of the Knee Joint
advertisement

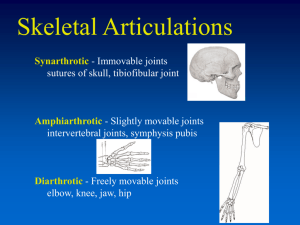
Osteoarthritis of the Knee Joint Ali Legnos Friction and Wear of Materials Fall 2012 1 1. Background The knee joint is a subject of much biomechanical and tribological study. This joint bears on average 3.9 times the individual’s body weight while walking on level ground1, and with daily use and age, the lubricating cartilage and fluid protecting bones in the knee can thin due to fatigue wear. When partial or complete of erosion of the cartilage occurs and bare bones come into contact, a degenerative disease called Osteoarthritis will result. Bone spurs can develop at the joint causing pain and can leave patients bedridden. There is currently no cure for Osteoarthritis.2 Extreme cases of Osteoarthritis of the knee require Total Knee Replacements (TKRs), or Total Knee Athroplasty (TKA), in which the damaged bone and cartilage is removed and replaced by a prosthetic. Prostheses are typically made of metal covered with polyethylene plastic.3 A normal knee compared to a knee with TKR joint is shown in Figure 1. Figure 1 Normal Knee (Left) and Knee with TKR (Right)4 Understanding the friction, wear and lubrication of the knee joint is a complex problem, requiring understanding of the anatomical make-up of the joint and what factors influence 2 and are affected by friction and wear on the contacting surfaces. There is a plethora of research on several aspects of the knee joints, including but not limited to its biomechanics; friction, wear and lubrication properties; and prosthesis design and modes of failure. The focus of this research is to provide an overview of the anatomy of the knee joint and present a compilation of recent scientific and engineering conclusions relating to a) factors that affect wear of the knee joint, and b) methods commonly used to measure friction, wear and lubrication of the joint. 1.1. Knee Anatomy The knee joint consists of the intersection of bones protected by lubricating films of cartilage, and surrounded by a lubricating fluid called synovial fluid. A brief overview of the anatomy of the knee is provided below. 1.1.1. Knee Bones The knee joint is the intersection of three bones: the femur (thigh bone), tibia (shin bone) and patella (knee cap), as shown in Figure 2. The tibiofemoral joint is a hinge joint connecting the tibia to the femur. The patellofemoral joint is a saddle joint connecting the patella to the front of the head of the femur bone. 3 Figure 2 Normal Knee Joint, Side View5 1.1.2. Articular Cartilage Articular cartilage is smooth tissue that covers bones where they intersect other bones at joints. It functions as a low friction surface to protect the bones from the compressive forces on the knee during joint movement. With use, articular cartilage can gradually wear thin, decreasing the protective lubricating layer over the bone. In extreme cases, articular cartilage will wear away completely at a given location on the joint and the bones will come into direct contact, as shown in Figure 3. Since cartilage is not regenerative, once it is worn away surgical options, such as inserting prostheses, are often employed.6 4 Figure 3 Knee Osteoarthritis7 The heads of the femur and of the tibia located at the knee joint are covered by a layer of articular cartilage, as shown for a healthy knee in Figure 2 and in a knee with Osteoarthritis in Figure 3. The underside of the patella is also protected by a layer of cartilage. The tensile modulus of cartilage will decrease with age and wear, decreasing the elasticity of the material in the plastic deformation regime. Wear will also lead to a reorganization of fibers present in the cartilage, which can result in split-lines and wearlines on the surface of the cartilage.8 1.1.3. Synovial Fluid Synovial fluid is a viscous substance located in synovial joints, such as the knee, that acts as a lubricating agent to reduce friction. It is found in the cavity surrounding the heads of the tibia and femur, and the patella, as shown in Figure 2. Synovial fluid has a high concentration of hyaluronic acid, whose high molecular weight and long coiled molecules give synovial fluid high elasticity and viscosity. 9 The molecular weight and concentration of hyaluronic acid are responsible for the boundary layer phenomena at the 5 synovial fluid-articular cartilage interface. It is the “stickiness” of the boundary layer that is theorized as to why synovial fluid is an effective lubricant10, but overall, lubrication measurements of synovial fluid are varied and poorly understood.11 2. Factors Affecting Knee Joint Wear Understanding joint kinematics and the properties of bone, cartilage and synovial fluid are crucial to understanding the tribological environment of the knee joint. Articular cartilage and synovial fluid act as lubricants for the bone and achieve low friction in healthy joints. Loading on the joint, including maximum and normal sustained loading must be understood for the various conditions a human knee is subject to, and the compressive and shear forces calculated appropriately. Williams et. al. summarized the unique factors contributing to friction, wear and lubrication of a synovial joint, such as the knee, in Figure 4.12 Figure 4 Key Challenges for Synovial Joint Tissue Engineering 6 Several macro scale factors have been hypothesized to influence the location and degree of wear on the knee joint, including age, sex, height, weight, genetics and positional alignment of the leg bones. 2.1. Weight, Body Mass Index, Gender and Age Several studies have been performed to correlate a patient’s weight, Body Mass Index (BMI), gender and age to stress on the knee and the onset and severity of Osteoarthritis. Being overweight and/or having an elevated BMI put an increased stress on the knee joint, and are generally agreed to be a significant factor in the onset of Osteoarthritis of the knee due to an increased load on the joint. An explicit BMI has not been identified as a cut-off value to separate high-risk from low-risk individuals.13 Some studies have cited that females have increased wear of the knee joint, leading to higher incidences of Osteoarthritis diagnoses than in men, and/or more severe symptoms, while other studies have shown only weak correlations. One study noted that females on average have greater knee flexion and knee extensor movement, which is a factor in the onset of Osteoarthritis.14 Another study found that women showed worse Osteoarthritic symptoms then men.15 2.2. Knee Bone Alignment Studies have indicated that misalignment of the bones at the knee joint can lead to accelerated wear on the joint. Ding et. al. found that the degree of tibial varus, or degree of rotation of the tibia in the direction of the body’s centerline (i.e. bowlegged) with respect to the femur, is highly correlated to knee joint wear.16 Srivastava et al. studied 7 the correlation of tibial varus to articular cartilage wear. The surface geometry of sixteen polyethylene tibial prosthetic inserts that had been removed from patients’ knees were compared to unused prostheses using a laser displacement sensor with a resolution of 3 μm. Surgical techniques aim for tibial insert alignment at 90 degrees to the sagittal plant, with a tibial varus of 2 to 3 degrees often achieved with surgical tools. The results indicated a strong correlation between the tibial varus and wear volume of the prosthetic insert, indicating twice the volumetric wear on prostheses with greater than 3 degrees of varus compared to those with less than 3 degrees of varus.17 3. Wear Measurement Techniques Observations of cartilage wear on the knee joint can be accomplished by direct measurement using Magnetic Resonance Imaging (MRI) and x-rays. India ink is commonly used to measure the surface roughness of articular cartilage. Additionally, material properties have been estimated for the bones, cartilage and synovial fluid, and computer simulations have been developed to predict wear. 3.1. Magnetic Resonance Imaging Direct measurement of an individual’s knee, including bone volume and cartilage thickness, is readily measured using MRI. Subsequent measurements can indicate a loss of cartilage volume, or the volumetric wear. Scales have been developed and published to standardize the measurement of cartilage wear. The Whole-Organ MRI Score (WORMS), shown in Table 1, classifies the location and severity of cartilage wear on a joint.18 8 Table 1 Whole-Organ MRI Score (WORMS) Connolly et. al. measured cartilage thickness on the tibia and femur in the tibiafemoral joint and calculated average values. MRI of 20 patients were drawn in CAD and analyzed. The study concluded that the average femoral articular cartilage thickness is 2.75 mm and the average tibial articular cartilage thickness is 2.76 mm, and showed a strong correlation between cartilage thickness and the patients’ height and weight. 19 Similarly, Iranpour et. al. generated CAD models of 37 patellae with articular cartilage based on x-ray images. They found the average patellar thickness to be 2.5 mm.20 3.2. Surface Geometry Using India Ink With age and wear, the tensile strength of articular cartilage of the knee experiences a decrease in tensile strength, as much as 65% between the ages of 24 to 90. Cartilage deterioration results from a degradation of extracellular matrix components and modification of the collagen network through crosslinks. 21 Covering the surface of 9 articular cartilage with India Ink is a common method of visually inspecting the cartilage surface to assess the extent and location of wear. An individual particle of India Ink is approximately 40 nm in diameter, and particles clump in groups approximately 100 nm in diameter. These large diameters do not permit the India Ink from penetrating and permanently staining healthy cartilage, but staining may occur in protein deficient areas of the cartilage. The amount of light reflection and surface pattern are used to visually inspect the location and amount of cartilage erosion.22 3.3. Modeling Techniques Data gathered from physical models, either using India Ink or MRI images, and cadavers is often modeled using CAD and analyzed using finite element methods. Such models are often used to measure contact stresses and strains, which are difficult to measure in vivo. Computation simulations are often employed as a low cost and non-invasive option.23 Li et. al. tested a cadaver of the femur and patella bones and their articular cartilage, and generated a CAD model of the cadaver geometry, as shown in Figure 5. Both experimental setups underwent the same series of loading to simulate wear due to fatigue, and it was found that wear depths measured in the computer simulation were within 0.01 mm accuracy to the cadaveric experiment. An experimental limitation was identified as the difference in wear between living articular cartilage and dead cartilage on the cadaver. Archard’s wear law is appropriate for use on the dead cartilage, but the need for a validated wear law for cartilage was expressed.24 10 Figure 5 Li et. al. Cadaver and CAD Models Used to Compare CAD Model Accuracy25 4. Conclusions Understanding the anatomical and physiological aspects of the knee joint is imperative to improving the diagnosis, and possible prevention or cure of Osteoarthritis. There are several factors, many currently disputed in the scientific community, affecting the amount and location of wear on the tibia, femur and patella, including age, sex, weight, genetics, alignment of the knee bones, etc. Understanding these factors will help doctors diagnose severe cartilage wear prior to a diagnosis of Osteoarthritis, and hopefully better prepare the population to prevent or cure the disease. “Knee Joint Considerations in Total Knee Replacement”; Kuster, Marcus S; Wood, Graeme A.; Stachowiak, Gwidon W.; Gachter, Andre; University of Western Australia, January 1997, http://www.bjj.boneandjoint.org.uk/content/79-B/1/109.full.pdf 2 “Osteoarthritis”, Mayo Clinic, http://www.mayoclinic.com/health/osteoarthritis/DS00019 3 “Knee Joint Replacement”, Biomet, http://www.biomet.com/patients/knee_replacement.cfm 1 11 “Knee Replacement”, Medline Plus, http://www.nlm.nih.gov/medlineplus/kneereplacement.html 5 “Total Knee Replacement Overview”, Bay Area Medical Information, http://www.bami.us/Msk/TKR.html 6 “Articular Cartilage Restoration”, American Academy of Orthopaedic Surgeons, http://orthoinfo.aaos.org/topic.cfm?topic=a00422 7 “Arthritis is Joint Disease,” November 14, 2011, Osteoarthritis information, Knee Osteorthritis Information, http://www.osteoarthritisblog.com/category/aboutknee-osteoarthritis/ 8 “Wear-lines and split-lines of human patellar cartilage: relation to tensile biomechanical properties”; Bae, W. C.; Wong, V. W.; Hwang, J.; Anatonacci, J. M.; Nugent-Derfus, G. E.; Blewis, M. E.; Temple-Wong, M. M.; Sah, R. L.; Osteoarthritis and Cartilage, Volume 16, Issue 7, July 2008, Pages 841-845; http://www.sciencedirect.com.colelibprxy.ewp.rpi.edu/science/article/pii/S1063458407003780 9 “Treatment Options for Osteoarthritis in the Knee”, Palo Alto Medical Foundation http://www.pamf.org/sports/king/osteoarthritis.html 10 “Synovial Fluid”, Lipowitz, Alan J., Chapter 86, University of Pennsylvania, http://cal.vet.upenn.edu/projects/saortho/chapter_86/86mast.htm 11 “Friction and wear changes in synovial joints”; Stachowiak, G.W.; Batchelor, A.W.; Griffiths, L.J.; Wear, 171, 135-142, 1994. 12 “Shape, loading, and motion in the bioengineering design, fabrication, and testing of personalized synovial joints”; Williams, Gregory M.; Chan, Elaine F.; TempleWong, Michele M.; Bae, Wong C.; Masuda, Koichi; Bugbee, William D.; Sah, Robert L.; Journal of Biomechanics, Volume 43, Issue 1, 5 January 2010, Pages 156-165; http://www.sciencedirect.com.colelibprxy.ewp.rpi.edu/science/article/pii/S0021929009005120 13 “Obesity and knee arthroplasty”; Gillespie, G. N.; Porteous, A. J.; The Knee, Volume 14, Issue 2, March 2007, Pages 81-86; http://www.sciencedirect.com/science/article/pii/S0003999311003303 14 “Gait characteristics of patients with knee osteoarthritis”; Kaufman, Kenton R.; Hughes, Christine; Morrey, Bernard F.; Morrey, Michael; An, Kai-Nan; Journal of Biomechanics, Volume 34, Issue 7, July 2001, Pages 907-915, http://www.sciencedirect.com/science/article/pii/S0021929001000367 15 “Sex and Body Mass Index Correlate With Western Ontario and McMaster Universities Osteoarthritis Index and Quality of Life Scores in Knee Osteoarthritis”; Elbaz, Avi; Debbi, Eytan M.; Segal, Ganit; Haim, Amir; Halperin, Nahum; Agar, Gabriel; Mor, Amit; Debi, Ronen; Archives of Physical Medicine and Rehabilitation, Volume 92, Issue 10, October 2011, Pages 1618-1623; http://www.sciencedirect.com/science/article/pii/S0003999311003303 16 “Tibial subchondral bone size and knee cartilage defects: relevance to knee osteoarthritis”; Ding, C.; Cicuttini, F.; Jones, G.; Osteoarthritis and Cartilage, Volume 15, Issue 5, May 2007, Pages 479-486; http://www.sciencedirect.com.colelibprxy.ewp.rpi.edu/science/article/pii/S1063458407000106 4 12 “Effect of tibial component varus on wear in total knee athroplasty”;Srivastava, Ajay; Lee, Gregory Y.; Steklov, Nikolai; Colwell Jr., Clifford W.; Ezzet, Kace A.; D’Lima, Darryl D.; The Knee, Volume 19, Issue 5, October 2012, Pages 560-563; http://www.sciencedirect.com.colelibprxy.ewp.rpi.edu/science/article/pii/S0968016011002043 18 “Tibial subchondral bone size and knee cartilage defects: relevance to knee osteoarthritis”; Ding, C.; Cicuttini, F.; Jones, G.; Osteoarthritis and Cartilage, Volume 15, Issue 5, May 2007, Pages 479-486; http://www.sciencedirect.com.colelibprxy.ewp.rpi.edu/science/article/pii/S1063458407000106 19 “Tibiofemoral cartilage thickness distribution and its correlation with anthropometric variables”; Connolly, A.; FitzPatrick, D.; Moulton, J.; Lee, J.; Lerner, A.; Proc Inst Mech Eng H., 2008 Jan, 222(1), 29-39; http://www.ncbi.nlm.nih.gov/pubmed/18335716 20 “The Width:thickness Ratio of the Patella”; Iranpour, Farhad; Merican, Azhar M.; Amis, Andrew A.; Cobb, Justin P.; Clin Orthop Relat Res., 466(5), 1198-1203, May 2008; http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2311467/ 21 “Age- and site-associated biomechanical weakening of human articular cartilage of the femoral condyle”; Temple, M. M.; Bae, W. C.; Chen, M. Q.; Lotz, M.; Amiel, D.; Coutts, R. D.; Sah, R. L.; Osteoarthritis and Cartilage, Volume 15, Issue 9, September 2007, Pages 1042-1052; http://www.sciencedirect.com.colelibprxy.ewp.rpi.edu/science/article/pii/S1063458407001070 22 “Introduction to Bioengineering”; Fung, Yuan Cheng; Chien, Shu; p. 163 23 “Dynamic Simulation of Knee Joint Contact During Human Movement”, Yanhong, Bei, University of Florida, Ph. D. Dissertation, 2003, http://etd.fcla.edu/UF/UFE0002364/bei_y.pdf 24 “Computational Wear Simulation of Patellofemoral Articular Cartilage during In Vitro Testing”; Li, Lingmin; Patil, Shantanu; Steklov, Nick; Bae, Won; Temple-Wong, Michele; D’Lima, Darryl D.; Sah, Robert L.; Fregly, Benjamin J.; J Biomech, 44(8), 1507-1513, May 2011, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3119794/ 25 “Computational Wear Simulation of Patellofemoral Articular Cartilage during In Vitro Testing”; Li, Lingmin; Patil, Shantanu; Steklov, Nick; Bae, Won; Temple-Wong, Michele; D’Lima, Darryl D.; Sah, Robert L.; Fregly, Benjamin J.; J Biomech, 44(8), 1507-1513, May 2011, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3119794/ 17 13