Acute Gastroenteritis: An Approach
Acute Gastroenteritis:
An Approach
Paolo Aquino, M.D., M.P.H.
Approach
Etiology
Diagnosis
Treatment
Prevention
Outline
Considerations
Approach
• Rule out acute/surgical abdomen
• Hydration status
Acute Abdomen
Intraluminal
Obstruction
Extraluminal
Obstruction
Gastrointestin al
Disease
Paralytic
Ileus
Blunt
Trauma
Miscellaneous
Foreign Body
Bezoar
Fecalith
Gallstone
Parasites
Cystic fibrosis
Tumor
Fecaloma
Hernia
Intussusceptio n
Volvulus
Duplication
Stenosis
Tumor
Mesenteric cyst
SMA syndrome
Pyloric stenosis
Appendicitis
Crohn disease
Ulcerative colitis
Vasculitis
Peptic ulcer disease
Meckel’s
AGE
Sepsis
Pneumonia
Pyelonephritis
Peritonitis
Pancreatitis
Cholecystitis
Renal stones
Gallstones
PID
Lymphadenitis
Accident
Battered child syndrome
Lead poisoning
Sickle cell disease
Familial
Mediterranean fever
Porphyria
DKA
Addisonian crisis
Testicular torsion
Ovarian Torsion
Approach
History
• Symptoms
Nausea, emesis, retching
Abdominal pain
Bowel movements
Timing
• Age
• Onset
• Relation to feeds
• Focus of infection, other affected individuals
Approach
Physical examination
• Temperature, heart rate, blood pressure, pain
• Abdominal examination
Auscultation before palpation
Palpation
• Masses
• Tenderness
Auscultation for bowel sounds
Approach
Objectives
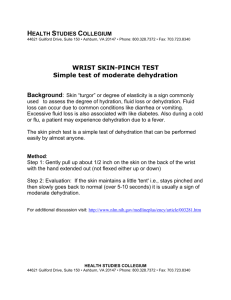
• Assess the degree of dehydration
• Prevent spread of the enteropathogen
• Selectively determine etiology and provide specific therapy
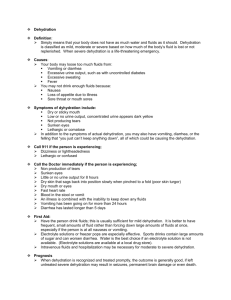
Dehydration
Mild (3-5%)
• Normal or increased pulse
• Decreased urine output
• Thirsty
• Normal physical exam
Dehydration
Moderate (7-10%)
• Tachycardia
• Little/no urine output
• Irritable/lethargic
• Sunken eyes/fontanelle
• Decreased tears
• Dry mucous membranes
• Skin- tenting, delayed cap refill, cool, pale
Dehydration
Severe (10-15%)
• Rapid, weak pulse
• Decreased blood pressure
• No urine output
• Very sunken eyes/fontanelle
• No tears
• Parched mucous membranes
• Skin- tenting, delayed cap refill, cold, mottled
Dehydration
Treatment
• Calculate deficits
Water: % dehydration x weight
Sodium: water deficit x 80 mEq/L
Potassium: water deficit x 30 mEq/L
• Treat mild-moderate dehydration with oral rehydration solutions
• May treat severe dehydration with intravenous fluids
• Hyponatremic v. isotonic v. hypernatremic
Etiology
Enteropathogens
• Non-inflammatory vs. inflammatory diarrhea
Non-inflammatory
• Enterotoxin production
• Destruction of villi
• Adherence to GI tract
Inflammatory
• Intestinal invasion
• Cytotoxins
Etiology
Chronic diarrhea
• Giardia lamblia
• Cryptosporidium parvum
• Escherichia coli: enteroaggregative, enteropathogenic
• Immunocompromised host
• Non-infectious causes: anatomic, malabsorption, endocrinopathies, neoplasia
Etiology
Bacterial
• Inflammatory diarrhea
Aeromonas
Campylobacter jejuni
Clostridium dificile
E. coli: enteroinvasive, O157:H7
Plesiomonas shigelloides
Salmonella
Shigella
Vibrio parahaemolyticus
Yersinia enterocolitica
Etiology
Bacterial
• Non-inflammatory
E. coli: enteropathogenic, enterotoxigenic
Vibrio cholerae
Viral
• Rotavirus
• Enteric adenovirus
• Astroviruus
• Calcivirus
• Norwalk
• CMV
• HSV
Etiology
Parasites
• Giardia lamblida
• Entamoeba histolytica
• Strongyloides stercoralis
• Balantidium coli
• Cryptosporidium parvum
• Cyclospora cayetanensis
• Isospora belli
Diagnosis
History
Stool examination
• Mucus
• Blood
• Leukocytes
• Stool culture
Diagnosis
Examination for ova and parasites
• Recent travel to an endemic area
• Stool cultures negative for other enteropathogens
• Diarrhea persists for more than 1 week
• Part of an outbreak
• Immunocompromised
• May require examination of more than one specimen
Antimicrobial therapy
Aeromonas
• TMP/SMZ
• Dysentery-like illness, prolonged diarrhea
Campylobacter
• Erythromycin, azithromycin
Clostridium dificile
• Metronidazole, vancomycin
E. coli
• TMP/SMZ
Antimicrobial therapy
Salmonella
• Cefotaxime, ceftriaxone, ampicillin, TMP/SMZ
• Infants < 3 months
• Typhoid fever
• Bacteremia
• Dissemination with localized suppuration
Shigella
• Ampicillin, ciprofloxacin, ofloxacin, ceftriaxone
Vibrio cholerae
• Doxycycline, tetracycline
Therapy
Antidiarrheal medication
• Alter intestinal motility
• Alter adsorption
• Alter intestinal flora
• Alter fluid/electrolyte secretion
Antidiarrheal medication generally not recommended
• Minimal benefit
• Potential for side effects
Prevention
Contact precautions
Education
• Mode of acquisition
• Methods to decrease transmission
Exclusion from day care until diarrhea subsides
Surveillance
Salmonella typhi vaccine
Any questions?