Preparation of Diabetic Patient
advertisement

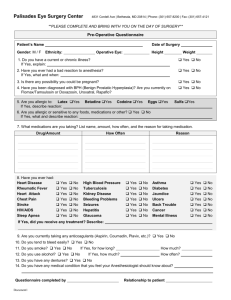
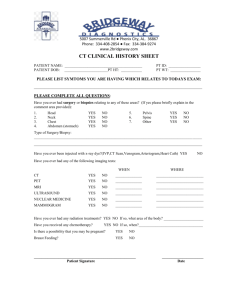
Preoperative Care By: Dr. Muath Mustafa Department of Surgery, BMC OUTLINES -Introduction: -Evaluation: -Routine preoperative measures: -The use of Antibiotic: -Prophylaxis against Deep Vein Thrombosis and Pulmonary Emboli: -Grades of Surgery: -ASA Grades: -Preparation of Hypertensive Patient: -Preparation of Diabetic Patient: Introduction: To obtain satisfactory results in surgery, a careful preoperative preparation of the patient is vital. The importance of this preparation becomes more evident as the surgical procedure performed becomes more complex. Evaluation: -Take a full history and exclude any significant medical problems (DM,HTN,COPD,Asthma). -Check clinical signs against the planned procedure, in particular noting the side involved. -Take a full drug history with specific enquiry regarding allergic responses to drugs, latex, and skin allergies. =Medications to be continued over the preoperative period: Anti HTN IHD Drugs Bronchodilators DM Medications Stop oral Warfarin (Anticoagulant) 3-4 days preoperatively and check the prothrombin time prior to surgery. If prothrombin time remains unacceptably high, the patient may require an infusion of Fresh Frozen Plasmaز Patients on Warfarin who have had a life-threatening thrombotic episode (Pulmonary Embolus) with in the previous 3 months should be switched to heparin intravenously until 6 hrs before surgery. The heparin can usually be restarted 4 hrs after surgery. =Medications to be stopped: Aspirin,Clopedogrel (Antiplatelets). Stop 48 hrs before surgery. If not stopped the patient is at increased risk of bleeding. Monoamain oxidase inhibitor. Lithium. They may interfere with anaesthitic agents. Tricyclic antidepresent Phenothiazine. Stop OCPs 4 weeks before surgery. -Take history of nutritional status. Improve if needed. -Take investigations: CBC: all patients. U & E: all patients. ECG: all patients > 40 years. Chest x-ray: all patients >30 years Liver functions: all patients. Hepatitis: ? All patients Echocardiogram: abnormal ECG, ischemic heart, heart failure. Clotting screen (Coagulation profile): anticoagulants, abnormal LFTs Calcium: Thyroid and Laryngectomy. Pulmonary functions: abnormal chest x-ray, partial Laryngectomy, Oesophagectomy. Note: Young and fit patients do not require ant preoperative investigations. Routine preoperative measures: -Each surgical procedure has a standard protocol for patient preparation. Adhere to the protocol and use a checklist; you will not leave out an important step. -Prohibit solid diet to adult patients for 6 hrs and clear fluids for 4 hrs prior to an elective general anaesthetic. Fasting time for children vary. We instruct the patient to fast to reduce the risk of pulmonary aspiration. Summary of Fasting Recommendations to Reduce the Risk of Pulmonary Aspiration: Ingested Material Clear liquids Breast milk Infant formula Non-human milk Light meal Minimum Fasting Period (hours) 2 4 6 6 6 -Operation site must be prepared by marking, and removal of hair if needed. Ask the patient to shower and clean the operation site with antiseptic solution if available. Avoid hair shaving or clipping long time before the surgery. Instead it is done at the time of surgery to avoid bacterial colonization. -Explain to the patient or guardian the procedure, and any likely complications, answer questions the patients may have, and only then have them sign the consent form. Keep in mind that operating surgeon should obtain the consent form. Seek help from a senior colleague if you are unable to answer patient`s questions. Also, consent should ideally be taken from patients not immediately before an operation but sometime ahead, so that they may have a period of reflection, and an opportunity to ask further questions that may arise -If specific services, such as frozen section histopathology, or intraoperative radiotherapy are likely to be required during the operation, organize these in advance. -Before going to the operating room: He/she will have to remove: 1. Dentures/partial plates 2. Glasses/contact lenses 3. Appliances/prosthesis 4. Makeup/nail polish 5. Hairpins/hairpiece 6. Undergarments The use of Antibiotic: -As a general rule, treat patients with clinical infection using systemic antibiotics before they undergo operation. -Antibiotic prophylaxis for an elective operation depends the procedure being performed. RISK OF WOUND INFECTION BY TYPE OF WOUND. Clean Clean-contam. Contaminated Dirty 2% 10% 20-40% All -Clean procedures, as varicose veins, do not require antibiotic prophylaxis. Abdominal operations not associated with significant contamination, such as cholecystectomy, demand only a single dose of prophylactic antibiotic given on induction of anaesthesia. -Procedures in a contaminated field, such as appendicitis, require a preoperative dose and two postoperative doses. This regimen is also satisfactory for most other gastrointestinal tract procedures, including gastric surgery, and colonic operations on prepared bowel. -The choice of antibiotic prophylaxis is determined by the surgical procedure itself. Operations potentially contaminated by skin flora require prophylaxis against staphylococcal infection with Flucloxacilline 500mg I/V. Procedures involving the bowel require broad-spectrum cover for Gram-positive and Gram-negative organisms and anaerobes. (Cephalosporine with Metronidazol). Biliary tract procedures rarely involve anaerobic contamination. Cephalosporin alone is satisfactory. Prophylaxis against Deep Vein Thrombosis and Pulmonary Emboli: Pulmonary Emboli are a major cause of mortality for surgical patients. Risk factors for DVT: Age >40 years Obesity Varicose veins High oestrogen pill Previous DVT or PE Malignancy Infection Heart failure / recent infarction Polycythaemia /thrombophilia Immobility (bed rest over 4 days) Major trauma. Risk factors for DVT: Incidence of DVT and fatal pulmonary embolism in hospital patients: Risk Low risk = Moderate risk = High risk = DVT <10% 14% 40-80% PE <0.01% 0.5% 5% Incidence of fatal pulmonary embolism in high risk patients increases 500 folds. Prophylaxis against DVT: Treatment of DVT: I/V Heparin Oral Warfarin after 3days of i/v heparin Grades of Surgery: ASA Grades: Preparation of Hypertensive Patient: -If systolic blood pressure > 160 mmhg and diastolic pressure > 110 mmhg, the elective surgery should be rescheduled. -Moderate or marked, longstanding, untreated hypertension increases perioperative morbidity and mortality, and it is significant risk factor for the production of coronary atherosclerosis. -Stabilize patients with sustained systemic arterial hypertension (systolic > 160 mmhg, diastolic > 110 mmhg) on antihypertensive therapy before proceeding with long duration elective surgery. -Untreated or inadequately treated hypertensives respond in an exaggerated manner to the stress of surgery, with resultant increase in the operative morbidity and mortality. -Assume that patients with long standing moderate to marked hypertension have coronary atherosclerosis and manage them appropriately, even in the absence of overt signs and or symptoms of ischemic heart disease. -Do CXR, ECG, treadmill test and Coronary Angiography with the possibility of recanulation of the blocked artery if needed. Preparation of Diabetic Patient: -Take a detailed history regarding the DM status, and the cardiovascular system status of the patient, and before surgery, the cardiovascular status of the patient should be reviewed. Regimes for surgery on diabetic patients Type of surgery Minor Intermediate/Major Controlled by diet No specific precautions Measure blood glucose 4-hourly, if > 12mmol start glucose-potassiuminsulin sliding scale regimen. Controlled by oral agents Omit medication on the morning of operation and start when eating normally postoperatively Omit medication and monitor blood glucose 1-2 hourly, if > 12mmol start glucose-potassium-insulin sliding scale regimen. Controlled by insulin Unless very minor procedure (omit insulin when nil by mouth) give glucosepotassium-insulin sliding scale regimen during surgery and until eating normally postoperatively. -Patient taking long-acting insulin preoperatively should be converted to Actrapid insulin, and surgery should be scheduled for the early morning if possible. -Infuse 10% glucose 500ml + 10 mmol potassium chloride (KCL) at 100 ml per hour. Prepare a 50ml syringe containing 50 units of Actrapid(Short acting) insulin in 50 ml normal saline(=1 unit per ml) and connect to a 3-way tap to a glucose infusion. Adjust the rate of the syringe driver according to the following sliding scale: Blood glucose(mmol) Rate of syringe driver (ml/h) <5 Switch off 5-7 1 2 7-10 10-20 3 >20 4 -If two successive blood glucose values are > 20 mmol, consult the duty doctor. ANY QUESTIONS?