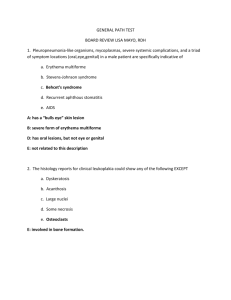
lecture 5
advertisement

Lecture5 / 16-5-2013 *One of clinical aspects related to blood is "Anemia", which means a decrease in hemoglobin in blood, due to abnormalities on globins' chains or deficiency in some minerals. Abnormalities on globins' chains: 1- Sickle cell anemia : Caused by a mutation which happens when changing of just one amino acid in one of the 2 β polypeptide chains in the hemoglobin .this shows how specific the amino acid chain is. (a changing only in one amino acid, could be so effective ) This type of anemia produces a sickle red blood cells which are deformed cells, can block blood vessels and prevent tissues from receiving oxygen. This deficiency of oxygen called hypoxia. 2-Thalassemia: Caused by absence of chains in hemoglobin. An absence of one chain either α or β"minor or heterozygous" or absence of both chains from the same kind "major or homogenous". β thalassemia: if the β chain is absence. α thalassemia: if the α chain is absence. Controlling the number of red blood cells: Red blood cells in adults produced in the bone marrow. Because RBCs are an Anucleated cells it have a life span of around 120 day for the normal cells. Un normal cells have shorter life span. Erythropoietin is a controller hormone of red blood cells number which has to be constant. This protein is produced in kidney in the adult and the liver in the fetus. it works on bone marrow stimulating production of RBCs . the oxygen level on our blood is the controlled condition which controls production of erythropoietin: If the level of oxygen decrease ( a hypoxia occurs) this stimulates the kidney to produce more erythropoietin with the result that more red blood cells will be produced when erythropoietin reaches bone marrow . If the level of oxygen increase again (when an appropriate increase of the number of RBCs occurs) this suppress the production of erythropoietin in kidney cells. - a negative feedback- . See figure 19.6 page 738 RBC life cycle: After 120 days of the RBC life, macrophages in liver or spleen phagocytize ruptured red blood cells. When it phagocytozed. the hemoglobin split apart and separates to" heme + globin" Globin is broken into amino acids that reused for protein synthesis. An iron is removed from the heme then the non-iron heme is broken, and got a straight form called beliverdin which is a green in color. Then Beliverdin hydrogenated and converted into belirubin (the bile pigment) which is yellow pigment that gives the gallbladder fluid its yellow color. Bilirubin secreted from the liver to the gallbladder then to the duodenum and finally enters the large intestine where the bacteria converted it to stercobilin which is the pigment that gives the stool its brown color. The iron which removed from heme is associates with the plasma protein transferrin. iron-transferrin complex is formed Then this transferrin transfer the iron to the bone marrow where it's plays a role in erythropoiesis. Note: Erythropoiesis is the production of red blood cells. ]iron + globin + vitamin B12 +erythropoietin= RBC[ *this process is the erythropoiesis * Some of access iron stored on the bone marrow, spleen or liver, where the iron detaches from transferrin and attaches to iron-storage protein called ferritin. See figure 19.5 page736 Important Note: -related to point five of RBC life cycleThe bacteria in large intestine converted bilirubin to urobilinogen which have two forms: 1-Urobilinogen absorbed back into the blood converted to urobilin: a yellow pigment that excreted in urine 2- Urobilinogen is eliminated in the feces in form of stercobilin: a brown pigment which gives stools (feces) the brown color. Clinical aspects: Jaundice: is the increase of the level of bilirubin in the blood (hyperbilirubinemia). It is always a sign of liver dysfunction. Obstructive jaundice: causes obstruction of bilirubin, so it can't reach the large intestine. With the result that, the stools will be white in color (due to absence of stercobilin). And the urine will be red (Due to secretion of bilirubin in urine). Anemia: Iron deficiency anemia: due to deficiency of iron. The cell becomes smaller "microcyte" because of little amount of hemoglobin. And it becomes hypochromic (in color). B12 deficiency anemia: it called macrocytic anemia or megaloplastic anemia due to enlarge of red blood cells .it may result from different causes : 1-nutritional deficiency 2-removal of stomach, ileum or a diseases on them, which cause a problem in absorbing B12 ,because it reabsorbs on ileum by a factor secretes from stomach. *We can solve this problem by injections. Note: anemia accelerate the production of red blood cells that increases reticulocyte number in blood. (More than 1% or 2%) White blood cells (WBCs) WBCs are also produced by hematopoiesis in bone marrow. Types of WBCs : Granular leukocytes (granulocyte): these cells have granules on their cytoplasm. This type divided into three kinds according to the stain they accept : 1-Neutrophil 2-Eosinophil: *they are acidophilic 3-Basophil:* they are basophilic (basic loving) Agranular leukocytes: have no granules in the cytoplasm. This type Contains: 1- Monocyte: very large macrophages 2- Lymphocytes: T lymphocyte and B lymphocyte. Note: In embryo T lymphocytes are differentiated in thymus gland that's why called "T" lymphocytes. And B lymphocytes called like this because it comes from bursa or bone marrows then it differentiate into special kind of lymphocytes. *differential leukocytic count: -DLCuse to determine which kind of leukocyte has the abnormality high range. For example to determine either the infection is viral (high abnormality of lymphocytes number) or bacterial (high abnormality of neutrophils number). High number of basophils is due to allergy. And abnormality of monocytes number (monocytosis) is due to bacterial infection. *leukemia: uncontrolled increase in leukocyte count. Done by: Mais Al-Reem Al-housani