40131
advertisement

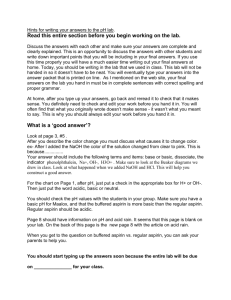
UPDATE ON ANTIPLATELET THERAPY IN THE TREATMENT AND PREVENTION OF CARDIOVASCULAR DISEASE Charles H Hennekens, MD, DrPH Sir Richard Doll Research Professor of Medicine Charles E. Schmidt College of Medicine Florida Atlantic University Clinical Professor of Preventive Medicine Nova Southeastern University Voluntary Professor of Family Medicine and Community Health University of Miami Miller School of Medicine Disclosure Dr. Hennekens receives investigator initiated research grant support from Bayer to the Charles E. Schmidt College of Medicine at Florida Atlantic University. He serves as an independent scientist in an advisory role to investigators and sponsors, including as Chair or member of Data and Safety Monitoring Boards to Actelion, Amgen, Anthera, Bayer, Bristol-Myers Squibb, Canadian Institutes of Health Research, Dainippon-Sumitomo, National Association for Continuing Education,, Pozen, Pfizer, PriMed, United States (US) Food and Drug Administration, U.S.National Institutes of Health, and UpToDate. He serves as an independent scientist in an advisory role to legal counsel for GlaxoSmithKline and Stryker. He serves as speaker for the Association for Research in Vision and Ophthalmology, AstraZeneca, International Atherosclerosis Society, and Pfizer. He receives royalties for authorship or editorship of three textbooks and as co-inventor on patents held by Brigham and Women’s Hospital concerning inflammatory markers for cardiovascular disease. He has an investment management relationship with The West-Bacon Group within SunTrust Investment Services who has sole discretionary investment authority. He owns no common or preferred stock in any pharmaceutical or device industry. Death is inevitable but premature death is not. Sir Richard Doll OBJECTIVES Aspirin in the treatment of CVD Additive benefits of aspirin and statins Aspirin in the prevention of CVD Dual antiplatelet therapy in CVD Newer antiplatelet agents in CVD Milestones For Aspirin 5th century BC Hippocrates 1897 AD Felix Hoffman/Friedrich Bayer synthesize aspirin 20th Century Aspirin becomes the most widely used drug in the world for pain relief 1971 John Vane discovers CVD mechanism 1988 Physician’s Health Study shows aspirin prevents first MI 1988 APT shows aspirin decreases MI, stroke, and CVD death for survivors of MI and stroke 1988 ISIS-2 shows aspirin decreases mortality during acute MI Moses Receiving The Tablets From God Milestones For Aspirin 5th century BC Hippocrates 1897 AD Felix Hoffman/Friedrich Bayer synthesize aspirin 20th Century Aspirin becomes the most widely used drug in the world for pain relief 1971 John Vane discovers CVD mechanism 1988 Physician’s Health Study shows aspirin prevents first MI 1988 APT shows aspirin decreases MI, stroke, and CVD death for survivors of MI and stroke 1988 ISIS-2 shows aspirin decreases mortality during acute MI Milestones For Aspirin 5th century BC Hippocrates 1897 AD Felix Hoffman/Friedrich Bayer synthesize aspirin 20th Century Aspirin becomes the most widely used drug in the world for pain relief 1971 John Vane discovers CVD mechanism 1988 Physician’s Health Study shows aspirin prevents first MI 1988 APT shows aspirin decreases MI, stroke, and CVD death for survivors of MI and stroke 1988 ISIS-2 shows aspirin decreases mortality during acute MI Milestones For Aspirin 5th century BC Hippocrates 1897 AD Felix Hoffman/Friedrich Bayer synthesize aspirin 20th Century Aspirin becomes the most widely used drug in the world for pain relief 1971 John Vane discovers CVD mechanism 1988 Physician’s Health Study shows aspirin prevents first MI 1988 APT shows aspirin decreases MI, stroke, and CVD death for survivors of MI and stroke 1988 ISIS-2 shows aspirin decreases mortality during acute MI The Most Plausible Mechanism Of Aspirin In Reducing Risks Of Cardiovascular Disease Aspirin irreversibly acetylates the active site of cyclooxygenase, which is required for the production of thromboxane A2, a powerful promoter of platelet aggregation Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action of aspirin like drugs. Nat New Biol. 1971;231:232-5. Totality Of Evidence Basic research (why) Epidemiology (whether) descriptive studies case reports case series ecological studies Hennekens. Epidemiology in Medicine. 1987. analytic studies observational case-control cohort randomized trials Observational Epidemiologic Studies Some but not all case-control & cohort studies indicate that individuals and/or their health care providers who selfselect for aspirin have lower risks of CVD. For most epidemiologic hypotheses, randomized trials are neither necessary nor desirable For small to moderate effects, however, the only reliable design strategy is the large randomized trial because the amount of uncontrolled & uncontrollable confounding factors inherent in observational studies can be as large as the effect sizes Hennekens CH, DeMets D: The need for large scale randomized evidence without undue emphasis on small trials, their meta-analyses or subgroup analyses JAMA 2009 Evolution of Antiplatelet (AP) Therapy Trials Year No Of Trials No Of Patients 1988 25 25,000 1997 194 212,000 AP vs control (135,000) Different AP (77,000) Antithrombotic Trialists’ Collaboration. BMJ. 2002;324:71. Aspirin in the Treatment of CVD In a wide range of patients who have survived a prior occlusive event (including MI, occlusive stroke or transient ischemic attack, or other high risk categories including unstable and stable angina, angioplasty, or coronary artery bypass graft), antiplatelet therapy, principally with aspirin, prevents ~25% of serious vascular events, including significant reductions on MI, stroke, and CVD death. All these patients have 10-year risks of CHD of 20% or more based on the Framingham risk score recommended by the US NHLBI. AntiThrombotic Trialists Collaboration. Lancet, 2002 Benefits of Aspirin on Risk of Stroke In 158 trials, there were 3,522 nonfatal and 1,424 fatal strokes after randomization. Antiplatelet therapy, principally with aspirin, reduced stroke by about 25%, regardless of whether the patient entered the trial with prior MI, stroke, TIA, or other high-risk conditions. Antiplatelet therapy, principally with aspirin, increases the absolute risk of hemorrhagic stroke by 3 per 10,000 treated patients. The upper bound of the 95% confidence interval is less than 1 per 1000 treated patients. AntiThrombotic Trialists Collaboration. Lancet, 2002 Second International Study of Infarct Survival ISIS-2 Collaborative Croup Lancet. 1988 Aug 13;332: 349-60. Hypothesis: Additive Benefits of Statins and Aspirin to Decrease Risks of CVD ATHEROSCLEROSIS The principal underlying cause of occlusive CVD events which is inhibited by statins THROMBOSIS The principal proximate cause of occlusive CVD events which is inhibited by aspirin Hebert P, Pfeffer MA, Hennekens CH: Use of Statins and Aspirin to Decrease Risks of CVD J CV Pharm Ther. 2002;7:77-80 Summary: Additive Benefits of Aspirin and Statins in Secondary Prevention of CVD A meta-analysis of 5 trials in secondary prevention of CVD of over 15,000 patients with over 73,000 patient-years of observation demonstrated that the combination of aspirin and statins provided statistically significant and clinically important additive benefits for the prespecified individual endpoints of fatal or non-fatal MI as well as ischemic stroke and a combined endpoint of CHD death, nonfatal MI, CABG, PTCA or ischemic stroke: The probability of synergy (i.e. greater than additive benefits) was 0.92. These statistically significant and clinically important benefits were also present in individual analyses of data from the LIPID and CARE trials Hennekens CH, et al. Arch Int Med, 2001. Greater Relative Risk Reductions (RRR) for Pravastatin (Prava) + Aspirin (ASA) versus Prava or ASA alone RRR Relative Risk (95% CI) Fatal or Non-Fatal MI 0.69 Prava+ASA vs ASA Alone 31% 0.74 26% Prava+ASA vs Prava Alone 0.400 0.600 0.800 1.000 Ischemic Stroke 0.71 Prava+ASA vs ASA Alone 0.69 Prava+ASA vs Prava Alone 0.400 29% 0.600 31% 0.800 1.000 CHD Death, Non-Fatal MI, CABG, PTCA, or Ischemic Stroke 0.76 Prava+ASA vs ASA Alone 0.87 Prava+ASA vs Prava Alone 0.400 24% 0.600 Hennekens CH et al. Arch Int Med 2004; 164:945-948. 0.800 13% 1.000 Summary: Aspirin in Primary Prevention of CVD In a comprehensive worldwide meta analysis of the 6 randomized trials of primary prevention aspirin produces a statistically significant and clinically important reduction in risk of a first myocardial infarction by about 1/3 but the available data on stroke and cardiovascular death remain inconclusive In these apparently healthy men and women at low risk aspirin is of uncertain net value as the reduction in occlusive events needs to be weighed against any increase in major bleeds. The average 10 year risk of a first CHD event among the apparently healthy men and women in the 6 randomized trials is less than 5%. The chief need is for randomized evidence in apparently healthy individuals whose 10 year risk of a first CHD event is 10-19%. Until then any decision to use aspirin in primary prevention should be an individual clinical judgement by the healthcare provider. Writing Group (Baigent C, Blackwell L, Buring J, Collins R, Emberson J, Godwin J, Hennekens C, Kearney P, Meade T, Patrono C, Peto R, Roncaglioni R, Zanchetti A). Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data. Lancet. 2009;373:1849-60. 10-Year Risk of a First CHD Event in the Six Major Trials of Aspirin in Primary Prevention of CVD WHS 2.5% HOT 3.6% PPP 4.3% PHS 4.8% BMD 8.9% TPT 12.4% Dose Of Aspirin: Indirect Comparisons No Trials % Reduction (SE) 3P value 500-1500 34 19 (3) <0.00001 160-325 19 26 (3) <0.00001 75-150 12 32 (6) <0.0001 <75 3 13 (8) NS 68 23 (2) <0.0001 Regimen Aspirin Alone (mg) Total X32 het = 8.2, P=.04. . AntiThrombotic Trialists Collaboration. Lancet, 2002 Time To Achieve Maximal Inhibition Of Serum Thromboxane B2 With 75 mg ASA Hennekens CH and Schneider W. Expert Rev Cardiovasc Ther. 2008; 6: 95-107 Indirect and Direct Comparisons Between Daily Aspirin Doses of 325mg or less and Major Extracranial Bleeding in the Secondary Prevention Trials Indirect comparisons: In meta-analyses of trials of daily aspirin doses of 325mg or less (160325, 75-160, or <75), risks of major extracranial bleeds were similar. Direct comparisons: In the two trials that directly compared daily aspirin doses of 75-325mg with <75mg, risks of major extracranial bleeds were similar. AntiThrombotic Trialists Collaboration. Lancet, 2002 Optimal Dosing For Aspirin In CHD Secondary Prevention & Primary Prevention 75 mg – 325 mg Acute CVD Syndrome 162.5 mg – 325 mg Hennekens CH, Dyken M, Fuster V:Circ. 1997 Effects On Platelets ASA Irreversible inhibition NSAIDS Reversible inhibition Possible but unproven small clinical CVD benefits of naproxen Possible but unproven inhibition of clinical CVD benefits of aspirin by ibuprofen COXIBS Acetaminophen Hennekens CH, Borzak S: JCPT, 2008 Prothrombotic effects and risks of similar magnitude to NSAIDS on CVD No effects on platelets but risks on liver and kidneys Dose-Dependent Side Effects of Aspirin The 5 Year UK-TIA Trial of about 2400 Side Effects Placebo 300 mg 1200 mg GI Symptoms 25% 29% 39% GI bleeding requiring transfusion 1.6% 2.6% 4.9% Warlow C. et al. BMJ, 1988 Possible Additional Beneficial Mechanisms of Action of Higher Doses of Aspirin on CVD Enhance nitric oxide formation Decrease inflammation Stabilize endothelial function Hennekens CH, Sechenova, O, Hollar D, Serebruany VL. Dose of Aspirin in the Treatment and Prevention of Cardiovascular Disease: Current and Future Directions. JCPT 2006. Hennekens CH, et al. A randomized trial of aspirin at usual clinical doses and increased nitric oxide formation in humans. JCPT 2010. Lack of Sex Differences in Response to Aspirin: ATT Patients with Prior MI or Stroke Percent Reductions Endpoint Men Women Major coronary events 19% 25% Stroke 17% 22% Hennekens CH, Hollar D, Baigent C. Sex differences in response to aspirin in CVD: an hypothesis formulated but not tested. Nature: Cardiovascular Medicine 2006,3:4-5 Dual Antiplatelet Therapy Risks versus Monotherapy Benefits and risks: Aspirin + Dipyrimadole Aspirin + Clopidogrel Issues with Clopidogrel Clopidogrel versus Prasugrel Clopidogrel versus Ticagrelor DUAL ANTIPLATELET THERAPY AND INCREASED RISKS OF BLEEDING In a meta-analysis of 18 randomized trials which included 129,314 patients Those assigned to dual antiplatelet therapy have about a 50% increase in risks of major bleeding compared with those given single agent therapy The magnitude of these excess risks are about as high as the approximately 60% increase observed in the trials comparing single antiplatelet agents to placebo These excess risks of major bleeding should be considered in relation to the benefits on occlusive CVD events in choosing the optimal antiplatelet strategy, especially for long-term treatment of patients with prior events or those at high risk of developing CVD. Fund Clin Pharm 2008; 22:315-321 Aspirin + Dipyrimadole: Second European Stroke Study (ESPS-2) Randomized, double-blind placebo controlled 2x2 factorial trial 6602 patients with prior ischemic stroke or TIA ASA (25mg bid) and/or dipyrimadole (200mig bid sustained release) Deaths from stroke were reduced 13% by ASA (p=0.016) 15% by dipyrimadole (p=0.039) 24% by the combination of ASA and dipyrimadole (p<0.001) Diener, HC et al J Neurol Sci .1996 Nov; 143: (1-2)1-13 Aspirin + Dipyridamole: PROFESS 20,332 post-ischemic stroke patients within 120 days Randomized to aspirin 25mg +extended release dipyrimadole 200mg bid vs clopidogrel 75mg qd After 2.5 years there were similar rates of the primary prespecified composite endpoint of stroke, MI or vascular death. NEJM, 2008;359:1238-1251 Clopidogrel + Aspirin Clopidogrel adds to the benefit of aspirin in some circumstances. CURE, a randomized trial of acute MI, showed that clopidogrel adds to the benefit of aspirin on CVD events but increased major bleeding. COMMIT/CCS-2, a randomized trial of acute coronary syndromes in China, showed that clopidogrel adds to the benefit of aspirin on CVD and total mortality but did not increase major bleeding. CURE Trial Investigators NEJM. 2001;345: 494-502 Second Chinese Cardiac Study: COMMIT Randomized, double-blind, 2x2 factorial trial of clopidogrel and metoprolol 45,852 patients within 24 hours of onset of symptoms of suspected acute myocardial infarction Randomization in clopidogrel arm to daily 75mg clopidogrel+162mg aspirin(22,960) or placebo +160mg aspirin(22,891) COMMIT Collaborative Group. Lancet 2005; 366: 1607-1621. COMMIT Clopidogrel Arm: Primary Outcomes End point Clopidogrel, n=22 961 (%) Placebo, n=22 891 (%) Odds ratio (95% P value CI) Death/MI/stroke 9.2 10.1 0.91 (0.86-0.97) 0.002 Death from any cause 7.5 8.1 0.93 (0.87-0.99) 0.03 COMMIT Collaborative Group. Lancet 2005; 366: 1607-1621. COMMIT: Major Bleeding Bleeding Clopidogrel (%) Placebo (%) Excess per 1000 p Any major bleed 0.58 0.55 0.4 0.59 COMMIT Collaborative Group. Lancet 2005; 366: 1607-1621. CHARISMA A randomized, double-blind placebo controlled trial of 15,603 patients (79% ) with established CVD and 21% with multiple risk factors designed to test whether clopidogrel should be continued beyond 1 year in addition to aspirin. All patients received daily aspirin(75-162mg) and were randomized to daily clopidogrel(75mg) or placebo Clopidogrel patients had an event rate of 6.8% and placebo patients had an event rate of 7.3%. CHARISMA demonstrated no significant benefit long term when clopidogrel is added to aspirin. Rates of severe bleeding were similar but clopidogrel patients experienced significantly higher rates of moderate bleeding. There was possible effect modification by presence or absence of prior events, a post hoc formulated hypothesis not directly tested in this trial. Bhatt DL, et al; N Engl J Med. 2006. 54: 1706-1717 ISIS-2 Investigators, Lancet, 1988 Issues with Clopidogrel Onset: 4-6 hours (after loading dose with 8 x maintenance dose) Offset: 5-7 days Variable response: 25-30% of patients achieve less than 25% inhibition of platelet activity Must undergo 2 step metabolism (CYP3A4 mediated) to active agent Binds irreversibly to P2Y12 receptor Postulated but unproven interaction with PPIs. Gurbel, PA, et al, Circulation 2003; 107:2908-2913; Laine L, Hennekens CH: Am J Gastro. Published online 11/13/09 Dose of Clopidogrel: CURRENT- Oasis7 Randomized, double-blind, 2x2 factorial trial 25,087 ACS patients (70.8% UA/non-STEMI) Clopidogrel arm: double dose (600mg then 150mg dailyx7days then 75mg dailyx22 days) vs standard dose (300mg then 75mg daily x29 days) Aspirin arm: 300-325mg daily vs 75-100mg daily x 30 days. Mehta, S et al. Am Heart J. Nov 6 2008 ; 156: 1080-1088 Clopidogrel Dose Comparison Overall, for efficacy, double-dose clopidogrel (600 loading dose + 150 for 7 days then 75 mg for 22 days) versus standard dose ( 300 + 75 for 29 days) produced no significant reduction in the primary composite of major CV events (CV death, MI or stroke) The hazard ratio of 0.95 was a weighted average of 0.85 (p=.03) among the subgroup undergoing PCI and 1.17 (p=0.14) among the subgroup not undergoing PCI Overall, for safety, using the CURRENT definitions, double dose clopidogrel produced significant increases in severe and major bleeds. Presented at ESC Congress 2009, Barcelona Spain ASA Dose Comparison ASA 300-325 mg versus ASA 75-100 mg showed no significant differences in efficacy or bleeding. Presented at ESC Congress 2009, Barcelona Spain Proton Pump Inhibitor and Clopidogrel Interaction Hennekens CH and DeMetsD: The need for large scale randomized evidence without undue emphasis on small trials, their meta-analyses or subgroup analyses. JAMA, December 2, 2009. Bhatt D, et al The COGENT trial. Presented at TCT September 24, 2009. When effect sizes are small to moderate (relative risks < 1.5 – 2.0), it is only possible to conclude whether statistical associations are valid in randomized trials with sufficient numbers of clinical endpoints and designed a priori to test the hypothesis COGENT is the only large scale randomized trial tested omeprazole versus placebo on CV events in clopidogrel users . This trial showed no significant difference in CV events (hazard ratio = 1.02, 95% confidence limits from 0.70 – 1.51) as well as a significant reduction in GI events (hazard ratio = 0.55, 95% confidence limits from 0.36-0.85). Laine L and Hennekens CH. PPI and Clopidogrel Interaction: Fact or Fiction. AJG, Published online November 13, 2009. The current totality of evidence does not justify a conclusion that PPIs are associated with clinical cardiovascular disease (CV) events among clopidogrel users, let alone support a judgment of causality. Proton Pump Inhibitor and Clopidogrel Interaction …According to US FDA November 17, 2009 New data show that when clopidogrel and omeprazole are taken together, the effectiveness of clopidogrel is reduced. Patients at risk for heart attacks or strokes who use clopidogrel to prevent blood clots will not get the full effect of this medicine if they are also taking omeprazole. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPati entsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm19078 7.htm Proton Pump Inhibitor and Clopidogrel Interaction …According to Laine and Hennekens November 13, 2009 In randomized trials, PPIs seem to decrease recurrent ulcer bleeding in patients who bled on low-dose aspirin and continue aspirin. In addition, randomized, placebo-controlled trials show that both PPIs and histamine-2 receptor antagonists decrease the development of endoscopic ulcers in lowdose aspirin users. Current consensus recommendations do not specifically address clopidogrel monotherapy, but do state that patients taking dual antiplatelet therapy should receive a PPI. Laine L and Hennekens CH. PPI and Clopidogrel Interaction: Fact or Fiction. AJG, Published online November 13, 2009. Clopidogrel and PPI: Summary In several studies, omeprazole decreases pharmacodynamic effect of clopidogrel on surrogate markers such as platelet aggregation. Studies of the other individual PPIs have not shown such effects. Some, but not all, observational studies show that patients prescribed clopidogrel have small but significant effects of all 5 PPIs on increased rates of CV events in clopidogrel users. In one randomized trial designed to test the hypothesis, clopidogrel users randomized to omeprazole have no increased risk of CV events. Despite an insufficient totality of evidence, the FDA suggests that health care providers avoid prescribing omeprazole, esomeprazole, or cimetidine to patients receiving clopidogrel. When the totality of evidence is incomplete it is appropriate to remain uncertain. If a healthcare provider chooses to heed the FDA then use one of the other PPIs (e.g., pantoprazole, rabeprazole) and separate the PPI and clopidogrel by around 14-18 hrs by prescribing the PPI before breakfast and clopidogrel at bedtime or PPI at dinner and clopidogrel at lunchtime New Oral Antiplatelet Drugs Adenosine Diphosphate-Receptor Antagonists Prasugrel Thienopyridine More rapid onset of action than clopidogrel Irreversible inhibitor of the P2Y12 receptor Ticagrelor * Cyclo-pentyl-triazopyrimidine (CPTP) More rapid onset of action than clopidogrel Reversible inhibitor of the P2Y12 receptor * Not approved by FDA Triton-TIMI 38 13,608 patients with moderate to high-risk acute coronary syndromes with scheduled PCI Randomized to prasugrel (60 mg loading dose and a 10 mg daily maintenance dose) or clopidogrel (300 mg loading dose and a 75 mg daily maintenance dose) for 6-15 months. Triton –TIMI Investigators. NEJM; 357: 2001 2015 TRITON-TIMI 38: EFFICACY and SAFETY 15 138 events Clopidogrel 12.1 Endpoint (%) CV CVDeath/MI/Stroke Death / MI / Stroke 9.9 10 Prasugrel 5 TIMI Major Non-CABG Bleeds 35 events Prasugrel Clopidogrel 2.4 HR 1.32 1.8 (1.03-1.68) p=0.03 0 0 30 60 90 180 270 Days 360 HR 0.81 (0.73-0.90) p=0.0004 NNT = 46 450 NNT = 167 PLATO Ticagrelor vs Clopidogrel in Patients with Acute Coronary Syndromes 18,624 patients with acute coronary syndromes Randomization: Ticagrelor 180 mg loading dose, 90mg BID Clopidogrel 300-600 mg loading dose, 75 mg QD All patients received ASA 75-325 mg Wallentin, L et al NEJM 2009; 361: 1045-1057 Cumulative incidence (%) PLATO: Time to first primary efficacy event (CV death, MI or stroke) 13 12 11 10 9 Completeness of follow-up 99.97% = 5 pts lost to follow-up 9.8 Ticagrelor 8 7 6 5 4 3 2 1 0 HR 0.84 (95% CI 0.77–0.92), p=0.0003 0 No. at risk Ticagrelor 11.7 Clopidogrel 60 120 180 240 300 360 Days after randomisation 9,333 8,628 8,460 8,219 6,743 5,161 4,147 Clopidogrel 9,291 8,521 8,362 8,124 6,743 5,096 4,047 Wallentin, L Presented at ESC Congress 2009 Barcelona Spain PLATO Time to Major Bleeding - Primary Safety Event K-M estimated rate (% per year) Completeness of follow-up 99.97% = 5 pts lost to follow-up 15 Ticagrelor 10 Clopidogrel 11.58 11.20 5 HR 1.04 (95% CI 0.95–1.13), p=0.434 0 0 60 120 180 240 300 360 Days from first IP dose No. at risk Ticagrelor 9,235 7,246 6,826 6,545 5,129 3,783 3,433 Clopidogrel 9,186 7,305 6,930 6,670 5,209 3,841 3,479 Wallentin, L Presented at ESC 2009 Barcelona Spain Risks Associated with ADP receptor Antagonists in Patients with ACS by Trial Schӧmig, A NEJM 2009; 361: 1108-1111 Issues in Clinical Practice Unfortunately, for healthcare providers and their patients, most patients prefer the prescription of pills to the proscription of harmful lifestyles. Double Cheeseburger, Large Fries, Jumbo Coffee.. Oh And An Aspirin -Gotta Take Care Of The Ticker Y’Know. Aspirin May Reduce Risk Of Heart Attack New Yorker Magazine. 1988. French Fries 20 years ago 210 calories 2.4 ounces Today 610 calories How many calories are ounces in6.9 these fries? Calorie difference: 400 Calories How to burn* 400 calories: Walk 2 hour 20 minutes *Based on 130-pound person. Darwinism and Risk of Cardiovascular Disease Walking the Dog A bit of cultural news ….. After a 2 year loan to the United States, David returns to Italy… …Proud Sponsors Established Risk Factors for CHD Blood cholesterol 10% = 20%-30% in CHD High blood pressure 5-6 mm Hg = 42% in Stroke = 16% in CHD Cigarette smoking Cessation = 50%-70% in CHD Body weight BMI<25 vs BMI>27 = 35%-55% in CHD Physical activity 20-minute brisk walk daily = 35%-55% in CHD Shifting Worldwide Burden of Disease 1990 All Other 25.5% 2020 Cancer 11.9% All Other 33.2% Cancer 18.0% CVD 28.4% Communicable, Perinatal, Nutritional 34.2% Communicable, Perinatal, Nutritional 15.1% CVD 33.7% Murray CJL, Lopez AD, eds. The Global Burden of Disease. Cambridge, Mass: Harvard University Press; 1996. 2005: Beijing, China vs US Beijing US Cigarette smoking in men 58% Same as 1950 Body Mass Index Weight in Kg/ Height in m2 24.8 Same as 1990 1990 – 2010: Fast Food restaurants in China 1990 2010 McDonalds 1 800 mainland 200 Hong Kong KFC – 1,900 Selected Worldwide Death Rates From CHD in Adults Aged 34 to 74 Years* Death Rate (per 100,000) Country Men Women Total Russian Federation 638 231 869 Bulgaria 353 133 486 United Kingdom 265 97 362 United States 214 87 301 Austria 223 74 297 Germany 206 72 278 France 87 20 107 Japan 57 20 77 *All values are for 1997. British Heart Foundation. Coronary Heart Disease Statistics: British Heart Foundation Statistics Database. London, England: British Heart Foundation; 2002. “We must all hang together, or assuredly we shall all hang separately.” – Benjamin Franklin July 4, 1776 GOALS OF HEALTH CARE PROVIDERS AND ACADEMIC RESEARCHERS Maximize benefit and minimize risk which is not to be confused with avoidance of risk. Make clinical decisions based on the totality of evidence not dependence on particular subgroups of particular studies. Avoid misstatements of benefit to risk ratios which may increase publicity, academic promotions and grant support in the short run but confuse colleagues and frighten patients and make it more difficult to conduct high quality research ( COX-2 inhibitors and glitazones)