ACID-BASE BALANCE
advertisement

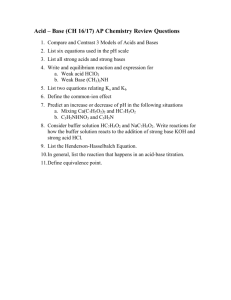
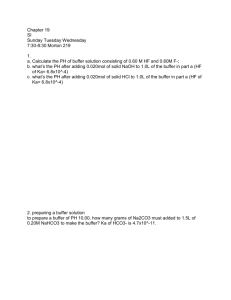
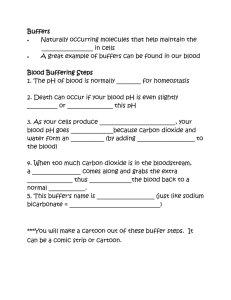
MLAB 2401: Clinical Chemistry Keri Brophy-Martinez Acid-Base Balance: Overview Terms Acid Any substance that can yield a hydrogen ion (H+) or hydronium ion when dissolved in water Release of proton or H+ Base Substance that can yield hydroxyl ions (OH-) Accept protons or H+ Terms pK/ pKa Negative log of the ionization constant of an acid Strong acids would have a pK <3 Strong base would have a pK >9 pH Negative log of the hydrogen ion concentration pH= pK + log([base]/[acid]) Represents the hydrogen concentration Terms Buffer Combination of a weak acid and /or a weak base and its salt What does it do? Resists changes in pH Effectiveness depends on pK of buffering system pH of environment in which it is placed Terms Acidosis Alkalosis pH less than 7.35 pH greater than 7.45 Note: Normal pH is 7.35-7.45 Acid-Base Balance Function Maintains pH homeostasis Maintenance of H+ concentration Potential Problems of Acid-Base balance Increased H+ concentration yields decreased pH Decreased H+ concentration yields increased pH Regulation of pH Direct relation of the production and retention of acids and bases Systems Respiratory Center and Lungs Kidneys Buffers Found in all body fluids Weak acids good buffers since they can tilt a reaction in the other direction Strong acids are poor buffers because they make the system more acid 8 Blood Buffer Systems Why do we need them? If the acids produced in the body from the catabolism of food and other cellular processes are not removed or buffered, the body’s pH would drop Significant drops in pH interferes with cell enzyme systems. Blood Buffer Systems Four Major Buffer Systems Protein Buffer systems Amino acids Hemoglobin Buffer system Phosphate Buffer system Bicarbonate-carbonic acid Buffer system Blood Buffer Systems Protein Buffer System Originates from amino acids ALBUMIN- primary protein due to high concentration in plasma Buffer both hydrogen ions and carbon dioxide Blood Buffering Systems Hemoglobin Buffer System Roles Binds CO2 Binds and transports hydrogen and oxygen Participates in the chloride shift Maintains blood pH as hemoglobin changes from oxyhemoglobin to deoxyhemoglobin Oxygen Dissociation Curve Curve B: Normal curve Curve A: Increased affinity for hgb, so oxygen keep close Curve C: Decreased affinity for hgb, so oxygen released to tissues Bohr Effect It all about oxygen affinity! Blood Buffer Systems • Phosphate Buffer System • Has a major role in the elimination of H+ via the kidney • Assists in the exchange of sodium for hydrogen • It participates in the following reaction • HPO-24 + H+ H2PO – 4 • Essential within the erythrocytes Blood Buffer Systems Bicarbonate/carbonic acid buffer system Function almost instantaneously Cells that are utilizing O2, produce CO2, which builds up. Thus, more CO2 is found in the tissue cells than in nearby blood cells. This results in a pressure (pCO2). Diffusion occurs, the CO2 leaves the tissue through the interstitial fluid into the capillary blood Bicarbonate/Carbonic Acid Buffer Carbonic acid Conjugate base Bicarbonate Excreted in urine Excreted by lungs Bicarbonate/carbonic acid buffer system How is CO2 transported? 5-8% transported in dissolved form A small amount of the CO2 combines directly with the hemoglobin to form carbaminohemoglobin 92-95% of CO2 will enter the RBC, and under the following reaction CO2 + H20 H+ + HCO3- Once bicarbonate formed, exchanged for chloride Henderson-Hasselbalch Equation Relationship between pH and the bicarbonate-carbonic acid buffer system in plasma Allows us to calculate pH Henderson-Hasselbalch Equation General Equation pH = pK + log A- HA Bicarbonate/Carbonic Acid system o pH= pK + log HCO3 H2CO3 ( PCO2 x 0.0301) Henderson-Hasselbalch Equation 1. 2. pH= pK+ log H HA The pCO2 and the HCO3 are read or derived from the blood gas analyzer pCO2= 40 mmHg HCO3-= 24 mEq/L 3. Convert the pCO2 to make the units the same pCO2= 40 mmHg * 0.03= 1.2 mEq/L 3. Lets determine the pH: Plug in pK of 6.1 4. 5. Put the data in the formula pH = pK + log 24 mEq/L 1.2 mEq/L pH = pK + log 20 pH= pK+ 1.30 pH= 6.1+1.30 pH= 7.40 The Ratio…. Normal is : 20 = Kidney 1 Lungs = metabolic respiratory The ratio of HCO3- (salt) to H2CO3 ( acid) is normally 20:1 Allows blood pH of 7.40 The pH falls (acidosis) as bicarbonate decreases in relation to carbonic acid The pH rises (alkalosis) as bicarbonate increases in relation to carbonic acid Physiologic Buffer Systems Lungs/respiratory Quickest way to respond, takes minutes to hours to correct pH Eliminate volatile respiratory acids such as CO2 Doesn’t affect fixed acids like lactic acid Body pH can be adjusted by changing rate and depth of breathing “blowing off” Provide O2 to cells and remove CO2 Physiologic Buffer Systems Kidney/Metabolic Can eliminate large amounts of acid Can excrete base as well Can take several hours to days to correct pH Most effective regulator of pH If kidney fails, pH balance fails 25 References Bishop, M., Fody, E., & Schoeff, l. (2010). Clinical Chemistry: Techniques, principles, Correlations. Baltimore: Wolters Kluwer Lippincott Williams & Wilkins. Carreiro-Lewandowski, E. (2008). Blood Gas Analysis and Interpretation. Denver, Colorado: Colorado Association for Continuing Medical Laboratory Education, Inc. Sunheimer, R., & Graves, L. (2010). Clinical Laboratory Chemistry. Upper Saddle River: Pearson . 26