The Febrile Infant
advertisement

Management of the
Febrile Infant
Risk Minimizers vs. Test Minimizers
Steven E. Krug, M.D.
SAEM Annual Meeting
St. Louis, MO -- May, 2002
Fever, What’s The Big Deal ?
65% of children 0-2 years visit a physician for a
febrile illness
10
to 20% of all pediatric visits to EDs
20 to 30% of pediatric office visits
Fever without a source accounts for as many
as 50% of these visits
A self limited illness in the vast majority
A small percentage will have a SBI
Occult Bacteremia in Febrile Children
How It All Began
McGowan JE, et al: NEJM 1973; 288:1309
Febrile children at Boston City Hospital
“24 hour pediatric walk-in clinic”
Temp > 38.3 0C -- all ages - 3 month study
Results:
10,535 visits 2165 children with fever
708 blood cultures 31 (4.4%) true positives
Note: 43 cultures (6.1%) produced false positives
So, Are You a Risk-Minimizer ?
Green SM, Rothrock SG: Ann Emerg Med 1999; 33:211
Desire to lower the risk of adverse sequelae
from occult infections - “ROWS”
Do not believe that clinical evaluation is
sufficient to reliably identify ill children
Use risk stratification to target higher risk
patient groups for intervention
Believe that the potential benefit of reducing
adverse sequelae justifies empiric diagnostic
testing and treatment
If Not, Perhaps a Test-Minimizer ?
Green SM, Rothrock SG: Ann Emerg Med 1999; 33:211
Believe the occurrence of adverse outcomes
is so low as to not justify time, expense and
invasiveness of risk stratification
Believe that clinical evaluation and follow up
will serve to identify nearly all ill children
Believe that parents prefer less testing and
treatment
Are willing to accept a greater chance of
being wrong
Well Intentioned Risk Minimizers at Work
Can We Identify High Risk Children ?
Demographic and clinical parameters
Lab screening profiles
age, temperature, petechiae
CBC, ESR, CRP, UA, etc.
OB/SBI risk appears to correlate with some
sensitivity, specificity and positive predictive value
for OB and SBI were less than ideal
Clinical scoring systems (McCarthy, et al.)
initially very promising, ultimately disappointing
Identification of High Risk Patients
Sensitivity of the Physical Exam
McCarthy, et al. Pediatrics 1982; 70:802
Yale Observation Score (AIOS)
incidence of SBI related to score
< 10 = 2.7%, > 10 = 40.2%, > 16 = 92.3%
sensitivity 88%, specificity 77%, low PPV
negative predictive value of normal Hx &
PE findings plus low AIOS was 96%
AIOS was fairly good in its ability to identify the sick,
but perhaps even better in identifying the well ?
Failure of Clinical Assessment
Teach SJ, Fleisher GR: J Pediatr 1995; 126:877
Prospective application of the Yale Obs. Scale
children 3 - 36 months with T > 39.0 0C
611 children in study, 192 with bacteremia
median YOS (6) was the same for both groups
YOS > 10:
sensitivity 5.2%; specificity 96.7%,
positive predictive value 4.5%,
negative predictive value 97.1%
The YOS has performed similarly in other recent studies
Social Smile & SBI
Bass JW, et al: Pediatr Infect Dis J 1996; 15:541
Do smiling febrile children have bacteremia?
512 children aged 3 to 36 months of age
T > 39.5 0C and WBC > 15,000
social smile associated with shorter fever duration
smile present in 45% of bacteremic children
smile present in 49% of non-bacteremic pts.
no demographic or laboratory differences found
between the groups
Yikes !! - So, is that a smile, or is it a grimace ?
Lessons Learned From the Search for OB/SBI
Risk Factors for OB/SBI
Age: neonates, 28-90 days, 3-36 months
Fever: OB risk increases with temperature
hyperpyrexia (T > 40.5 0C) - 8 to 25% OB
Petechiae - 15 to 20% occurrence of SBI
Immunodeficiency - e.g. HIV, SCD
WBC > 15,000; Bands > 1000
5 fold increased risk for occult bacteremia
Ill patient or toxic appearence
The big question -- Are all of these still true ??
Identification of Low Risk Patients
Physical & Laboratory Screening Profiles
Rochester Criteria
Dagan et al: J Pediatr 1985; 107:855
T > 380C, term, well appearing, secure follow-up
peripheral WBC between 5-15,000/mm3
band count < 1500 /mm3
urinalysis with < 10 WBC/hpf
no evidence of ear, soft tissue or bone infection
Performance: 233 infants 0-2 months of age
1 of 144 (0.7%) low risk infants had SBI
22 of 89 (25%) high risk infants had SBI
Identification of Low Risk Patients
Dagan R, et al: J Pediatr 1988; 112:355
Modified Rochester Criteria
added diarrhea to criteria:
if present < 25 WBC/hpf on stool smear
Performance
237 infants 0-2 months of age
0 of 148 low risk infants had SBI
21 of 88 (24%) high risk infants had SBI
So, perhaps we can identify the low risk children !
Identification of Low Risk Patients
Baker MD, et al: NEJM 1993; 329:1437
CHOP Low Risk Criteria
T > 38.20C, well appearing, low IOS
WBC < 15,000 /mm3 ; BNR < 0.2
urinalysis with < 10 WBC/hpf
CSF with < 8 WBC/mm3 & (-) gram stain
negative chest x-ray
Performance: 747 patients aged 29-56 days
64/65 patients with SBI noted as high risk
1/287 assigned to low risk had SBI
OPD assignment saved $ 3,100/patient
CHOP Low Risk Protocol: More Data
Baker MD, et al: Pediatrics 1999; 103:627
Three year study (1994-1996) at CHOP
Infants 29 to 60 days of age with T > 38.0 0C
422 infants
43 (10%) with SBI
UTI (4%); OB (2.1%); BM (1.2%); BGE (1.2%);
cellulitis (1.2%)
101 (24%) identified as low risk
no SBI in the low risk infants
Note: Over 8 years this protocol has shown a nearly perfect
100% negative predictive value for >1200 infants
Are Febrile Neonates Different
Baker M, Bell L: Arch Pediatr Adol Med 1999; 153:508
Can laboratory screening profiles reliably identify
febrile neonates with low risk for SBI ?
applied CHOP protocol to 254 infants (3 - 28 days)
43% of infants qualified for OPD management
32 infants (12.6%) with SBI
17 UTI (6.7%); 8 OB (3.1%); 4 BM (1.6%), BGE (.8%)
5 “low risk” infants had serious infections
would miss 20 infants with SBI per 1,000
Yes, febrile neonates are indeed different
Identification of Low Risk Patients
Baskin M, et al: J Pediatrics 1992; 120:22
The BCH Low Risk Criteria
T > 380C, low IOS, presence of secure follow-up
peripheral WBC < 20,000/mm3
CSF WBC < 10/mm3
urinalysis dip with (-) leukocyte esterase
all patients treated with ceftriaxone
Performance: 503 patients aged 28 -89 days
27 of 503 (5.4%) who met the criteria had SBI
9 OB (1.8%), 8 UTI (1.6%), 10 BGE (2.0%)
all were treated and were well at follow-up
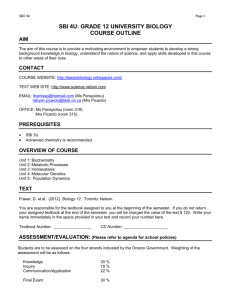
Components of Fever Protocols
Avner J, Baker MD: EMCNA 2002; 20:49
Boston
Age (days)
28-89
0
Temp ( C)
> 38.0
Infant Obs. Score
Yes
Peripheral WBC
< 20,000
CSF obtained
Yes
Antibiotic given
Yes
SBI in low risk pts (%) 5.4
NPV (%)
94.6
Sensitivity (%)
Not stated
Philadelphia
29-56
> 38.0
Yes
< 15,000
Yes
No
0
100
100
Rochester
0-60
> 38.0
No
5-15,000
No
No
1.1
98.9
92.4
Empiric Antibiotic Therapy
Does it Work?
Carroll WD, et al: Pediatrics 1983; 72:608
Small study (10 patients) - PCN vs. placebo
Difference between groups was not great
Jaffe DM, et al: NEJM 1987; 317:1175
Large multi-center study - amoxicillin vs. placebo
Enrolled 955 children 3-36 months with T > 39.0 0C
27 (2.8%) with bacteremia -- small number of cases
Outcome differences between groups were not great
Empiric Antibiotic Therapy
Does it Work?
Bass JW, et al: Pediatr Infect Dis J 1993; 12:466
Prospective study - augmentin vs. ceftriaxone
519 children aged 3-36 months -- 60 (11.6%) with OB
T > 40.0 0C - or - T > 39.5 0C and WBC > 15 K
Both Rx regimens appeared to be adequate
Fleisher GR, et al: J Pediatr 1994; 124:504
Multi-center study - ceftriaxone vs. amoxicillin
6733 patients -- 195 (2.9 %) with bacteremia
“...ceftriaxone eradicated bacteremia, had fewer
focal complications, and less persistent fever…”
Is There a Cost Effective Strategy?
Lieu TA, et al: Pediatrics 1992; 89:1135
Decision analysis, cost-effectiveness model
6 strategies for management of febrile infants
28 to 90 days with Temp > 38.0 0C
used data from literature (e.g. Baskin, Baker)
Clinical judgment alone appeared to be the least
effective clinical model and the 2nd least cost
effective strategy
Full sepsis W/U and outpatient IM ceftriaxone
was judged to be the most effective strategy
Practice Guidelines
Baraff L, et al*: Ann Emerg Med 1993 & Pediatrics 1993
Expert consensus panel recommendations
Based on meta-analysis of the literature
Fever is defined as > 38.0 0C for 0-3 months
and > 39.0 0C for 3-36 months
Infants at greatest risk during 0-3 months
Rochester criteria selected as screening criteria
for high vs. low risk
* Note: Panel members confessed risk-minimizers
Consensus Panel Guidelines
Toxic-Appearing Infants and Children
Hospitalize, evaluate and treat for presumed
sepsis, meningitis, or SBI
This holds for all age groups
THIS SHOULD BE A NO BRAINER
Consensus Panel Guidelines
Febrile (low risk) Infants < 28 days of age
Despite low probability of sepsis and studies
showing favorable outcome for outpatient
observation, the panel recommends SBI
evaluation and hospital admission for all
infants with either parenteral therapy or close
observation
Consensus Panel Guidelines
Low-Risk Infants 28-90 Days of Age
Obtain urine culture and provide close follow-up
- OR -
Full sepsis evaluation (blood, urine, CSF) and
treat with IM ceftriaxone
All
children who receive presumptive therapy
should have an LP
Consensus Panel Guidelines
Low-Risk Infants 3-36 Months of Age
Urine culture for males < 6 mo & females < 2 yrs
Stool culture if blood or mucus or > 5 WBC/hpf
Chest x-ray if decreased breath sounds or SOB
Blood culture if T > 39.0 0C and WBC > 15,000
Empiric therapy if T > 39.0 0C and WBC > 15,000
No diagnostic tests or antibiotics if T < 39.0 0C
The Febrile Infant
Variability in Management Approaches
Ros SP, et al. Pediatr Emerg Care 1994; 10:264
Surveyed members of AAP Section on EM
Numerous fever and age group definitions
74% routinely screen with a CBC
45% routinely draw blood cultures
36% use clinical appearance as basis for culturing
53% routinely administer antibiotics
44% use lab criteria as basis for antibiotic Rx
Despite published guidelines, no clear standard of care!
What Do Parents Prefer
Oppenheim PI, et al: Ann Emerg Med 1994; 24:836
Interviewed parents regarding management
options for febrile infant/child scenarios
Parents successfully identified the strategies
associated with a higher probability for an
adverse outcome
71% chose options with less testing and
treatment (and greater risk!)
So, perhaps parents are test minimizers??
What do Parents Prefer
Bennett JE, et al: Arch Pediatr Adol Med 2000; 154:43
Survey of parent utilities for outcomes of OB
convenience sample, single urban PED
94 subjects interviewed
provided with 8 possible outcomes
blood drawing viewed to be of minimal risk and
concern
Parents were intolerant of adverse outcomes
Okay, so maybe parents are risk-minimizers
Parents, Physicians & Antibiotics
Bauchner H, et al: Pediatrics 1999; 103:395
Survey of AAP general pediatricians
610 responses (67%)
40% indicated that parents frequently ask for
antibiotic when the MD feels it is not needed
48% stated parents often pressure them to
prescribe antibiotic therapy
nearly 1/3 stated they occasionally or frequently
comply with that pressure
parental pressure viewed as #1cause of the
unnecessary use of antibiotics
Risk Minimizers vs. Test Minimizers
- Published
guidelines
- “ROWS”
- Risk of OB
sequelae
- Parental
preferences
“To Test/Treat
- or Not To Test/Treat”
- Cost of care
- Changing Hx
of OB/SBI
- Risk of testing
- Risk of Rx
- Parental
preferences
Attorneys, Payors, and Other Predators
Management of the Febrile Infant
What’s Controversial, What’s Changed?
Eradication of Hemophilus influenzae
what is the current risk of OB and SBI
what is the natural history of pneumococcal OB
do the 1993 consensus guidelines make sense
Continuous blood culture monitoring systems
True efficacy of empiric antimicrobial therapy
The febrile infant with a viral infection
OB/SBI risk with hyperpyrexia; petechiae
Disappearance of H. influenzae
Prior to introduction of Hib vaccine (1987)
10-15% of OB and majority of OB related SBI
12,000 cases/yr invasive H. flu in children < 5 yrs.
33-60% develop focal infection, 15-25% develop BM
12 times more likely than pneumococcus
Currently about 300 cases per year (94/95)
no longer a leading cause of sepsis/meningitis
incidence now greatest in children < 5 months
Median age for BM: 1986 = 15 mo. 1995 = 25 yrs.
Risk of Bacteremia in the Post-Hib Era
Lee GM: Arch Pediatr Adol Med 1998; 152:624
Three year study (1993-1996) at BCH*
Children aged 3 - 36 months with T > 39.00C
11,911 patients
75% received CBC, 74% had blood cultures
149 positive blood cultures (1.6%)
92% pneumococcal
no H. influenzae isolates!!
*Is BCH the center of the risk-minimizer universe ?
Bacteremia in Boston
Lee GM: Arch Pediatr Adol Med 1998; 152:624
Prevalence greatest in 6 - 24 month age group
WBC and absolute neutrophil counts were the
most accurate predictors for bacteremia
OB risk associated with temperature
WBC > 15 x 109 -- {Sens. = 86%, Spec. = 77%}
attributed to higher WBC with pneumococcal OB
OR: > 40.0 =1.9; > 40.5 = 2.6; > 41.0 = 3.7
Lower OB rate not explained by Hib vaccine
Outcome of Pneumococcal Bacteremia
Bachur R, Harper MB: Pediatrics 2000; 105:502
Re-evaluation of children in ED with OPB
Nine year study at BCH (1987-96)
548 episodes of OPB
40 (7%) with PB or new focal infection
14 PB(2.5%); 8P(1.5%); 8M**(1.5%);
6C(1.0%); 4 PC(0.7%)
patients not initially Rx, and those treated who
remained febrile were are greatest risk for PB
majority with OPB can be managed as outpatients
** Three diagnoses/cases of BM were controversial
Persistent Bacteremia/Meningitis in OPB
Bachur R, Harper MB: Pediatrics 2000; 105:502
Rx Group
N__
__PB___
NoAntibx
68
19 (28%) 1 (1.5%)
OrAntibx
208
11 (5%)
2 (1%)
PaAntibx 195
10 (5%)
2 (1%)
TOTAL
40 (8%)
5 (1%)
471
BM__
Prevalence/Outcome of Occult Bacteremia
Alpern ER, et al: Pediatrics 2000; 106:505
Three year retrospective study (1993-1996)
Prevalence of OB = 1.9%
83% pneumococcal; H. influenzae not isolated
Focal bacterial infections in 17 (0.3%)
5900 children aged 2-24 months, T > 39.0
pneumonia (8), cellulitis (4), osteo (2), others (3)
Serious adverse outcome in 2 (0.03%)
meningitis (1), sepsis/death (1)
Note: 96% OB with spontaneous resolution without Rx
Occult Bacteremia in Philadelphia
Alpern ER, et al: Pediatrics 2000; 106:505
Mean time to culture shorter for true positives
mean times: true (+) = 14.9 hrs; false (+) = 31.1
< 18 hours 13x more likely to be true pathogen
Nearly all true positives re-evaluated in ED
average time from notification 10.6 (+ 9.7) hrs
33% were still febrile
53% admitted to the hospital
4.8% found to have persistent bacteremia
oral antibiotics Rx at 1st visit did not affect rate of PB
Perhaps blood cultures can be an effective screen?
Prevalence/Outcome of False (+) Blood Cultures
Alpern ER, et al: Pediatrics 2000; 106:505
Overall contamination rate was 2.1%
85% were re-evaluated in ED
35% were still febrile and were admitted
1.9% of repeat cultures also contaminated!
At least in Philadelphia, the risk of a contaminated blood
culture equals or exceeds that of a true positive !
Remember the data from McGowan, 1973?
Prevalence of False (+) Blood Cultures
Alpern ER, et al: Pediatrics 2000; 106:505
Age
(Months) N__
OB Rate
False + Rate
(95% CI)____ (95% CI)____
2-5
728
1.0% (0.4-2.0) 3.6% (2.3-5.2)
6-11
2181
1.8% (1.3-2.4) 1.8% (1.3-2.5)
12-17
1722
2.3% (1.6-3.1) 1.8% (1.2-2.5)
18-24
1270
2.0% (1.3-3.0) 2.0% (1.3-3.0)
Use of Antibiotics to Prevent SBI
Bulloch B, et al: Acad Emerg Med 1997; 4:679
Meta-analysis of published RCCT’s
Antibiotic use trended to risk for SBI
4 studies: Carroll, Jaffe, Fleisher, Bass
odds ratio = 0.60 (P.O.) & 0.38 (I.M.)
need to treat 414 kids to prevent 1 SBI case
no significant effect of antibiotic therapy
Concluded that widespread antibiotic use
should not replace clinical judgement
Outcomes in Occult Bacteremia
Bulloch B, et al: Acad Emerg Med 1997; 4:679
Study
Occult Bacteremia (n) Serious Bacterial Infections
Carroll, et al.
5 in IM + PO PCN
5 in no antibiotic
None
2 meningitis
Jaffe, et al.
19 in PO amoxicillin
8 in placebo
1 periorb. cellulitis, 1 bacteremia
1 persistent bacteremia
Fleisher, et al. 76 in PO amoxicillin
Bass, et al.
71 in IM ceftriaxone
3* meningitis, 1 septic arthritis,
1 sepsis, 1 pneumonia
2** meningitis, 1 osteomyelitis
22 in PO augmentin
38 in IM ceftriaxone
3 pneumonia
None
Does empiric therapy truly reduce the risk for SBI?
Predictors of Pneumococcal Bacteremia
Kuppermann N, et al: Ann Emerg Med 1998; 31:679
With invasive H. influenzae infections out of the
picture, are there unique predictors for OPB
Multivariate analysis - 6,500 children 3-36 months
164 children (2.5%) with OPB
Three variables retained association with OPB
ANC: OR of 1.15 for each 1,000 cells/mm3
if ANC > 10,000 -- OPB rate 8.2%
temp: OR of 1.77 for each 10 C
age < 2 years: OR of 2.43 vs. 2-3 years of age
Band Counts in Young Febrile Children
Kuppermann N, et al: Arch Pediatr Adol Med 1999; 153:261
Compared CBC findings in febrile children
with a documented SBI (bacteremia or UTI)
versus a proven respiratory viral infection
Children with SBI had a greater mean ANC
11.3
x 109 vs 5.9 x 109
No differences in percentage band count or
absolute band count between the groups
Identification of Children with
UMD
Kuppermann N, et al: Pediatrics 1999; 103:e20
Clinical/hematologic features of children with
unsuspected meningococcal disease (UMD)
retrospective, four center study,1985-96
381 children with meningococcal disease
45 (12%) with UMD [discharged home !!]
compared to 6400 culture negative children
no difference in Temp, WBC, ANC
significantly higher band counts in UMD
predictive value of band count was low (PPV 0.06%)
Bad news… There is still no crystal ball for UMD
Febrile Children with Bronchiolitis
Kuppermann N: Arch Ped Adoles Med 1997; 151:1207
Evaluated risks of bacteremia and UTI in febrile
children with/without bronchiolitis
432 children aged 0-24 months
Children with bronchiolitis had significantly
fewer positive cultures
blood 0% vs. 2.7%; urine 1.9% vs. 13.6%
none of the children < 2 months of age with
bronchiolitis (36) had bacteremia or UTI
SBI Risk in Children With
Recognizable Viral Syndromes
Greene DS, Harper MB: Pediatr Infect Dis J 1999;18:258
Five year retrospective study (1993 -1998)
Children aged 3-36 months with T > 39 0C
1347 children diagnosed with a “RVS”
croup, varicella, bronchiolitis, stomatitis
blood cultures obtained in 65%
2 of 876 (0.2%) blood cultures were positive
Office-based physicians have known this for a very long time.
Bacteremia in Fever & Petechiae
Mandl KD, et al: J Pediatr 1997; 131:398
Prior studies suggest a high risk for bacteremia
7 to 11% incidence of meningococcemia
Enrolled 411 children -- (58% 3-36 mo.)
8 (1.9%) with bacteremia or clinical sepsis
six with serious invasive bacteremia
none of 357 well-appearing children had OB
toxic appearance had sensitivity of 100%
WBC > 15 K or < 5K had sensitivity of 100%
all children with meningococcemia had purpura
Occult Pneumonia in Febrile Children
Bachur R, et al: Ann Emerg Med 1999; 33:166
What is the incidence of occult pneumonia in
febrile children with high WBC ?
Prospective cohort ED study
age < 5 years, T > 39 0C, WBC > 20,000
radiographs obtained in 225 of 278 patients
positive radiographic findings in
40% of those with a suggestive clinical exam
26% of those without clinical evidence for pneumonia
recommends empiric chest radiography
UTI’s in Febrile Infants
Shaw KN, et al: Pediatrics 1998; 102:e16.
UTI is by far the most frequent SBI
fever may be only presenting sign of UTI
What is the prevalence of UTI in febrile infants
2400 febrile infants -- overall 3.3%
gender -- male: 1.8%; female: 4.3%
race -- white: 10.7%; AA: 2.1%; others: 5.7%
other source -- yes: 2.7%; no: 5.9%
temperature -- < 39.0: 2.2%; > 39.0: 3.9%
Should we screen all febrile children for UTI ?
UTI’s in Febrile Children
Gorelick, Shaw: Arch Ped Adol Med 2000;154:386.
Developed clinical decision rule []
T > 39.0 0C
fever > 2 days
white race
age < 1 year
absence of another potential source
All with UTI had at least one risk factor
Presence of any two factors
sensitivity 95%, specificity 31%
Rule eliminated 30% of unneeded cultures
Risk of SBI in Febrile Seizures
Trainor J, et al: Clin Pediatr Emerg Med 1999; 1:13
Multi-center study of ED management of
simple febrile seizures (Chicago, 1998)
455 children with febrile seizure
1.3% with bacteremia
5.9% UTI
12.5% with abnormal chest x-ray
normal CSF in all who had an LP (135)
Meningitis Risk in Simple Febrile
Seizures: What’s Been Reported ?
Literature review of reported cases of febrile
seizures and meningitis
2,870 cases of febrile seizures with LP’s
1.7% with bacterial meningitis
17% of those with meningitis described as
clinically inapparent
Is occult bacterial meningitis a significant
clinical entity ?
Meningitis Risk in Febrile Seizures
Green SM, et al: Pediatrics 1993; 92:527
Studied children with meningitis -- how many
presented solely with seizures?
486 children with bacterial meningitis
complex seizures present in 79%
93% of those with seizures were obtunded
of the few with “normal” LOC, 78% had nuchal rigidity
the two patients without meningismus had
other straightforward indications for LP
Occult meningitis is more myth than fact
What is the Cost Effective Strategy?
Yamamoto LG, et al: Am J Emerg Med 1998; 16:193
Updated decision analysis which considered:
low incidence of H. influenzae infections
emergence of resistant S. pneumoniae
negative consequences of unnecessary Rx
Assuming zero or low Rx consequences -empiric therapy associated with best outcomes
Assuming realistic Rx consequences - no
testing and no treatment option may be best
Cost Effectiveness Post-Vaccine?
Lee GM, et al: Pediatrics 2001; 108:835
Updated prior decision analysis, considering:
Elimination of H. influenzae
Lower rate of occult bacteremia (1.5%)
Published efficacy of empiric Rx
Negative consequences of unnecessary Rx
At current rate of OB, CBC plus selective blood
culture and treatment is still best
If OB rate < 0.5%, strategies employing empiric
testing & treatment should be eliminated
Serotyping of Pneumococcal OB
Alperin ER, et al: Pediatrics 2001; 108:e23
What is potential efficacy of pneumococcal
vaccine in the prevention of OB
S pneumoniae accounts for the vast majority
(83%) of pathogens in children with OB
Eight serotypes isolated:
6A, 9V, 19F, 18C, 4, 6B, 23F, 14
98% of serotypes would be covered by the
currently licensed vaccine -- all except 6A
Good news…We may soon erradicate OPB
Food For Thought And A Little Math
Current risk of OB: 1.5 to 1.9%
92% pneumococcal
Risk of meningitis in OPB: 1 to 2%
Risk of adverse sequelae in BM: 33 - 50%
Need to treat 2500 febrile kids to prevent one
case of BM; 5000-7500 per adverse sequelae
remember that antibiotics may not prevent BM!
incidence of ADR’s: 150 - 600(?)/ case of BM
alarming growth rate of antibiotic resistance
Evolving Pneumococcal Resistance
Kaplan, et al: Pediatrics 1998; 102:538.
Prospective surveillance study of invasive
pneumococcal infections
three year (1993-1996), eight center study
1291 systemic pneumococcal infections
Proportion of non-susceptible isolates (PCN,
ceftriaxone) increased annually
nearly doubled over the three year period
penicillin resistance 21%
ceftriaxone resistance 9.3%
So, What Do We Actually Know
Extremely common presenting complaint
Much concern (phobia?) regarding fever
Fairly effective strategies to identify low risk
infants - these do not apply to neonates
#1 bad actor (H. flu) effectively erradicated
UMD - “pediatrician’s nightmare” - still out there
Risk of OB, now under 2%, primarily OPB
Can apply risk stratification to OPB
93-96% spontaneous resolution of OPB
So, What Do We Actually Know
No consensus regarding optimal approach
to the febrile infant
Not entirely clear what parents want
Empiric Rx does not prevent sequelae
Rising rates of antimicrobial resistance
UTI remains the most common occult “SBI”
RVS are a reasonable explanation for fever
Pneumovax may make this all a moot point
Some Friendly Advice
Keep abreast of the literature
Discuss this with colleagues & mentors
local practice variations
institutional practice guidelines
antimicrobial resistance rates
Both approaches (RM & TM) are defensible
Choose the best strategy for you
Be consistent
Always treat the ill appearing child with fever
Notable Quotes
“Unfortunately, many practitioners have become
reluctant to rely on clinical judgement, preferring
diagnostic tests and frequent use of antibiotics.”…….
“We should resist the urge to use antibiotics
empiricially, especially in a patient who looks well, for
whom antibiotics have not been shown clearly to be
beneficial”
-- JK Stamos, ST Shulman: Lancet 1997
“Antibiotics are not antipyretics”
-- SE Krug: Overheard many evenings in CMH ED