Vibrio cholera
advertisement

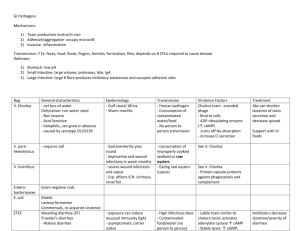
Non Invasive Enteritis II Barriers to GIT infection: • • • • • • • Stomach acidity (low PH). Mucus layer and gut motility (peristalsis)→ prevent adhesion. The glycocalyx (mucin rich layer) covers the epithelial cells surface→ entrap invading bacteria. Shedding of mucosal epithelium lining the GIT. Bile secretion prevent the growth of non-enteric bacteria and enveloped viruses. M cells (microfold) of Peyer’s patches which have a surveillance function (sampling). Normal flora of intestinal tract. Secretory IgA. Bacterial enteritis: • Non invasive → multiplication within the lumen and toxin production → watery diarrhea. Causative agents: o V. cholerae. o Enterobacteriaceae: Enterotoxigenic E. coli, Enteropathogenic E. coli. • Local invasion → invade and destruct the mucosa and the epithelia → bloody diarrhea. E.g. Shigella and Enterohemorrhagic E.coli, Campylobacter jejuni, Salmonella enteriditis ……. • Systemic invasion → Cuasative bacteria can be isolated from the blood; Salmonella Typhi, Brucella. Vibrio cholerae Vibrionaceae: gram negative rods, curved, motile by single polar flagellum. Alkaliphiles (pH 6.8-10). Vibrionaceae family: o Vibrio cholerae → cholera (watery diarrhea). o Vibrio parahaemolyticus. o Vibrio vulnificus. V. cholerae has ≈ 140 serotypes based on its LPS (O antigen). Serotype O1 is the most common followed by serotype O139. V. cholerae serotype O1 has 2 biotypes: • Classical. • El Tor. N Epidemiology: o Vibrio cholerae O1 biotype classical → 6 pandemics in Asia for centuries. o Vibrio cholerae O1 biotype El Tor was isolated from pilgrims at El Tor station in 1905.It had caused the seventh pandemic in1961. o Infections with the new serotype Vibrio cholera O139 (Bengal) appeared in Bangladesh in 1990 and spread to India and other countries. o Cholera cause ≈ 3 millions cases and 10000 deaths yearly. Pathogenesis and Microbial Virulence: Transmission: Source: human cases or carrier. Human disease only without animal reservoir. o Waterborne: drinking un-boiled or untreated water. o Foodborne; Contaminated sea food or shellfish. o Fecal-oral route: human carriage (colon) is reported in some cases. Pathogenesis: o Pathogenic dose: 108-109 CFU/ml (lower in hypochlorohydria). o When vibrios reach ampulla of Vater in the duodenum; surviving organisms are bathed in bicarbonate-buffered pancreatic juice (pH can be as high as 9). n o Vibrios reach the epithelia of the small intestine by flagella & mucinase enzyme that hydrolyses the mucus. o Adhere to the epithelia of the intestinal tract by type 1 common pili (colonization factor antigen Cfa). o Vibrios stick to each other and establish colonization (micro-colonies) by toxin-co-regulated pili (TCP). o Produce cholera toxin. Cholera toxin (Ctx) binds to the receptor on epithelial cells → stimulate G protein → activate the adenylate cyclase → increase cAMP production → inhibit sodium absorption and increase chloride secretion by enterocytes → ↑NaCl in the lumen→ passive secretion of water → severe watery diarrhea + mucus (the action of the mucinase) → Rice Water Diarrhea. Flagella, mucinase, Cfa, TCP Clinical presentation: • Incubation period: 2 hours – 5 days (inoculum size) • Sever watery diarrhea (rice water without faecal matter) and vomiting of clear fluid. No fever Dehydration and electrolytes imbalance (patients may lose 10-20 liters of fluid/ day) dry mouth and skin; decreased skin turgor. • Deep rapid breathing due to acidosis: • Rapid pulse. • Coma (Na, Cl loss). • Death: 70% if not treated 0.5% with treatment. Rice water diarrhea N Laboratory diagnosis: Clinical specimens: stool. Microscopy (diagnostic in endemic area): • Wet mount: highly motile bacilli which stop moving when we add specific antisera. • Gram stain: Vibrios are gram-negative curved bacilli, motile with a single polar flagellum. Antigen detection: detect the O1 or O139 antigens or the cholera toxin. Cultural and isolation (diagnostic in non endemic area i.e. gold standard) : • Media: o Blood agar: usually beta hemolytic (El Tor). o MacConkey's agar: non-lactose fermenting colonies. o Alkaline peptone water: Selective media; pH 8.5-9 o TCBS: Thiosulfate-citrate-bile salts-sucrose agar; Selective and differential → change the color from green to yellow. • Biochemical reactions: catalase, oxidase and indole positive and can reduce nitrate to nitrite (cholera red reaction positive). Diagnosis Serotyping and biotyping: Epidemiological purposes. PCR: detect nucleic acid in the sample. Treatment: - Fluid and electrolyte replacement in early stage (life saving). - Antibiotics: Tetracycline or co-trimoxazole. Oxidase Test Indole Test Prevention: - Prevent transmission: food and water hygiene & acidification of food. - Vaccines: killed vaccine with recombinant binding subunit of the cholera toxin. Non Cholera Vibrios Vibrio parahaemolyticus: • Halophilic microbes. • Transmission: consumption of undercooked or raw seafood; shellfish, and crustaceans. • Gastroenteritis: fever, abdominal pain, watery diarrhea some times with blood due to invasive enteritis. Vibrio vulnificus: Halophilic vibrio. Transmission: undercooked shellfish or exposure of wound to salt water. Invasive enteritis; associated with high mortality rate (septicemia and death). Wound infection. Flesh eating bacteria (V. vulnificus) Escherichia coli: E. coli groups associated diarrhea: Watery diarrhea: Enteroaggregative E. coli Watery toxin mediated diarrhea: o Enterotoxigenic E. coli. o Enteropathogenic E. coli. Bloody diarrhea due to invasive enteritis: o Enterohemorrhagic E. coli. o Enteroinvasive E. coli. Enterotoxigenic E. coli: the causative agent of traveler’s diarrhea. Produce two enterotoxins: - Heat labile (LT): activate G protein and adenylate cyclase; ↑cAMP. (same effect of cholera toxin). - Heat stable (ST): activate guanylate cyclase. → watery diarrhea. Enteropathogenic E. coli: Cause watery diarrhea in infants. Adhere to the epithelial cells by Cfa pilus & insert exotoxin Tir (translocation intimin receptor) → brush border damage; malabsorption and watery diarrhea. Ctx: cholera toxin. ST: heat stable toxin. LT: labile toxin. Cfa: colonization factor antigen.