Richard Aguilar 3 - National Hispanic Medical Association
advertisement

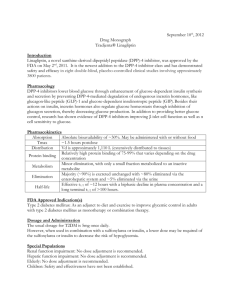
Efficacy and safety of linagliptin in Hispanic/Latino patients with type 2 diabetes: a pooled analysis from six randomized placebo-controlled phase 3 trials Jaime A. Davidson1, Rosemarie Lajara2, Richard Aguilar3, Michaela Mattheus4, Maximilian von Eynatten4 1University of Texas Southwestern Medical Center, Dallas, TX, USA; 2Diabetes America, Plano, TX, USA; 3Diabetes Nation, Sisters, OR, USA; 4Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany; 5Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, CT, USA 18th National Hispanic Medical Association’s (NHMA) Annual Conference; 27-30 March 2014; Washington, D.C. Author disclosure information This study was supported by Boehringer Ingelheim Pharmaceuticals, Inc. (BIPI) Richard Aguilar: advisory panels and speaker’s bureau for Boehringer Ingelheim, Amylin, Eli Lilly, Takeda, Novo Nordisk, and Janssen Pharmaceuticals; consultant for Boehringer Ingelheim, Amylin, and Takeda Jaime Davidson: advisory panels for Boehringer Ingelheim, AstraZeneca, Bristol-Myers Squibb, Johnson & Johnson Lifescan, Merck-Sharp & Dohme, Roche, Allergan, Janssen Pharmaceuticals, Roche Diagnostics; advisory panels and speaker’s bureau for Sanofi, Novo Nordisk, Eli Lilly; speaker’s bureau for Merck-Serono and Novartis; consultant for Animas Rosemarie Lajara: scientific advisor for Eli Lilly and Dexcom; scientific advisor and speaker’s bureau for Boehringer Ingelheim, Novo Nordisk, and Sanofi; speaker’s bureau for Amylin, AstraZeneca, and Abbott Michaela Mattheus and Maximilian von Eynatten are employees of Boehringer Ingelheim The authors were fully responsible for all content and editorial decisions, were involved at all stages of slide development, and have approved the final version Medical writing assistance during the preparation of these slides was supported financially by BIPI and provided by Ann Kerrigan of Envision Scientific Solutions Portions of these data were previously presented at the American Association of Clinical Endocrinologists (AACE) 22nd annual meeting, May 1-5, 2013, Phoenix, AZ, USA Global diabetes epidemic Diabetes caused 5.1 million deaths in 2013. Every six seconds a person dies from diabetes IDF Diabetes Atlas, 6th Edition (2013) % of people aged ≥20 years Proportion of adults with diagnosed diabetes: US national survey data 2007-2009 15 11.8 10 Risk was 66% higher among Hispanics 7.1 5 0 Non-Hispanic whites Hispanics Hispanic/Latinos also at increased risk of diabetes-related complications and mortality A combination of genetic, socioeconomic, and cultural factors underlie the increased diabetes burden in this group Evidence for the efficacy and safety of glucose-lowering agents in this group is scarce National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011. Linagliptin Dipeptidyl peptidase (DPP)-4 inhibitor with a unique xanthine-based structure1 – Glucagon-like peptide (GLP)-1 is an incretin hormone released from the gut in response to food – GLP-1 mediates glucose-dependent insulin release and glucose-dependent glucagon suppression – DPP-4 inhibitors block the degradation of GLP-1, thereby increasing endogenous GLP-1 levels – and lowering blood glucose level Linagliptin is a highly selective DPP-4 inhibitor and has been shown to have the highest potency within its class Linagliptin does not undergo major hepatic metabolism and is mainly excreted unchanged via bile and gut1,2 Once-daily dosing with no dose adjustment in renal or hepatic impairment2 Improves glucose control with very low risk of hypoglycemia and neutral effect on body weight2 1 2 Deacon and Holst. Expert Opin Investig Drugs. 2010;19:133-140 Tradjenta. US prescribing information. Revised June 2013 Hypothetical case-based question Martina is a 44-year-old mother of Mexican origin raising 2 teenagers while working part-time. She was diagnosed with type 2 diabetes at 40 and has been treated with metformin 500 mg BID since then. She is 5’1” and weighs 164 lbs. (BMI 31 kg/m2). Her blood pressure is 120/80 on Lisinopril 20 mg once daily. She states that she has been busy; she does not have time to eat properly like she should, and that the metformin sometimes upsets her stomach. She also notes that she sometimes forgets her evening metformin dose. She tried adding some “yerba buena’’ tea from Mexico to help control her “sugars” and she is here today for a check-up; her HbA1c is 8.3%, essentially unchanged from her results 3 months earlier, 8.4%. What therapy changes would you recommend for Martina’s T2D? A. None, continue metformin and refer for diabetes education B. Increase metformin dose C. Add a DPP-4 inhibitor D. Add a sulfonylurea E. Add an SGLT-2 inhibitor Safety and efficacy of linagliptin in Hispanic/Latino patients with T2D 1 Analysis approach: pooled analysis of Phase 3 RCT Monotherapy (18 wks) Barnett et al. Diabetes Obes Metab. 2012 2 Monotherapy (24 wks)* Haak et al. Diabetes Obes Metab. 2012 3 Add-on to metformin (24 wks) Taskinen et al. Diabetes Obes Metab. 2011 4 Add-on to sulfonylurea (18 wks) Lewin et al. Clin Ther. 2012 5 Add-on to metformin + sulfonylurea (24 wks) Owens et al. Diabet Med. 2011 6 Add-on to basal insulin ± metformin and/or pioglitazone (24 wks) Data from 745 patients (who selfidentified ethnicity as Hispanic or Latino) were pooled from six phase 3 trials in which participants received linagliptin (5 mg/day) or placebo as monotherapy, or in combination with other common oral antidiabetes drugs (as stable background therapy) Yki-Järvinen et al. Diabetes Care. 2013 Primary endpoint in all studies HbA1c change from baseline to week 18 or 24 * Patients were assigned to 1 of 6 treatment arms, including initial combination therapy. Only linagliptin monotherapy and placebo arms were included in this analysis Baseline characteristics Linagliptin Placebo 478 267 Sex, n (%) Male Female 213 (44.6) 265 (55.4) 117 (43.8) 150 (56.2) Country, n (%) Argentina Brazil Canada Mexico Peru United States 271 (56.7) 22 (4.6) 3 (0.6) 126 (26.4) 3 (0.6) 53 (11.1) 155 (58.1) 25 (9.4) 0 (0.0) 49 (18.4) 2 (0.7) 36 (13.5) Age, years, mean (SD) 57.4 (10.0) 56.8 (9.7) BMI, kg/m2, mean (SD) 30.3 (5.0) 31.4 (4.6) 467 264 HbA1c, %, mean (SD) 8.25 (0.85) 8.23 (0.92) FPG, mg/dL, mean (SD) 161.4 (46.3) 156.1 (44.4) 24 (5.1) 125 (26.8) 318 (68.1) 19 (7.2) 57 (21.6) 188 (71.2) Patients, n (treated set) Patients, n (full analysis set) Time since diagnosis, n (%) ≤ 1 year > 1 to 5 years > 5 years Change in HbA1c (%) over time (18-week data set) Adjusted mean change (95% CI): −0.63 (−0.77, −0.48) P<0.0001 Data based on six clinical trials. Full analysis set, last-observation carried forward. Analysis of covariance model included continuous baseline HbA1c and fixed effects for treatment, study, and washout. The OBSMARGIN option was used for the computation of least squares means coefficients. Change in HbA1c (%) at 24 weeks Data based on four clinical trials. Full analysis set, last-observation carried forward. Analysis of covariance model included continuous baseline HbA1c and fixed effects for treatment, study, and washout. The OBSMARGIN option was used for the computation of least squares means coefficients. Placebo-adjusted mean change in HbA1c in different subgroups Full analysis set, last-observation carried forward. Interactions of treatment-by-subgroup were added to the ANCOVA and an equal weighting option was used for the computation of least squares means coefficients. Safety (treated set) Linagliptin (n=478) Placebo (n=267) Any adverse event (AE), % 67.6 68.9 Investigator-defined drug related AE, % 15.1 18.7 AE leading to discontinuation, % 2.1 3.0 Serious AE, % Fatal Drug-related serious AE 3.6 0.2 0.4 3.0 0.0 0.4 Two patients who received linagliptin experienced a serious AE that was considered related to the study drug (one case of bronchial hyperactivity and one case of pancreatitis) A single patient in the linagliptin arm died due to cardiorespiratory arrest. The cause of death was judged unrelated to study drug Linagliptin and placebo were both weight neutral (adjusted means [SE] at week 24: 0.37 [0.15] kg and 0.21 [0.21] kg, respectively [P=0.5454]) Hypoglycemia (treated set) Two patients experienced severe hypoglycemia with linagliptin (both patients were also receiving insulin and both patients recovered) Study conclusions Linagliptin in Hispanic/Latino patients was well tolerated and achieved clinically meaningful improvements in glycemic control − Overall efficacy results were consistent among clinically relevant subgroups of patients − Overall, linagliptin was not associated with an increased risk of hypoglycemia and was weight neutral Together, the above observations support the use of linagliptin as a treatment option for this highly burdened population Hypothetical case-based question Martina is a 44-year-old mother of Mexican origin raising 2 teenagers while working part-time. She was diagnosed with type 2 diabetes at 40 and has been treated with metformin 500 mg BID since then. She is 5’1” and weighs 164 lbs. (BMI 31 kg/m2). Her blood pressure is 120/80 on Lisinopril 20 mg once daily. She states that she has been busy; she does not have time to eat properly like she should, and that the metformin sometimes upsets her stomach. She also notes that she sometimes forgets her evening metformin dose. She tried adding some “yerba buena’’ tea from Mexico to help control her “sugars” and she is here today for a check-up; her HbA1c is 8.3%, essentially unchanged from her results 3 months earlier, 8.4%. What therapy changes would you recommend for Martina’s T2D? A. None, continue metformin and refer for diabetes education B. Increase metformin dose C. Add a DPP-4 inhibitor D. Add a sulfonylurea E. Add an SGLT-2 inhibitor BACKUP Study design Assessment of eligibility Treatment-naïve patients / patients pre-treated with a permitted antidiabetic agenta 2 week placebo run-in Patients pre-treated with nonpermitted antidiabetic agents 4 weeks washout followed by 2 weeks placebo run-in Assessment of eligibility Randomizationb Linagliptin 5 mg a Permitted Placebo antidiabetes agents: metformin (NCT00601250), metformin + sulfonylurea (NCT00602472), sulfonylurea (NCT00819091), basal insulin ± metformin and/or pioglitazone (NCT00954447). b NCT00798161, patients were randomized to 1 of 6 treatment arms, but only Hispanic/Latino patients from the linagliptin and placebo arms were pooled for these analyses Statistical methods Efficacy analyses were performed on the full analysis set, including all patients with a baseline value and ≥1 on-treatment value; missing data were replaced using last observation carried forward (LOCF) The primary analysis used analysis of covariance (ANCOVA) to compare change in HbA1c and FPG for the linagliptin and placebo groups, with continuous baseline HbA1c and fixed effects for treatment, study, and washout. The FPG model also included continuous baseline FPG. The OBSMARGIN option for the computation of LSMEANS was used For subgroup analyses the effect of subgroup and the interaction of treatmentby-subgroup were added to the ANCOVA. An equal weighting option for the computation of LSMEANS was used Antidiabetes treatment at enrollment, n (%) Linagliptin n=467 Placebo n=267 No treatment 20 (4.3) 16 (6.1) Metformin 70 (15.0) 20 (7.6) Sulfonylurea 35 (7.5) 16 (6.1) Alpha-glucosidase inhibitor 1 (0.2) 0 (0.0) Insulin 29 (6.2) 26 (9.8) 216 (46.3) 73 (27.7) Metformin & glinide 1 (0.2) 0 (0.0) Metformin & DPP-4 inhibitor 4 (0.9) 1 (0.4) Metformin & insulin 79 (16.9) 98 (37.1) Glitazone & insulin 2 (0.4) 3 (1.1) Metformin, sulfonylurea, & alpha-glucosidase inhibitor 1 (0.2) 0 (0.0) Metformin, glitazone, & insulin 9 (1.9) 11 (4.2) Metformin & sulfonylurea Adjusted mean change in FPG and PPG at 24 weeks FPG Data based on four clinical trials. Full analysis set, last observation carried forward. ANCOVA model included continuous baseline HbA1c and FPG, and fixed effects for treatment, study, and washout PPG Data based on a subset of patients of one clinical trial Pancreatitis T2D increases the risk of acute pancreatitis Postmarketing reports of acute pancreatitis, including fatal pancreatitis, have been reported for DPP-4 inhibitors. The Warnings and Precautions section of DPP-4 inhibitor drug labels contain warnings about the risk of acute pancreatitis In the clinical trial program, pancreatitis was reported in 15.2 cases per 10,000 patient year exposure while being treated with linagliptin, compared with 3.7 cases per 10,000 patient year exposure while being treated with comparator (placebo and active comparator, sulfonylurea). Three additional cases of pancreatitis were reported following the last administered dose of linagliptin (US prescribing information) An observational study demonstrated a significantly increased risk of acute pancreatitis with GLP-1 based therapies. However, data from randomized controlled trials and meta-analyses have not shown any increase in the incidence of acute pancreatitis with DPP-4 inhibitors These results must be confirmed by ongoing large cardiovascular outcomes trials – No increased risk of pancreatitis or pancreatic cancer in two recently completed DPP-4 inhibitor trials [Scirica BM, et al NEJM 2013; White WB, et al. NEJM. 2013] An FDA review is ongoing. For now, ‘’FDA believes that the current labeling for approved GLP-1 based therapies reflects the extent of our understanding of the safety signals at this point in time’’ (Lisa Kubaska, FDA, CDER; http://www.medscape.com/viewarticle/808830) For a comprehensive review and discussion of the evidence see: Scheen A. Expert Opinion on Drug Safety, 2013