File
By Cristina Roybal CVT
Vet 402- Advanced Veterinary Terminology
Tarleton State University
History
:
Leo is a four year-old, male/neutered, French Bulldog. Leo presented to the emergency service at the Center for Veterinary Specialty Care in
Carrollton, Texas for an acute (rapid) onset of non-ambulatory paraparesis (inability to walk in hind legs, hind limb weakness) that occurred over the previous 24-48 hours following a traumatic incident while playing with another dog. Initially, Leo seemed a little off balance but not overtly painful and was weak in the hind limbs, though able to walk without assistance. He is now unable to walk without assistance.
Leo was seen previously for an intervertebral disk extrusion that was surgically corrected three years prior to the current presentation. The owners report that Leo has also stopped eating.
Physical Exam
:
Leo presents quiet, alert, and responsive (QAR), Temperature: 101.6
(normal), Heart Rate 80 bpm (normal), and Respiratory Rate: 100 bpm/Panting (high). Leo is unable to stand without support. He can maintain his own weight for about 15-20 seconds. The patient has good voluntary motor (the ability to move) to both hind legs. He is weak in both hind legs, though notably stronger on the left side.
When an animal has an intervertebral disc rupture, it can be described similarly to the jelly of a jelly donut exploding out.
The disk is the cushion between the vertebrae in the spine. The force of the explosion and the compression of the jelly on the spinal cord causes pain and loss of function.
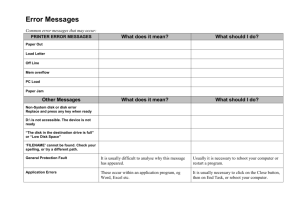
There are several diagnostic options to evaluate a potential disk extrusion. Many of them require general anesthesia.
Radiographs may be taken to rule out diskospondylitits (an inflammatory process of the vertebrae), neoplasia (abnormal growth such as a tumor), or trauma to the spine.
Myelography: A myelogram uses a contrast medium (fluid) that is injected into the spinal canal, after which a series of radiographs are taken to see where the disk compression is located.
Computed Tomography (CT): CT uses ionic radiation that passes through the patient, and images of the internal body structures can be viewed on a computer. This type of study is helpful in diagnosis of a herniated disk, but may be more diagnostic when combined with myelography.
Magnetic Resonance Imaging (MRI): MRI uses radio waves and a magnetic field to obtain images of the animal’s internal body structures. MRI allows for the best classification of disk herniations. For example, whether the disk is extruding, protruding or bulging
(Griffin, Levine, Kerwin, & Cole, 2009). MRI tends to be very expensive and there is limited availability in veterinary medicine.
Click here for a video of Dr. Stephen Lane DVM,
Diplomate ACVIM (neurology) discussing diagnosis of intervertebral disc disease (IVDD) using MRI.
Assessment
: A complete blood count (CBC) and chemistry profile were completed for pre-anesthetic bloodwork. His CBC showed a slightly low platelet count, and the chemistry profile had an elevated cholesterol and bilirubin. A blood smear revealed that his platelet count was adequate. Leo was cleared for anesthesia.
Diagnostic Plan
: Leo was anesthetized for a CT with the possibility of a myelogram for a suspected intervertebral disk extrusion.
Treatment Plan
: The CT showed a large amount of disk material causing a compression in the thoracic vertebral region (chest), specifically at the T-11, T-12 junction.
Leo was moved directly from CT into the operating room to have a hemilaminectomy (right-sided approach) in order to relieve the compression.
A hemilaminectomy is one of the surgical options for relieving the compression of a herniated disk. This procedure indicates for the surgeon to create a window on either the left or right side of the vertebral canal by drilling through the vertebra(e), using a high-speed drill, where the herniated disk is underlying. Using the previous donut example, the surgeon creates an opening through the vertebral body to carefully remove the jelly from around the spinal cord. Click here for a video of this procedure from Southpaws
Veterinary Specialty Surgery in
Melbourne.
According to an article by doctors John
F. Griffin IV, Jonathan M. Levine,
Sharon C. Kerwin, and Robert C. Cole in
2009, hemilaminectomy is a more beneficial option compared to dorsal laminectomy to relieve the compression of a herniated disk.
Post operative supportive care, pain management, bladder management, and physical therapy are imperative for the success of a hemilaminectomy to treat an intervertebral disk extrusion.
Post operative hemilaminectomy patients will typically be hospitalized anywhere from three to five days.
The patient may receive intravenous (IV) fluids as well as IV and oral pain medications
Depending on the patient’s ability to voluntarily move the pelvic (hind) limbs, the management of the urinary bladder is also necessary. This may include placing a closed urinary collection system, using a catheter intermittently to empty the bladder, or via manual expression of the bladder by palpating
(feeling for) the bladder and applying a consistent pressure until the sphincter releases and the bladder allows urine to be emptied.
Leo was placed on intravenous plasmalyte (IV fluids) for supportive care.
An indwelling urinary catheter with a closed collection system was placed to facilitate emptying Leo’s bladder.
Leo received intravenous hydromorphone every six hours for the first 24 hours after surgery for pain, and was then started on oral Tramadol and Gabapentin for pain management.
For the first 24 hours after surgery, the surgery site was cold compressed every six hours, and this was followed by warm compresses the for the next 24 hour period.
Leo also received laser treatments via the Companion Therapy Laser to assist with controlling edema and swelling around the surgery site.
This picture was taken the night Leo had his back surgery.
Physical Therapy can include passive range of motion and massage of the affected limbs, supported standing exercises, underwater treadmills and swimming pools, and etc. Physical therapy helps the patient regain strength in the muscles that may atrophy (waste away) from lack of use while the patient is unable to walk.
Once the patient is sent home, they are to be strictly cage rested for about six weeks. During this time, there should be no running, jumping, stair climbing, or rough-housing. The dog can be taken outside to urinate/defecate, but are not permitted to go on lengthy walks until they are past the six week mark.
Owners can continue physical therapy to help their companion get their strength back in the hind legs.
Leo’s surgery was a success. Leo was hospitalized in the intensive care unit at the Center for Veterinary
Specialty Care for three days after surgery. The first day after surgery he was weak, but he gradually regained strength in his hind legs with physical therapy. Leo was discharged from the hospital to go home with his owners. By that time, he was able to urinate and empty his bladder on his own. His owners continued to perform his physical therapy at home where Leo got stronger every day. Leo is making a full recovery.
The hemilaminectomy was performed early enough after the incident that Leo was able to recover quickly. According to the experts, the sooner a patient has surgery after an acute disk rupture, the better their chances are for recovery.
Griffin, J.F., Levine, J.M., Kerwin, S.C., & Cole, R.C. (2009).
Canine Thoracolumbar Intervertebral Disk Disease: Diagnosis,
Prognosis, and Treatment. Compendium: Continuing
Education for Veterinarians. Retrieved from VetLearn.com.
Southpaws Specialist Veterinary Surgery. http://www.youtube.com/watch?v=grzlXcRXn5s
Rocky Mountain Veterinary Neurology. http://rockymountainveterinaryneurology.com/videointervertebral-disc-disease/
University of Pennsylvania School of Veterinary Medicine. http://cal.vet.upenn.edu/projects/saortho/chapter_62/62m ast.htm
Melbourne Veterinary Referral Centre. http://www.dcv.org.au/Documents/Intervertebral%20Disc%20
Disease.htm