Paper - ILPC
advertisement

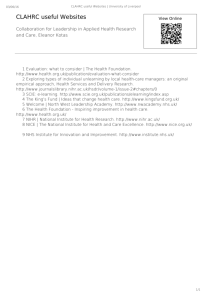
NOT FOR CIRCULATION OR QUOTATION WITHOUT EXPRESS PERMISSION FROM AUTHORS This paper draws on work co-funded by an organisation* that requires 28 days sight of papers prior to general release. Permission for full paper release is being requested but, in the meantime, we hope that the following section will be a useful guide to the arguments within the full paper. *The funder is the National Institute of Health Research (NIHR). This paper represents the views of the authors and not necessarily those of the NIHR or the co-funding healthcare organisations. Losing control? The implications for GPs of national and local performance measurement systems McBride, A., Kislov, R. and Spence M., Manchester Business School Introduction Harrison (2009:192) argues that the transformation of UK doctors into technicians with an increased susceptibility to outside control is a ‘likely direction of travel’. Three dynamics are cited by Harrison (2009:193) as underpinning this trajectory: Conceptual commodification of healthcare; the internalisation of pay-for-performance measures in primary care; and the potential for an emerging medically qualified ‘administrative elite’ (Freidson 1994 as cited in Harrison 2009). This paper explores the dynamics of this potential direction of travel in primary care in England. Successive Governments have been keen to standardize clinical care by General Practitioners (GPs) in the National Health Service (NHS) as they are deemed to have the largest potential impact on public health – both as treatment providers within their communities and as gatekeepers to more expensive aspects of secondary care. This has taken considerable time given that GPs operate as independent contractors but, in 2004, management established a classification system that identified aspects of clinical and organizational quality that could be measured and used as pay-for-performance indicators (Harrison, 2009: 191). Called the ‘Quality and Outcomes Framework’ (QOF), this system has NOT FOR CIRCULATION OR QUOTATION WITHOUT EXPRESS PERMISSION FROM AUTHORS incentivised GPs to keep registers of patients with targeted diseases and has increased their compliance with clinical guidance (McDonald et al, 2007). In addition to QOF introduced as a top-down, country-level system, a less explicit strategy has been the more localised, bottom-up use of service improvement (SI) initiatives at the level of individual healthcare organisations around particular (prescribed) care regimes, patient pathways and disease-programmes (Kitchener and Exworthy, 2008). These service improvements bear the hallmarks of performance management, for example, using information and communication technologies (ICTs) to quantify observations, provide feedback and identify the level of change required. Such initiatives themselves are not new, clinicians have been involved in a number of reflective exercises over time – it is the context in which these initiatives have been introduced that has changed. For example, in the 1980s, the medical profession was expected to become systematically involved in medical audit, such that they could identify variations in practice (from agreed standards) and effect change (Department of Health 1989). There is considerable distance, however, between the context in which fledgling medical audit practices evolved in the 1980s and ‘90s (McBride 1992; Exworthy 1998) and the more tightly regulated terrain of the present. Indeed, Waring et al (2010) argue that the presence of regulatory activities that specify the content of medical work and enable the supervision of its performance is indicative of a move from “state-sanctioned, collegial, self-regulation to a form of regulation that can be understood as state-directed bureaucratic regulation” (551). They (Ibid: 541) reach this conclusion by using Black (2001) to understand regulation as, “the sustained and focused attempt to alter the behaviour of others according to defined standards or purposes with the intention of producing a broadly identified outcome or outcomes, which may involve mechanisms of standard-setting, information-gathering and behaviour modification.” The mode through which the state, and management, seek to regulate GPs, however, is emerging ‘uneasily’ (Kitchener and Exworthy 2008:219) and whereas opportunities may be exploited to facilitate a ‘panoptic surveillance’ of the medical profession (Ibid. :218), sufficient tensions exist within the system to ensure that GPs retain a degree of ‘regulated autonomy’. For example, it remains difficult for non-experts to routinely review and regulate medical performance (Waring et al 2010:549) and protocols and guidelines do not reach universal adoption (Kilminster et al 2010). In addition, whilst some control of GP work NOT FOR CIRCULATION OR QUOTATION WITHOUT EXPRESS PERMISSION FROM AUTHORS arguably transferred to an emergent administrative elite of GPs within Primary Care Trusts (PCTs) (Kitchener and Exworthy 2008:220), PCTs themselves have since been disbanded, with Clinical Commissioning Groups (CCGs) emerging as the ‘new kid on the block’. Irrespective of this organisational restructuring, however, previous work has tended to either look at changing behaviour as a result of centrally-derived performance measures (eg Exworthy et al 2003; McDonald et al 2007) or service improvement (Braithwaite et al., 2011; Davies et al., 2007; Fitzgerald et al., 2013; Foy et al., 2005; Grimshaw et al., 2006; Kislov et al., 2012). We still need to know how GPs respond to this two-pronged strategy to regulate their work. By looking at this during a period of organisational change, we can also see whether (and how) organisational changes mediate these responses. Participation in, and observation of, one of the nine NIHR (National Institute of Health Research) CLAHRCs (Collaboration for Leadership in Applied Health Research and Care)1 enables us to do address some of these questions. Established across England in 2008 (NIHR 2010), and bringing together academic institutions, NHS healthcare providers and commissioners over a five-year period, CLAHRCs aim to create innovative ways of ensuring clinical research is put ‘into practice’, eg the co-production of research that more obviously meets the needs of practitioners; the development of research-oriented practitioners; the facilitation of research implementation through the application of service improvement and implementation science ‘in the field’. By providing funding solely on the basis of co-funding by local NHS organisations, the NIHR sets up the potential for local CLAHRCs to develop collaborative working between research academics and practitioners, as each has a vested interest in determining the CLAHRC agenda. This paper is based on activities of the implementation work stream of a CLAHRC. The implementation stream of this particular CLAHRC has the explicit aim of using principles of service improvement and implementation science to facilitate the implementation of evidence based research in practice. This work shares common themes with medical audit, particularly in its ultimate aim to effect real changes in practice. Three major contextual differences are apparent, however, in comparison to the gentler introduction of medical audit in the 1980s, with each difference arguably facilitating the closer binding of national 1 CLAHRCs are a collaboration between NHS healthcare organisations and academic institutions and are part of NIHR NOT FOR CIRCULATION OR QUOTATION WITHOUT EXPRESS PERMISSION FROM AUTHORS and local performance measures, and thereby enabling closer control of the GP. Usefully, each contextual difference can be illustrated through the three stages of the basic audit cycle. The first stage requires the setting of standards and who sets the standards, and how, has changed over time. In the past practitioners determined their own local standards against which to audit themselves, whereas now there exist national and, indeed, European standards against which to judge practice. Harrison (2002:192) indicates the proliferation of clinical guidelines intended to govern the treatment of entire categories of patients as being the development of ‘scientific-bureaucratic medicine’. When added to the assumption that cases within a category are ‘fundamentally homogenous’ (Harrison 2009:192), we can see how the setting of standards by external bodies could make it easier for managers to be ‘more easily able to control medical work’ (Ibid: 192). This potential grows with contextual changes at the second stage of the audit cycle: the observation of practice. We see two changes here. First, there has been an increased sophistication in the manner in which ICTs can be used to record numerous components of practice. Second, there is increased capacity of ICTs to provide clear, visual displays of comparative practice – both in relation to clinical guidelines (ie what variation exists between standards and practice) and across GP Practices (ie what variations exist across GP practices). It is the third, and final, stage of the audit cycle (effecting change), however, where contextual changes provide the greatest pressure for GPs to change their practice. In the past regime of self-regulation, it was ‘hoped’ that peer discussion of variations of practice from standards would result in changes of practice and a ‘closing of the loop’ that would be apparent in re-audits. The modernisation of medical regulation to address medical scandals and bring closer alignment with ideals of market liberalisation (Waring et al 2010) has, on the one hand, provided more power to external bodies to become interested in such activities and, on the other, provided financial incentives (such as QOF) for GPs to change. If the wider question is seeking evidence of the transformation of UK doctors into technicians with an increased susceptibility to outside control (Harrison 2009), or at the very least their responses to the evolution of a ‘state-directed bureaucratic regulation’ (Waring et al 2010), then CLAHRC enables us to address this through the study of two SI audit and NOT FOR CIRCULATION OR QUOTATION WITHOUT EXPRESS PERMISSION FROM AUTHORS feedback interventions deploying ICTs to collect, analyse and present the data measuring the accuracy of chronic disease registers in primary care. First, using Waring et al’s (2010:540) definition of regulation, we have chosen two SI interventions that have led to changed behaviour and outcomes in GP practices that were desired by others. We then look more specifically at what was happening at each stage of the audit cycle and examine how this intervention could be considered a sustained and focused attempt to alter the behaviour of GPs. So for example, at the first stage, we indicate the process through which standards are determined, for whom and by whom, and how they are linked to financial incentives and commissioning decisions. At the second stage, we identify the manner in which practice was observed and re-presented to the GPs. Lastly we examine the manner in which GPs were encouraged to change and how they changed. In summary, the authors examine the extent to which the alignment of these lower level SI audit and feedback interventions with national level incentives, such as QOF, leaves GPs susceptible to greater regulation from outside the profession.