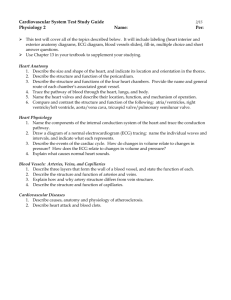
Chapters 12 & 13
advertisement

Chapters 13 The Cardiovascular System Human Anatomy & Physiology P. Wilson 1 II. 13.1 Introduction A. The functions of the cardiovascular system are: • to bring oxygen & nutrients to all cells • to remove wastes from cells, and • to carry the cellular wastes to sites of excretion. Human Anatomy & Physiology P. Wilson 2 III. 13.2 Structure of the heart A. The precise location of the heart is as follows: • in the mediastinum of the thoracic cavity • medial to the lungs (between them) • posterior to the sternum • anterior to the spine • base of the heart (upper portion) is beneath the 2nd rib • the heart extends inferiorly & to the left ending in a bluntly pointed apex at the level of the 5th intercostal space Human Anatomy & Physiology P. Wilson 3 III. 13.2 13.2 Structure of the heart B. Coverings of the Heart 1. The heart is enclosed by a double-layered pericardium. 2. The function of the serous fluid in the pericardial space is to reduce the friction between the pericardial membranes as the heart moves. http://www.youtube.com/watch?v=uR4t__B-Zwg 3. Pericarditis is an inflammation of the pericardium due to a viral or bacterial infection. • The inflammation produces adhesions in the layers of the pericardial sac that binds the 2 layers together; this restricts the movement of the heart AND causes significant pain. • Also, restriction of cardiac movement reduces the effectiveness of the heart’s pumping action. Human Anatomy & Physiology P. Wilson 4 III. 13.2 Structure of the Heart C. Wall of the Heart • Epicardium (the visceral pericardium) - reduces friction as the heart contracts & relaxes • Myocardium – the muscles of the heart that pump blood out of the heart chambers • Endocardium – the inner layer; contains blood vessels and specialized Purkinje fibers (carry impulses that cause the walls of the ventricles to contract. Human Anatomy & Physiology P. Wilson 5 Human Anatomy & Physiology P. Wilson 6 III. 13.2 Structure of the Heart D. 2 Human Anatomy & Physiology P. Wilson 7 III. 13.2 Structure of the Heart D. Heart Chambers & Valves 1. The chambers of the heart are the left & right atria (singular: atrium) and the left & right ventricles. 2. drawing to label 3. The right atrium receives oxygen-poor blood (from the body)from the inferior & superior vena cava and (from the heart) from the coronary sinus. 4. The left atrium receives oxygen-rich blood (from the lungs) via the 4 pulmonary veins – 2 veins from each lung/ Human Anatomy & Physiology P. Wilson 8 III. 13.2 Structure of the Heart E. The path of blood through the heart: • from coronary sinus and inf. & sup. vena cava into the right atrium • thru the tricuspid valve into the right ventricle • thru the pulmonary valve into the pulmonary arteries and thru the lungs then into the pulmonary veins • thru the pulmonary veins into the left atrium • thru the mitral (bicuspid) valve into the left ventricle • thru the aortic valve into the aorta then to the body Human Anatomy & Physiology P. Wilson 9 III. 13.2 Structure of the Heart F. Mitral valve prolapse occurs when leaflets of the valve bulge into the left atrium during ventricular contraction. This can allow blood to regurgitate back into the atrium. • Patients with this condition must take antibiotics before any invasive procedure to prevent further damage to the valves due to bacterial infection. Human Anatomy & Physiology P. Wilson 10 III. 13.2 Structure of the Heart G. The cells of the heart are supplied with blood by way of the right & left coronary arteries Human Anatomy & Physiology P. Wilson 11 III. 13.2 Structure of the Heart H. The muscles of the heart can suffer damage when deprived of oxygen. A first indication there is an interruption of oxygen to the muscle cells is pain. A prolonged interruption of oxygen supply will result in death of myocardial cells – a myocardial infarction (aka heart attack). I. Myocardial infarction results in irreversible, permanent damage to the heart muscle. Angina pectoris is the result of a temporary interruption of oxygen to cells and does not result in tissue scarring or permanent damage. Human Anatomy & Physiology P. Wilson 12 IV. 13.3 Heart Actions A. The cardiac cycle 1. consist of: • atrial systole (contraction) simultaneous with ventricular diastole (relaxation) ; then • ventricular systole (contraction) simultaneous with atrial diastole (relaxation). Note: the tricuspid & bicuspid (mitral) valves open & close simultaneously; the pulmonic & aortic valves open & close simultaneously. • Systole = when the TV & MV are closed and the PV & AV are open • Diastole = when the TV & MV are open and the PV & AV are closed Human Anatomy & Physiology P. Wilson 13 IV. 13.3 Heart Actions A. 2. The first heart sound (lubb) is the ventricular systole when the A-V valves are closing; the second heart sound (dubb) is the ventricular diastole when the pulmonary & aortic valves are closing B. Cardiac muscle fibers are similar to skeletal muscle except the fibers connect in branching networks, they self-exciting, and display rhythmicity. Stimulation to any part of the network sends impulses throughout the network. Human Anatomy & Physiology P. Wilson 14 IV. 13.3 Heart Actions, part C.1. Human Anatomy & Physiology P. Wilson 15 Start here on Monday! Human Anatomy & Physiology P. Wilson 16 IV. 13.3 Heart Actions C. Cardiac pulse conduction starts in the sinoatrial (S-A) node located in the right atrium. S-A node activity is rhythmic & initiates 70 to 80 impulses a minute. Because its generated the heart’s rhythmic contractions, it is called the heart’s pacemaker. D. 1. A recording of the electrical changes in the myocardium is an electrocardiogram (ECK or EKG). Human Anatomy & Physiology P. Wilson 17 IV. 13.3 Heart Actions E. 2. Calcium ions(Ca2+) & potassium ions (K+) affect heart rate in the following ways: • hyperkalemia (increased levels of K+) decreases heart rate • hypokalemia (low levels of K+) can lead to abnormal heart rhythm • hypercalcemia (high levels of Ca2+) can lead to an abnormally long contraction of the heart • hypocalcemia (lowlevels of Ca2+) can depress heart action NOTE about abnormal heart rhythms: tachycardia means the heart rate is faster than normal bradycardia means the heart rate is slower than normal Human Anatomy & Physiology P. Wilson 18 V. 13.4 Blood Vessels A. Arteries 1. The closed circuit (means that blood stays with vessels) includes arteries, arterioles, capillaries, venules, & veins. Paperman sez there are ~62000 miles of blood vessels in the human body; enuf to stretch 2.5 times around the world! 2. Arteries are tri-layered, strong, elastic vessels that are adapted to carry blood away from the heart under high pressure; they are capable of constricting & dilating when stimulated by the autonomic nervous system. Human Anatomy & Physiology P. Wilson 19 Page 330 Blue Box: Heart Transplant The recipient’s failing heart is removed except for the posterior walls of the atria and their connections to the vena cavae & pulmonary veins. The donor heart is prepared similarly and is attached to the atrial cuffs remaining in the recipient’s thoracic cavity. The recipient’s aorta & pulmonary arteries are connected to those of the donor heart. Human Anatomy & Physiology P. Wilson 20 V. 13.4 Blood Vessels A. Arteries 3. Arterioles are smaller vessels than arteries, have tri-layered walls similar to arteries, & are capable of vasodilation & vasoconstriction like arteries. • As arterioles approach capillaries, they become smaller & their walls thin; the walls of a very small artery consist only of an endothelial lining & some smooth muscle fibers surrounded by a small amount of connective tissue. Human Anatomy & Physiology P. Wilson 21 V. 13.4 Blood Vessels A. Arteries 4. Atherosclerosis is a disease of the arteries in which fatty plaques are formed in the vessel walls. This causes narrowing & roughening of the inner wall of the artery which, in turn, can lead to thrombus formation. Human Anatomy & Physiology P. Wilson 22 V. 13.4 Blood Vessels B. Capillaries 1. Capillaries are the smallest of blood vessels; they connect the smallest of the arterioles with the smallest of the venules. Capillaries are extensions of the inner linings of arterioles & form a semi-permeable layer through which exchanges of substances with cells take place. 2. The number of capillaries in a tissue (or the density of the capillary bed) is determined by the tissue’s rate of metabolism: • muscle & nervous tissues (which require an abundant supply of oxygen & nutrients) have a high density of capillaries • tissues with slow metabolic rates (cartilage, the epidermis, the cornea of the eye) have a low density of, or lack, capillaries. Human Anatomy & Physiology P. Wilson 23 V. 13.4 Blood Vessels B. Capillaries 3. The distribution of blood in the capillary pathways varies as the metabolic demands of the surrounding tissue varies. The distribution is controlled by pre-capillary sphincters which can open or close a pathway based on the demands of surrounding cells. Human Anatomy & Physiology P. Wilson 24 V. 13.4 Blood Vessels B. Capillaries 4. The endothelial cells in the capillaries of the brain are very tightly connected & allow very few substances to enter the brain. This serves as a protective barrier for the brain. The flip side – it makes it difficult to treat infections such as encephalitis & meningitis, and brain malignancies (neither antibiotics nor chemotherapeutic agents cross the blood brain barrier). 5. Transport mechanisms: • diffusion allows substances to cross membranes due to a concentration gradient – nutrients & oxygen move out of capillaries, carbon dioxide & other wastes move into capillaries. • filtration & osmosis are the other 2 transport mechanisms. Human Anatomy & Physiology P. Wilson 25 V. 13.4 Blood Vessels C. Veins 1. (& 2.) The walls of veins also have 3 layers but the walls of veins are thinner, less elastic, and have less smooth muscle than arteries. The inner walls of veins have valves that prevent the back flow of blood and keep it moving toward the heart. 3. When a drop in blood volume (due to hemorrhage) causes a drop in blood pressure, the walls of veins are stimulated to constrict (by the sympathetic nervous system); this maintains blood pressure by returning more blood to the heart and ensures a nearly normal blood flow even when as much as 25% of blood volume is lost. Human Anatomy & Physiology P. Wilson 26 VI. 13.5 Blood Pressure A. Blood pressure 1. Blood pressure is the force that blood exerts against the inner walls of blood vessels. This force occurs throughout the vascular system but the term blood pressure most commonly refers to pressure in the arteries supplied by branches of the aorta. Paper man sez the human heart creates enuf pressure to squirt blood 30 FEET! Human Anatomy & Physiology P. Wilson 27 VI. 13.5 Blood Pressure 2. The maximum pressure during ventricular contraction is the systolic pressure. When the ventricles relax, the arterial pressure drops, and the lowest pressure that remains in the arteries before the next ventricular contraction is the diastolic pressure. In a blood pressure reading of 120 / 80, 120 is the systolic pressure and 80 is the diastolic pressure. 3. The surge of blood entering the arterial system during a ventricular contraction causes the elastic arterial walls to expand. This expansion can be felt in arteries near the surface of the body as a pulse. Human Anatomy & Physiology P. Wilson 28 VI. 13.5 Blood Pressure B. Influencing Factors • Heart action: the volume of blood discharge from the left ventricle with each contraction is called the stroke volume. If either stroke volume or heart rate increases so does cardiac output and blood pressure will rise initially. • Blood volume equals the sum of the formed elements & blood plasma in the vascular system; blood pressure is normally directly proportional to blood volume in the cardiovascular system. Human Anatomy & Physiology P. Wilson 29 VI. 13.5 Blood Pressure B. Influencing Factors • Peripheral resistance, the force produced by friction between the blood and the walls of a blood vessel, hinders blood flow; blood pressure must overcome peripheral resistance if blood is to continue to flow. Therefore, factors that alter PR will change blood pressure. If PR lessens, BP lessens and visa versa. • Viscosity is the ease with which a fluid’s molecules flow past each other. The greater the viscosity, the greater the resistance to flowing. Increased viscosity increases BP; decreased viscosity decreases BP. Human Anatomy & Physiology P. Wilson 30 VI. 13.5 Blood Pressure Hypertension (high blood pressure) is a condition in which the arterial pressure is persistently elevated. • Primary hypertension (aka essential or idiopathic hypertension) is when there is no identifiable cause. • Secondary hypertension is high pressure that is due to an underlying cause such as: Kidney problems, adrenal gland tumors, thyroid problems Certain defects in blood vessels you're born with (congenital) Certain medications, such as birth control pills, cold remedies, decongestants, over-the-counter pain relievers and some prescription drugs Illegal drugs, such as cocaine and amphetamines Alcohol abuse or chronic alcohol use Obstructive sleep apnea Human Anatomy & Physiology P. Wilson 31 VI. 13.5 Blood Pressure Some of the consequences of prolonged hypertension: • the left ventricle is required to work harder, which can result in thicker myocardium – enlarging the heart. If the coronary arteries cannot supply sufficient blood to support the overgrowth, parts of the heart muscle may die & be replaced with fibrous tissue • the development of atherosclerosis which may cause coronary thrombosis or coronary embolism • Stroke (aka CVA – cerebral vascular accident) Human Anatomy & Physiology P. Wilson 32