SIRS and the Septic Response
advertisement

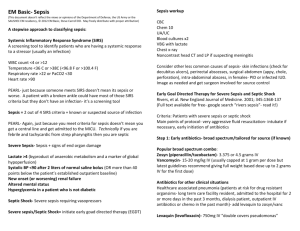
SIRS and the Septic Response Manoj Sayal, MD FRCSC March 5, 2008 Agenda 1. 2. 3. 4. A brief review of SIRS (systemic inflammatory response syndrome) SIRS and it’s role in sepsis Definitions of the sepsis syndrome Current sepsis guidelines Case 1 67yo male, presents to ER with 2 day history of N+V, abdo pain In ER, looks unwell: HR 130, BP 80/60 RR 36 SPO2 84% on room air; supplemental O2 applied, sats increase to 92% Diffusely tender abdomen, coarse air entry bilaterally What now? Case 1 2 large bore IV’s—normal saline 1 litre Labs drawn CXR (portable), EKG, ABGs Diagnosis? Case 1 CXR: RLL infiltrate WBC 22.4 Hb 108 Pl 98 Lytes normal; transaminases normal Amylase 700 What now? Case 2 Same patient, but normal amylase Case 3 Same patient but involved in a major house fire, normal amylase What’s wrong with each of these patients? Does their management differ significantly (initially)? They are all manifesting evidence of the SIRS response SIRS for Dummies (or Surgeons) Dysregulation of the normal response with massive and uncontrolled release of proinflammatory mediators creating a chain of events that leads to widespread tissue injury Results in MODS (Multiple Organ Dysfunction Syndrome) that causes the extremely high morbidity and mortality in this situation SIRS SIRS is a clinical diagnosis, recognized by 2 or more of the following (in the appropriate setting): 1. 2. 3. 4. Temp >38ºC or <35ºC HR>90bpm RR>20bpm or PaCO2<32mmHg WBC>12, <4 or >10% immature (band) forms SIRS Causes Acute pancreatitis, autoimmune disorders, vasculitis, thromboembolism, burns, surgery, pulmonary contusion, SEPSIS) SIRS How does this relate to infection or the response to infection? Definitions Infection an inflammatory response to microorganisms or the invasion of normally sterile host tissue by these organisms Bacteremia viable bacteria in the blood Definitions Sepsis In sepsis, clinical signs of SIRS are present and are due to either a culture proven infection or a suspected infection Clinical syndrome that complicates severe infection and represents the systemic response to the infection Definitions Severe Sepsis Sepsis plus at least one of the following: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Areas of mottled skin Capillary refill > 3 seconds Urine output < 0.5cc/kg/hr for at least one hour or renal replacement therapy Elevated lactate (>2 to 3) Abrupt change in mental status Abnormal EEG findings Platelet count <100, 000 DIC ARDS Cardiac dysfunction Definitions Septic Shock Severe sepsis plus at least one of the following: 1. 2. MAP<65mmHg despite adequate fluid resuscitation Maintaining MAP>60-65mmHg requires vasopressors: • • • Dopamine > 5μg/kg/min Norepinephrine < 0.25μg/kg/min Epinephrine < 0.25mg/min Definitions Refractory Septic Shock Septic shock that requires higher doses of the ionotropes to keep the MAP>65mmHg: Dopamine > 15μg/kg/min Norepinephrine > 0.25μg/kg/min Epinephrine >0.25mg/min Definitions Multiple Organ Failure/MODS Presence of altered organ functions in an acutely ill patient such that homeostasis cannot be maintained without intervention Primary: secondary to a well defined insult in which organ dysfunction occurs early and can be directly attributable to the insult itself (eg ARF from rhabdomyolysis) Secondary: organ failure not in direct response to the insult itself but as a consequence of a host response to the insult (eg ARDS in pancreatitis) Definitions Note that NO positive blood cultures are needed in the definition You only get positive cultures in 17-69% of all septic/septic shock patients Sepsis Getting more frequent (increasing by 8% per year since the 1970’s) with increasing severity 2% of all hospitalized patients Up to 75% of all ICU patients 20-50% mortality, depending on the degree: SIRS alone 7% Sepsis 16% Severe sepsis 20% Septic shock 46% Rangud-Feausto, MS et al, JAMA 1995; 273:117 Sepsis Characteristics that influence outcome in the septic patient include: Host response: is the host able to mount a fever or WBC response? Underlying disease: comorbidities (NIDDM, kidney failure, hepatic failure, cancer, EtOH abuse, immune suppression) APACHE II score Advanced age Site of infection: Lung/gut 50% Urine 30% Community acquired vs healthcare acquired Organism involved Antibiotics—timing and type Rapidity and adequacy of response Sepsis--Pathogenesis Pathogenesis Process of malignant intravascular inflammation Uncontrolled, unregulated, self-sustaining Exaggerated response of the normal inflammatory response Sepsis--Pathogenesis When tissue is injured, or infected, there is the simultaneous release of proinflammatory and antiinflammatory elements—the balance of these helps facilitate tissue repair and healing Remote tissue injury may ensue when this equilibrium in the inflammatory process is lost and these mediators exert systemic effects Sepsis--Pathogenesis The significant consequences of a systemic proinflammatory reaction include endothelial damage, microvascular dysfuntion, impaired tissue oxygenation and subsequent organ damage or injury The consequences of an excessive antiinflammatory response include anergy and immunosuppression Sepsis--Pathogenesis Normal inflammation involves the regulation of PMN rolling, adhesion, diapedesis, chemotaxis, phagocytosis and killing of invading bacteria These processes are highly controlled through proinflammatory and antiinflammatory cytokines released by activated macrophages Sepsis--Pathogenesis As a result of dysregulation of this process, an autodestructive process ensues to involve otherwise remote normal tissue and results in the sepsis syndrome Sepsis--Pathogenesis This involves many factors: Proinflammatory cytokines (TNFα, IL-6 etc) Bacterial factors—direct effect of invading microorganisms or their toxic products: Endotoxin (gm neg bacteria) Cell wall components (peptoglycans, muramyl dipeptide, lipoteichoic acid) Enterotoxins (staph), exotoxin (pseudomonas), M protein (GAS), toxic shock toxin etc Complement activation (C5a) Sepsis--Pathogenesis This results in cellular injury and subsequent organ dysfunction The precise mechanism is not known, but proposed mechanisms include: Cellular ischemia (O2 lack relative to need) Direct cell injury by inflammatory mediators and other products of inflammation Increased rate of apoptosis (programmed cell death) Sepsis--Pathogenesis If the mediators balance each other out and the initial infectious insult is overcome, homeostasis will be restored The initial insult may be so severe that it directly induces SIRS and MODS In most patients, a balance is not established and one of the 2 predominates Specific Organ Involvement Circulation Derangement in metabolic autoregulation occurs (process that matches O2 availability to need) Vasoactive mediators are released that cause microvascular permeability and vasodilation (prostacyclin and NO) Impaired compensatory secretion of ADH (vasopressin) may also contribute Circulation In central circulation, early manifestations include changes in systolic and diastolic ventricular function Initially, CO increases to compensate for the vasodilation until the patient is no longer able to do so Circulation In the regional circulation, there is heterogeneity in normal distribution of blood flow and loss of regulation The microcirculation is a key (if not the most important) target organ for injury in the sepsis syndrome There is a decrease in the number of functional capillaries which causes an inability to extract O2 maximally Circulation Panendothelial activation leads to widespread tissue edema, which is rich in protein Hypotension is the most serious expression of the circulatory dysfunction that results (reduced arterial tone, increased permeability) Other changes include venous dilatation (decreasing venous return to the heart) and the release of myocardial depressant factors Lung Endothelial injury leads to disturbed capillary blood flow and enhanced microvascular permeability and subsequent interstitial and alveolar edema PMN entrapment amplifies this damage ALI/ARDS GI Tract May provided positive feedback loop in injury from sepsis from various sources: Bacterial overgrowth in UGI tract leading to VAP if patients not fed or prophylaxed Translocation through gut wall of bacteria from circulatory abnormalities depressing the gut’s barrier funtion Liver Liver dysfunction can worsen sepsis by preventing bacterial clearance Can get reticuloendothelial system dysfunction from the sepsis syndrome Increased LFT’s/transaminases Kidney ATN (systemic hypotension, direct renal vasoconstriction, cytokine release etc may all cause) Likelihood of death increases dramatically if renal failure accompanies sepsis Nervous System CNS: altered sensorium PNS: peripheral neuropathy Limb muscle weakness and atrophy Reduced DTR’s Loss of peripheral sensation to light touch and pin prick Preservation of cranial nerve function Blood Thrombocytopenia DIC Hyponatremia Anemia Elevated or decreased WBC Treatment Try to get the patient back to homeostasis as quickly and safely as possible Fluid is your best ionotrope…do not be afraid of it “Hit them early, hit them hard” Treatment Early Goal Directed Therapy in the Treatment of Severe Sepsis and Septic Shock Emmanuel Rivers, NEJM 2001 Treatment Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2008 Crit Care Med 2008 Vol 36 No 1 Treatment Initial resuscitation (within first 6h) Begin resuscitation immediately in patients with hypotension or elevated lactate (>4)—do not delay until pending ICU admission Resuscitation goals CVP 8-12 mmHg MAP >65 mmHg U/O > 0.5ml/kg/hr SVC O2 sat >70% If venous O2 sat not achieved, consider futher fluid, PRBC (to keep Hct >30%) or dobutamine Treatment Diagnosis Obtain appropriate cultures providing it does not delay antibiotic administration 2 or more BCs One BC from each access device >48hr old Other sites as indicated Treatment Antibiotics As early as possible and always within 1hr Broad spectrum, covering all likely pathogens then narrow as clinically indicated Stop if not infectious cause, otherwise 710 days Treatment Source Control Identify anatomic site of infection as soon as possible (within 6hr of presentation) Choose source control with max efficacy and min physiologic upset Remove all intravascular devices if potentially infected Treatment Fluid Therapy Crystalloid or colloid Use fluid challenge technique while associated with hemodynamic improvement 1000cc crystalloid or 300-500cc colloid over 30 mins Rate of fluid administration should be reduced if cardiac filling pressures increase without concurrent hemodynamic improvement Treatment Vasopressors Maintain MAP > 65mmHg Norepinephrine or dopamine initially Then can add epinephrine or vasopressin Art line when practical No low-dose dopamine for renal protection Ionotropes Dobutamine in patients with depressed myocardial function Treatment Steroids Low dose in patients who respond poorly to fluids and vasopressors No ACTH stim test needed Use HC with or without FC Stop once patient is off vasopressors Treament Activated Protein C Consider in patients with sepsis induced organ dysfunction and high risk of death (APACHE II >24 or MODS) if there are no contraindications Treatment Blood Product Administration Give RBC if Hb < 70 to target 70-90 Do not use FFP unless there is bleeding or planned invasive procedures Give platelets when counts are <5000, or between 5000 and 30000 and there is significant bleeding risk Treatment Mechanical Ventilation Lung protective strategies, using ARDSnet guidelines SBT’s once patient ready for them HOB at 30-45 degrees Treatment Others Sedation as necessary DVT/Stress ulcer prophylaxis Glucose control (keep 5-8.3) Summary A large and diverse topic Will be a common occurrence in any surgical practice Needs to be recognized and dealt with quickly to minimize morbidity and mortality Treatment