus, emphysema may result; here alveoli also begin to break down, further eroding the ability to breathe. Fig. 11.15, p. 207 Disorders of the Respiratory System Asthma occurs in response to various allergens; smooth muscles in the bronchiole walls contract in spasms, mucus rushes in, and breathing becomes difficult. Steroid inhalers may be needed to relieve symptoms. Figure 11.16