clinical trials2014
advertisement

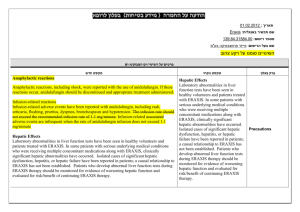
Epidemiology Clinical Trials 23.10.2014 Outline • Basic principles • Biases • Ethics- GCP • Statistical analysis • Ethics Well-designed clinical research Methodology Ethics What is a clinical trial? • Prospective study comparing the effect and value of intervention(s) (against a control) in human subjects (Comparative) • Alternative definition- experimental study in humans in which the investigator determines the exposure/intervention אלגוריתם לסיווג סוגי מחקר בבני אדם !!היום Surveys Case Reports Case Series Ecological study Early phases of clinical research Pre-clinical studies • Pre-clinical studies involve in vitro and in vivo experiments Phase 0 – FDA 2006 • “first-in-human” trials also known as human microdosing studies • designed to speed up development of promising drugs or imaging agents • administration of single subtherapeutic doses of study drug to a small number of subjects (10 to 15) to gather preliminary data on pharmacokinetics and pharmacodynamics • give no data on safety or efficacy, being by definition a dose too low to cause any therapeutic effect. Phase I - clinical trial new drug • Objective: dose finding for future trials • Participants: – in cancer trials, usually patients with advanced, resistant disease – in benign disease -healthy volunteers (paid) Phase I - clinical trial • Start with low dose (1/10 of LD50 most sensitive species) • Dose increased in pre-planned steps until dose-limiting toxicity (DLT) occurs in >1/3 • Cohorts of 3-6 patients treated at each level Phase I - clinical trial Usually 6 patients at “recommended dose” to Phase II studies NB: - useful for toxicity and pharmacokinetics - not designed to test efficacy/biologic effect - sample size insufficient for comparative questions Phase II - clinical trial • Outcome of interest: response (shorter term outcomes) • Target group: most likely to show favorable response but no effective therapy available. Good performance status, minimal prior therapy • Eligibility: patients with specific diagnosis, no internal control group (sometimes randomized) Phase II - clinical trial • Response does not translate necessarily to patient benefit • Concluding about treatment effectiveness is erroneous • High response rates in Phase II do not translate into improved survival in Phase III • In some diseases response is difficult to measure (no measurable disease) Phase III clinical trial • Randomized controlled clinical trial with sufficient sample size and long enough follow-up to determine treatment effect • Often multicentered • Frequently sponsored by pharmaceutical company or clinical trials consortium • Often administered by CRO • $$$$$$$$ Phase IV Clinical Trial • Post - marketing surveillance for side effects, tolerability, new indications • Often drug is provided for a limited time at no cost so that the company can collect the required information • Rare complications of drugs may only become apparent years after clinical trials (Ticlopidine – TTP, Eprex-PRCA) The unpredictable course of disease: the natural history of systemic lupus erythematosus in a patient observed before the advent of immunosuppressive drugs The unpredictable course of disease: the natural history of systemic lupus erythematosus in a patient observed before the advent of immunosuppressive drugs The unpredictable course of disease: the natural history of systemic lupus erythematosus in a patient observed before the advent of immunosuppressive drugs Total effects of treatment are the sum of spontaneous improvement, nonspecific responses and the effects of specific treatments The structure of a clinical trial Experimental Intervention Outcome Improved Not improved Population of patients with the condition SAMPLE ALLOCATION Improved Not improved Comparison Intervention Types of clinical trials: Parallel placebo controlled with composite outcome/endponts Crossover trial Most efficient and valid method of using patient as his own control Factorial design: Can answer n questions Randomization scheme for the PHS (physicians’ health study) Willing and eligible 22,000 Active Aspirin 11,000 Active carotene 5,500 Carotene placebo 5,500 Aspirin placebo 11,000 Active carotene 5,500 Carotene placebo 5,500 Clinical trials of equivalence Basic principles underlying confidence interval approach to equivalence/non-inferiority Garrett, Statist. Med. 2003 Clinical trials principles 1. Informed consent 2. Randomization 3. Blinding/masking - especially important for “soft” outcomes - single - double - “triple” 4. Objective, and equal assessment of outcomes 5. Monitoring committees and stopping rules Randomization 1. Guarantees equal probability of receiving control/experimental treatment to all participants (removes investigator bias) 2. Protects against imbalances in known and unknown confounders 3. Provides basis for statistical analysis Did the randomization work? Table 1 Stratified randomization: patients are first divided into strata (1-3) according to one or more prognostic factors and then randomized separately within each stratum into treatment (T) and control(C) groups Can’t always trust that randomization will result in balance Bias in clinical trials • Internal and external validity Location of potential bias in a randomized controlled trial Location of potential bias in a randomized controlled trial Internal Validity Unblinded trials (“open label”) Both participant and investigator know which intervention participant has been assigned - surgery - devices - lifestyle modification Advantages: Simpler, cheaper, more “comfortable” for investigator knowing patient assignment BIAS is the problem Bias in unblinded trials • Bias of expectation (participant and investigator) • Bias of reporting side effects (participant) • Bias of reporting adverse events • Increased withdrawal in placebo or control group Double blind trials • Neither the investigator nor the participant know treatment assignment • usually trials of drug efficacy (Sham treatments) • double blind assessments of interventions previously tested in single blind fashion may yield different conclusions • function of investigators must be taken over by others- monitoring toxicity and benefit Blinding • If pill – same color, sheen, texture, taste, smell • Same side effects? • If injection – same color, length of infusion, same care and fuss • Sham procedures, sham surgery Intention to treat analysis Drop out Population of patients with the condition Cross over Drop out Analysis according to treatment assigned Analysis by “intention to treat” • Should always be primary analysis • factors such as co-intervention, compliance, loss to follow-up may all be associated with the outcome (or the treatment effect) • proper strategy is to: a) randomize close to time of 1st treatment b) minimize these during the trial c) analyze according to treatment assignment Explanatory analysis Drop out Population of patients with the condition Cross over Drop out Analysis according to treatment received RCT – importance of Intention to treat Five-Year Mortality Drug Poor-Adherence Good Adherence NEJM 1980;303:1038 JAMA 1993;270:742 RCT- importance of intention to treat Five-Year Mortality Placebo Poor-Adherence Good Adherence NEJM 1980;303:1038 Location of potential problems of external validity in a randomized controlled trial External Validity Sampling for a clinical trial: the Coronary Artery Surgery Study (CASS) Circulation 68, 1983:939-950 % of patients remaining 100 Potentially eligible Seen at one of participating centers Suspected coronary artery disease Coronary angiogram 72 67 Exclusions Normal or minimally diseased Coronary arteries No operable vessels 30 Severe angina 29 Severe L. main coronary stenosis 13 Randomizable (after other exclusions) 5 Randomized Efficacy and effectiveness - + Internal validity Efficacy trial Does receiving treatment work under ideal conditions? Non-compliance + Less selected patients Less selected clinicians Costs Impracticality etc… Generalizability + - Effectiveness trial Does offering treatment help under ordinary circumstances? Effectiveness of treatment Efficacy: an intervention is efficacious if it does more good than harm in patients who use it. Effective: an intervention is effective if it does more good than harm in those patients to whom it is offered. Major Disadvantage of RCTs: Selectivity But…SHEP study Of 447,921 (100%) identified 31,960 (7.1%) met initial criteria 4,736 (1.06%) randomized . . Comorbidity: General Pop vs. Subgroup Men, gen’l pop % of Pop % of Pop DM CVD CHF MI Angina Wom., gen’l pop SHEP pop Messerli et al, Arch Int Med, 1999 How to measure effect in clinical trials The analysis of clinical trials Sackett BMJ 1994;309:755-6 Qualitative result: Treatment A is better than treatment B Statistical result: p < 0.05 Quantitative result: Risk ratio (Risk A: Risk B) (1-Risk ratio) x 100 = “relative risk reduction” Risk A - Risk B = “absolute risk reduction” 1/absolute risk reduction = NNT = number needed to treat to prevent 1 event” Naming the erroneous conclusions form a clinical trial The true state of affairs Drug A is better Drug A is no better than drug B than drug B Drug A is better than drug B TP Correct (1- = power) Conclusion drawn from a clinical trial FP Type I error (risk of making this error = =the P value!) w x y Drug A is no better than drug B Type II error (risk of making this error=) FN z Correct TN Meta-analysis: effect of antihypertensive drugs on patients with moderate to severe hypertension: five year follow up Treatment A = active antihypertensive drugs 1800 strokes among 15,000 patients randomized Risk = 1800 / 15,000 = 0.12 Treatment B = placebo or no active treatment 3000 strokes in 15,000 patients randomized Risk = 3000 / 15,000 = 0.20 Risk ratio = 0.12 / 0.20 = 0.6 Relative risk reduction = (1-0.6)x100 = 40% Absolute risk reduction = 0.20 - 0.12 = 0.08 NNT = 1/ 0.08 = 13 13 patients must be treated for five years to prevent one stroke Treatment of hypertension: changing definition of recommended treatment level over time What if trial done on mild hypertensives? Treatment A = active antihypertensive drugs 135 strokes among 15,000 patients randomized Risk = 135 / 15,000 = 0.009 Treatment B = placebo or no active treatment 225 strokes in 15,000 patients randomized Risk = 225 / 15,000 = 0.015 What if trial done on mild hypertensives? Risk ratio = 0.009/0.015 = 0.6 Relative risk reduction = (1-0.6)x100 = 40% Absolute risk reduction=0.015=-0.009=0.006 NNT=1/0.006 = 167 167 patients must be treated for 5 years to prevent one stroke The effect of different baseline risks and relative risk reductions on the number needed to treat Baseline (with no treatment) Relative risk reduction on treatment 50% 40% 30% 25% 20% 15% 10% .9 .6 .3 2 3 7 3 4 8 4 6 11 4 7 13 6 8 17 7 11 22 11 17 33 .2 .1 .05 10 20 40 13 25 50 17 33 67 20 40 80 25 50 100 33 67 133 50 100 200 .01 .005 .001 200 400 2000 250 500 2500 333 667 3333 400 800 4000 500 1000 5000 667 1333 6667 1000 2000 10000 Reducing mortality from colo-rectal cancer by screening for fecal occult blood Mandel NEJM 1993;328:1365-71 Assignment A = annual screening x 13 years Mortality 5.88 per 1000 Assignment B = biennial screening 13 years Mortality 8.33 per 1000 Assignment C = control group Mortality 8.83 per 1000 Risk ratio = A/C = 5.88/8.83 = 0.66 Relative risk reduction = (1-0.66) x 100 = 34% Abs.risk reduction = 0.00883 - 0.00588 = 0.00295 NNT = 1/0.00295 = 339 339 healthy people need to be screened yearly for 13 years to prevent one death from colo-rectal cancer Clinical Trials • Have made a huge impact on health • There are now 75 trials, and 11 systematic reviews of trials published per day and a plateau in growth has not yet been reached. • They are a problematic tool • PEOPLE ARE NOT MICE THEY CANNOT BE CONTROLLED Part two Ethics in clinical trials דרישות אתיות ETHICAL REQUIREMENTS Emanuel et al. JAMA 2000;283:2801-11 או מדעי/ערך חברתי ו SOCIAL &/OR SCIENTIFIC VALUE תוקף מדעי SCIENTIFIC VALIDITY בחירה הוגנת של משתתפים FAIR SUBJECT SELECTION תועלת חיובי-יחס סיכון FAVORABLE RISK-BENEFIT RATIO בקרה בלתי תלויה INDEPENDENT REVIEW הסכמה מדעת INFORMED CONSENT כבוד למשתתפים הפוטנציאלים והמגויסים RESPECT FOR POTENTIAL & ENROLLED SUBJECTS • • • • • • • • • • • • • • Ethical issues in clinical trials 1. Equipoise 2. Timing (“Enroll the first patient” Chalmers) 3. Inadequate sample size 4. Selective enrollment of patients 5. Violation of eligibility criteria Ethical issues in clinical trials (cont.) 6. Violation of randomization 7. Placebo/sham ethical? 8. Change in doctor/patient relations 9. Fraud in execution or analysis 10. Data dredging/selective presentation of results Macon County Study • 1929 -- Julius Rosenwald fund asks US public health service (PHS) for assistance in developing health programs for southern blacks (fund establishes a medical division to complement its educational activities) • PHS suggests demonstration treatment program for syphilis. Official Apology 1997 Equipoise B. Freedman NEJM 1987;317:141-5 “a state of genuine uncertainty regarding the comparative merits of treatments A and B for population P. Disturbed by: - prior prejudice/thoughts about treatment - preparation of research proposal - preliminary or interim results of trial Informed consent • Practical expression of autonomous choice • Modifications of consent required in 1/4 of protocols Ingredients - participants must: 1) have legal capacity to consent 2) be sufficiently free that consent is truly voluntary 3) be given adequate information 4) understand information well enough to make enlightened decisions Death of A Research Volunteer • Johns Hopkins University Asthma Study • 24 year old lab technician -volunteer • died of pulmonary complications of inhaled drug • after methacholine challenge given hexamethonium • pulmonary complications (rare) described in pre-1966 literature- not in informed consent • drug not FDA approved “Not quite as random as I pretended Lancet 1996;347:70 Most people are uncomfortable with the idea that important decisions should hang on chance • hold envelope up to light • change schedule • open bottles Violation of randomization יחידת הלב -ע”כ .Iלפני 3שנים בערך השתתפה היחידה במחקר גוסטו .במסגרתו נבדקה יעילות של T.P.Aלעומת -S.T.Kסטרפטוקינז בטיפול בחולים עם .Acute MIבאחד המקרים התקבל חולה בן 78עם Acute MIשהסכים להשתתף במחקר וחתם .נפתחה הערכה שהוא אמור לקבל לאחר תיאום עם מרכז הרנדומיזציה והתברר שיש לו ערכה ( S.T.Kנא לציין ש T.P.A -היא תרופה מאוד יקרה .ביחידה שמורה רק מנה אחת ואפשר להשתמש בה רק לאחר תיאום ואישור מההנהלה) .זה לא מצא חן בעיני הרופא המטפל כי הוא קיווה שיהיה T.P.Aלכן הוא פתח ערכה אחרת והתחיל לחפש , T.P.Aפתח עוד ערכה עד שמצא .שהתברר המעשה למרכזי המחקר נפסלה היחידה ככלל והורדה מכל המחקר שבמקביל רץ בהרבה יחידות באירופה וארה”ב. Fraud and clinical trials • • • • • • falsification of data entry of ineligible participants phantom participants (Ruben, Bezwoda) randomization procedure violation protocol violations publication fraud What is Misconduct? FDA’s Focus • Deliberate or repeated noncompliance with the regulations can be considered misconduct, but is a secondary focus compared to falsification of data. • Research misconduct does not include honest error or honest differences of opinion. Fakery • Baystate Medical Center in Springfield, Massachusetts, asked several anesthesiology journals to retract 21 drug studies published 1996-2008 by anesthesiologist Scott S. Reuben, M.D., a pioneer in the area of multimodal analgesia. • The studies were funded by Pfizer, Merck, and Wyeth. Reuben was also paid by Pfizer as a speaker to promote its products .Raymond F. Kerins Jr., a Pfizer spokesman: "It is very disappointing to learn about Dr. Scott Reuben's alleged actions". • Reuben is suspected of falsifying some of his data, including the names of patients and co-authors. Evan Ekman, MD, an orthopedic surgeon in Columbia, S.C., told Anesthesiology News that his name was forged on two of the retracted papers. • Dr. Hal Jenson, Baystate's chief academic officer, said that the investigation of Reuben's work found that in many cases "there was no clinical trial because there were no patients". Falsification of Data • Falsification of data includes creating, altering, recording, or omitting data in such a way that the data do not represent what actually occurred. The Misconduct Scale • Innocent Ignorance- misconduct of the uninformed kind – Noncompliance based on lack of understanding the regulatory consequences of an action. The act itself is usually intentional but the noncompliance is unintentional, not usually done to deliberately deceive The Misconduct Scale • Surprising Sloppiness- misconduct of the lazy kind – Consent forms inadvertently not obtained from subjects – Blood pressures rounded to the nearest 5mm – Data estimated rather than actually measured – Data inaccurately transcribed or recorded – Protocol ignored or shortcuts taken The Misconduct Scale • Surprising Sloppiness- misconduct of the lazy kind – Noncompliance due to inaction, inattention to detail, inadequate staff, lack of supervision. The act itself may be intentional or unintentional, the noncompliance is unintentional and usually repeated The Misconduct Scale • Malicious Malfeasance- Misconduct of the sleazy kind – Usually noncompliance due to deliberate action to deceive or mislead includes The “F” Word: Falsification Detecting and Handling Research Misconduct • The Fiddes Case • Background: shortage of research patients • Dr. Robert Fiddes turned his “sleepy” medical practice Whittier.Ca into major clinical research org. • Another study on an antibiotic required that patients have a certain type of bacteria growing in their ear. No problem for Fiddes. He bought the bacteria from a commercial supplier and shipped them to testing labs, saying they had come from his patients' ears.” • If patient didn’t have the condition – he bought urine from someone who did • 1997 found guilty – 15 month prison sentence Israel –role of Helsinki committee • הועדה פועלת על-סמך נוהל לניסויים רפואיים בבני אדם, בהתאם לתקנות בריאות העם (ניסויים רפואיים בבני אדם ,התשמ”א ,1980 ,על תוספותיהן ותיקוניהן ,)1999 ומיישמת את עקרונות הצהרת הלסינקי. • הוועדה דנה בהצעות מחקר לניסויים קליניים בבני אדם ומאשרת אותן ,וכן דנה בהצעות מחקר בתחום החברתי (פסיכולוגיה ,רפואה חברתית ובקשות הכוללות שאלונים). • ועדת הלסינקי המוסדית ,פועלת על-פי הוראות נוהל משרד הבריאות והוראות הנוהל ההרמוני הבינלאומי, העדכני ,להליכים קלינים נאותים (.)ICH-GCP ממשרד הבריאות נמסר" :בעקבות בדיקת מבקר המדינה בנושא ניסויים רפואיים שבוצעו בבית החולים הרצפלד וקפלן, 2011 ואיכות לבדיקת הנושא. מונתה בתאריך 28.6.05ועדת בקרה החלטת משרד הבריאות:קובלנה "בעקבות פרסום ממצאי מבקר המדינה וכן בעקבות דוח ועדת הבקרה ממחנה • המוות של הרבנית ברטה ויזל ( ,)84ניצולת שואה והאיכות פתחה משטרת ישראל בחקירה פלילית בנושא ,שהסתיימה המזעזעת. הפרשה לחשיפת זה שהביא בית ,היה אושוויץ ההשמדה היא מכונה בקובלנה, הרצפלד" ,כך הגריאטרי החולים פרשת " לאחרונה. בתה ,אחות בטוב. שלא לאחר בקפלן 2004 ויזל אושפזה ב- המדינה. חשה מבקר 2004למשרד בתחילת שהגיעה בעקבות תלונה נולדה הניסויים הפיקוחמ"על כיכשל בניסוייםשל שנגלתה, התמונה " בחולים קפלן" רופאים שלידי מערכתי על- הנעשים חוקיים לא גילתהעסקה לנוכח התלונה באמה ניסוי מבצעים האשפוז במהלך במקרה במקצועה, הפרקליטות. להפסיקלעיון המקרה הועבר הסכמתם לניסויים לתת כשירים שחלקם לא מבוגרים, כהונת את הבריאות .דאז משרד השתן“ל מנכ החליט החולים - של בבית מכן היא לאחר ימים ארבעה . הבטן דרך שלפוחית דיקור בתום חקירה ארוכה החליטה הפרקליטות לסגור את התיק מאחר שהיה קושי לקבוע אם פלילית.המרכזיים החברים את קפלן ולהחליף החולים ועדת הלסינקי של בית שהניסויעבירה היטבבפרשה הזאת ידעהשנעשתה אפשר להוכיח הרצפלדשהוא משום , חוקי אינו הבת מזיהום. נפטרה החולים בבית מחקרים נעצרו ממושכת תקופה ובמשך , בהרכבה הפרקליטות המליצה למשרד הבריאות להעמיד את החשודים לדין משמעתי, אמה כי העובדה לאור במיוחד אמה של הסכמתה אדםר". קליניים ניסויים בביתבביצוע ליקויים משמעתית" -בעניין הגשת ללאהחליט נעשה וזה בבני -,ד“ בנוסף קפלן. החולים המחקר קובלנהבקשות על כל פיקוחעלצמוד והוטל עבודתו.מאחותה בתקופת שהותה באושוויץ ,כדי שהופרדה תאומהסיים את הייתהשמואל לוי שלא תילקח לניסויים הזוועתיים של יוזף מנגלה .לפני כל ביקור נכתבו כולה, אומרת מהפרשה הייתהמערכתיים הופקו לקחים בבית"פרט לכך, נהליםעליי .אל ילמדו שלא לילדיה" : החולים היא מעודכנים והוגבר הפיקוח על הניסויים הרפואיים בכל בתי בישראל .עליי ניסויים". להם לעשות תיתנו החולים מבית החולים הרצפלד ,שירותי בריאות כללית ,והרופאים המעורבים בפרשה ומועסקים עדיין בכללית Clinical trials registration What and why? September 2004 A Statement from the International Committee of Medical Journal Editors • “In return for the altruism and trust that make clinical research possible, the research enterprise has an obligation to conduct research ethically and to report it honestly” • Concealing the presence of trials is dishonest! • Concealing the original purpose of the trial is also dishonest! Login Organization: User Name: Password: Forgot password Analysis of discrepancies between protocol and publication (Denmark and Canada) have shown.. • Publication bias is a real issue – Negative studies less likely to be published, especially by pharma • So is selective reporting of results – Statistically significant results more likely to be reported – Secondary outcomes and subgroup analyses presented as primary outcome Trial Registration Pros • • • • Enhanced public confidence All volunteers for medical research will contribute to improving human health Decrease publication bias Decrease selective presentation of results and inappropriate subgroup comparisons Cons • Bureaucratic delays • Gives an advantage to the competition Student’s role in research ethics • • • • Be aware of guidelines Be alert-ראש גדול Be honest Don’t do anything that makes you uncomfortable • Don’t chase the magic p value • Discuss authorship early