Microbiology in Infection Prevention
advertisement

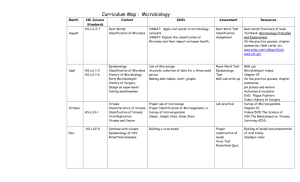
Microbiology in Infection Prevention Leslie Teachout MT (ASCP), CIC Riverton Memorial and Lander Regional Hospitals Infection Prevention Objectives • Discover and discuss the importance of the infection preventionist and microbiology working as a team. • Learn a basic understanding of microbiology and how it helps infection preventionists. • Discuss and interpret the antimicrobial susceptibility report and the antibiogram. Specimen Collection • Get a good specimen to Get good result! • Is very important! The Basics • Bugs are small – 2-5 microns or (106 meters) – Viruses are even smaller – nanometers (109) Classification based on three things – Shape – Gram Reaction – Growth requirements Shape Gram stain process There are four basic steps of the Gram stain: 1. Primary stain with crystal violet to a heatfixed smear of a bacterial culture 2. Followed by the addition of a trapping agent Gram's iodine 3. Rapid decolorization with alcohol or acetone 4. Counterstaining with safranin Gram stain Using Gram stain information!! • Gives a quick look at the specimen – Presumptive identification • Can interpret quality of specimen – Number of “pus” (polymorphonuclear) cells present Using Gram stain information (cont.)!! • Number of epithelial cells present – Surface • Number of bacteria present – Normal vs. abnormal Why the Gram Stain is important!!!! • Can help direct antibiotic therapy – Based on cell wall composition • Not so helpful if lots of normal flora present – Throats, stool, decubital ulcers • QUITE significant on sterile body sites – CSF, blood, urine and other fluids – Assists in the interpretation of culture results Other Stains Acid fast stain is another process. Tuberculosis can not be seen in a gram stain. Normal Respiratory Flora • • • • Oral anaerobes Streptococci species Neisseria species Haemophilus species Respiratory Tract Infections • • • • • Is this a sterile body site? Streptococcus pneumoniae Klebsiella pneumoniae Staphylococcus aureaus Haemophilus influenzae NORMALLY STERILE SITES IN THE HUMAN BODY: Colonization of one of these sites generally involves a defect or breach in the natural defenses that creates a portal of entry • Brain; Central nervous system • Blood; Tissues; Organ systems • Sinuses; Inner and Middle Ear • Lower Respiratory Tract: Larynx; Trachea; Bronchioles (bronchi); Lungs; Alveoli • Kidneys; Ureters; Urinary Bladder; Posterior Urethra • Uterus; Endometrium (Inner mucous membrane of uterus ); Fallopian Tubes; Cervix and Endocervix Never Normal Flora • Mycobacterium tuberculosis • Legionella species • Brucella species • Growth in a sterile body fluid Growth requirements What is Bacterial Growth Media? • A growth media is a mixture of nutrients, moisture and other chemicals that bacteria need for growth. Media are used to grow bacterial colonies Using Media to Identify Bacteria Like the differential staining of bacteria, special types of media can be used to provide clues about a microbe’s identity. There are many types of media that are specific about what they grow, or that provide information about the type of microbes present MRSA on Chromagar Typical Appearance of microorganisms Methicillin Resistant Staphylococcus aureus (MRSA) → rose to mauve Methicillin Susceptible Staphylococcus aureus (MSSA) → inhibited Other bacteria → blue, colorless or inhibited Hemolysis: complete lysis of RBCs Other identification requirements • Oxygen requirements • Ability to ferment or oxidize sugars to produce acid end products • Temperature ranges • Salt tolerance • Chemical tolerance • Enzymes • Motility Gram Positive or Gram Negative bacteria Catalase • Tests the organism’s ability to liberate oxygen from hydrogen peroxide • If it bubbles it staphylococci Coagulase • The ability of the organism under study to clump, clot or coagulate rabbit plasma. – Can use plasma or latex particles • Used as main identification of Staphylococcus aureus, distinguishing it form other Staph. species Coagulase test results Coag positive Staph aureus Coag. Negative Staph epi Basic Growth Times • Most human pathogens take 18-24 hours to grow enough on media to be visible and to be able to distinguish single colonies with the naked eye • Sensitivity testing from a pure culture can be anywhere from 4-24 hours later. • Full identification can take 24 to 48 hours. Pathogens in urine • Is urine a sterile fluid? – Escherichia coli or E. coli – Enterococcus faecalis – Proteus species – Klebsiella Pneumoniae – Enterobacter species Other Pathogens: • Skin and wound – Steptococcus – Staphylococcus • Gastroenteritis – Salmonella – Shigella – Campylobacter species Other Frequently Isolated Organisms (Seldom Pathogens) • Diphtheroids • Propionibacterium • Bacillus species Sensitivity Testing • Basically expose organism to antibiotic and see if it kills the bug. – Antibiotic impregnated discs – Micro-wells to which an organism suspension is added – Take 4-24 hours National excepted criteria for zone size Sensitivity Example Escherichia coli Pseudomonas aeruginosa Enterobacter spp. Klebsiella spp. 1131 Staphylococcus aureus (incl MRSA) Methcillin Resistant S.aureus Staphylococcus coag neg 585 72 92 51 176 29 75 82 68 87 47 Enterococcus faecalis Streptococcus pneumoniae meningeal susceptible non-meningeal susceptible Streptococcus agalactiae (Grp B) "viridans" Streptococcus ssp. 166 64 74 97 92 110 62 8 217 0 87 97 97 92 93 97 88 92 86 95 100 86 82 89 95 96 85 99 96 96 95 99 84 98 17 100 97 96 8 49 100 100 100 100 50 96 98 100 99 97 87 99 90 92 98 100 98 64 0 96 97 99 94 98 98 78 62 98 8 99 79 73 100 99 70 10 30 100 100 0 0 72 100 100 64 35 81 96 100 100 Vancomycin Tobramycin 79 Trimethoprim/Sulfa Tetracycline Rifampin Streptomycin (synergy) Quinupristin/Dalfopristin Piperacillin/Tazobactam Piperacillin Penicillin G Oxacillin Nitrofurantoin Linezolid Levofloxacin Imipenem Gentamicin (synergy) Gentamicin Clindamycin Erythromycin Ciprofloxacin Cefuroxime-parenteral Cefuroxime-oral Ceftriaxone Ceftazidime Cefepime Cefazolin Aztreonam Ampicillin/Sulbactam Ampicillin # of isolates tested Antibiograms 92 99 95 99 100 99 96 98 100 100 71 93 100 98 82 26 100 88 56 97 59 77 73 100 44 44 100 100 100 67 100 98 87 33 46 100 70 79 57 - Values are expressed in % susceptible - Shaded areas indicate that the antimicrobial was not tested against the organism, is not appropriate to report, or is a limitation of the test methods used. - % susceptible results for clindamycin on staphylococcus, Group B strep, and beta-hemolytic strep have been corrected to reflect isolates that demonstrated inducible clindamycin resistance - H.influenzae is only tested for beta-lactamase production; 89% of the isolates tested were beta-lactamase negative (ampicillin susceptible) penicillin Beta-lactam/Beta-lactamase inhibitor combination monobactam cephem fluoroquinolone lincosamide macrolide aminoglycoside carbapenem oxazolidinone nitrofurantoin streptogramin ansamycin tetracycline folate pathway inhibitor glycopeptide Antimicrobial Resistance Prevention and Control: • New drug development • Management of antimicrobial use • Surveillance • Periodic preparation and dissemination of institutional resistance patterns • P&T Committee team work Daily Micro Review • Culture source – Wounds - check previous admissions – Throats and vaginal cultures tend not to be hospital acquired (check admission date) • Location of the patient • Admission date • Culture date is this more than 24 hours from admission Positive Blood culture, Is follow up needed? Wound culture to follow up on: How to handle this information? • Spinal fluid with gram negative cocci – Is this a sterile body site? – Is this organism at pathogen or potential pathogen? Mycobacterium AFB stain • Does not stain with Gram’s Stain • Staining process uses carbol fushsin, slide is heated, then decolorize with HCI and alcohol for 5 minutes – Acid fast (AFB-bacillus) – Retain red color Mycobacterium • M. Tuberculosis (MTb) is a human pathogen • M. avium-intracellularae (MAI)in HIV patient • Divide once every 24 hours – 2-8 weeks for visible colonies • Some environmental species – M. gondonae – M. marinum What is a virus? • Viruses are not like bacteria! • Viruses are not like bacteria! • Viruses DO NOT “grow” or divide • Viruses make copies of themselves using: – Tools like enzymes or proteins they code – Using cell machinery – May target specific cells like the liver What is a Virus? • Obligate intracellular parasite • NOT a cellular organism – No organelles or – ribosome, energy-less • Not Free-living – Completely dependent on host cells Viruses • Enveloped – Easiest to kill, less hardy • Non-enveloped – Hardy, resistant to lower concentration of alcohol • Both DNA and RNA viruses • Test is generally sent to a reference lab Yeasts • Single cell organisms • Numerous species – Candida albicans • Opportunistic – Can be normal respiratory flora Sporulation Host Exit Spore state Disease Host Entry The life cycle of Clostridium difficile Toxin Production Germination Vegetative state Reproduction Adapted from description in Paredes-Sabja, D., Bond, C., Carman, R. J., Setlow, P. & Sarker, M.R. (2008). Germination of spores of Clostridium difficile strains, including isolates from a hospital outbreak of Clostridium difficile-associated disease (CDAD). Microbiology, 154, 2241-2250. Pathogen factors • • • • Strain type Antibiotic resistance Sporulation rates Toxin regulation Hypervirulent NAP1 “This is a specific strain of C. difficile that emerged first in North America, in Pennsylvania. This NAP1 strain has a genetic change that results in literally 16 to 23 times more toxin production in vitro,” explains William Jarvis, MD Last Thoughts • The names may change but the bugs stay the same • Get a good specimen to Get good result! Objectives • Discover and discuss the importance of the infection preventionist and microbiology working as a team. • Learn a basic understanding of microbiology and how it helps infection preventionists. • Discuss and interpret the antimicrobial susceptibility report and the antibiogram. Thank You • Any questions??