Fungal Infections of the skin Superficial and cutaneous
advertisement

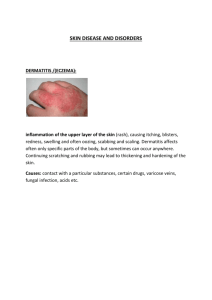
Skin fungal infections Clinical Skin fungal infections are generally divided into Superficial Tinea versicolor, Piedra (Trichosporosis), and Tinea nigra Cutaneous Dermatophytosis, Candidiasis of skin, mucosa, nails and others Subcutaneous Mycetoma, Sporotrichosis, Chromoblastomycosis, and others Superficial Mycoses Defined as infections in which a pathogen is restricted to the Stratum corneum, with little or no tissue reaction These affect the uppermost dead layers of skin or hair shaft They are painless and usually do not provoke the immune system They include 1- Tinea versicolor 2- Tinea nigra 3- Piedra Tinea Versicolor Tinea versicolor is a long-term (chronic) fungal infection of the skin The fungus interferes with the normal pigmentation of the skin resulting in small, discolored patches The most common sites The back, underarms, upper arms, chest, and neck Tinea versicolor occurs most frequently in teens and young adults Sun exposure may make tinea versicolor more apparent Tinea versicolor often recurs, especially in warm, humid weather Clinical presentation: Tinea versicolor is a type of infection of the keratinized epithelial cells in the stratum corneum. Hypo- or hyperpignented macules on chest or back. The infection causes patches of discolored skin that may be: Colored white, pink, tan or dark brown Slow-growing, scaly and mildly itchy More noticeable after sun exposure Causes The fungus that causes Tinea versicolor can be found on healthy skin (normal flora of skin). It only starts causing problems when the fungus overgrows A number of factors may trigger this growth, including: Hot, humid weather Excessive sweating Oily skin Hormonal changes Weakened immune system Malassezia furfur, and Malassezia globosa It is a Yeast Lipophilic Normal flora of skin Diagnosis Skin scraping Potassium hydroxide (20% KOH) Positive for short hyphae and yeast cells Spaghetti and meatballs Culture Malassezia furfur Oil should be added to the media Pityriasis versicolor commonly causes hypopigmentation in people with dark skin tones Superficial Mycoses Tinea nigra: Superficial fungal infection Causes dark brown to black painless patches (macule) on the palms of the hands and the soles of the feet. This infection is caused by the fungus formerly classified as Exophiala werneckii More recently classified as Hortaea werneckii Skin scrapings In 10% or 20% KOH will show brown septate hyphae The KOH lyses the nonfungal debris Culture on SDA & Mycobiotic Agar plate with the dominant fungi in the salterns, the black yeast Hortaea werneckii Diagnosis produce melanin in their cell walls Micrograph of the fungus Hortaea werneckii growth of dematiaceous fungus Superficial Mycoses - Piedra Asymptomatic infection of the hair shaft, causing nodules on the hair shaft On scalp hair, and other body hair. Black piedra (Exothrix infection) Piedraia hortae Dark pigmented nodules Hard and firmly attached to hair shaft White piedra( Endothrix infection) Trichosporon beigelii Lightly pigmented, white to brown nodules Soft, loosely attached N Laboratory diagnosis 1. Clinical Material 2. Direct Microscopy Hairs should be examined using 10% KOH White piedra Epilated hairs with white soft nodules present on the shaft Sabouraud's dextrose agar (SDA) Hair with black Piedra 3. Culture Treatment of Superficial infections 2% salicylic acid 3% sulfur ointments Whitfield's ointment Ketoconazole Piedra Cutting or shaving the hair Or apply 2% salicylic acid Or 3% sulfur ointment Nizoral shampoo (contains Ketoconazole) Antifungal agents Topical Dermatophytosis Fungal infections of the Keratinized tissues of the body (mainly: Stratum corneum, Skin epidermis, and dermis could be involved). Scalp, glabrous skin, and nails caused by a closely related group of fungi known as dermatophytes They are primary pathogens Contagious Direct contact between infected humans or animals (goats, sheep, camel, cows, horses) Transfer form one area of the body to another Familial cross infection occurs Tinea (Ringworm): Classified according to site of inf: T. capitis scalp T. corporis glabrous (body) skin T. pedis foot (Athlete’s foot) T. cruris groin Dermatophytes Etiology A group of related fungi called dermatophytes (filamentous fungi; septate hyphae and conidia): Microsporum infections on skin and hair Epidermophyton infections on skin and nails Trichophyton infections on skin, hair, and nails Keratin - utilizing on hosts - humans Tinea Capitis Ringworm of the scalp (Tinea capitis) is a fungal infection of the scalp hair and epidermis. Highly contagious infection most common in toddlers and school-age children Treatment for ringworm of the scalp includes medications taken by mouth medicated shampoo Some cases of ringworm of the scalp result in severe inflammation at the site of infection that may cause scarring or permanent hair loss Clinical presentation: Papules are solid raised skin lesions with defined borders (less than 1 cm). One or more round patches (Erythematous papules) of scaly skin where the hair has broken off or just above the scalp. Patches that slowly expand or enlarged in circular appearance Scaly, gray or reddened (inflamed) area. Brittle or fragile hair that easily pulls out Tender or painful areas on the scalp. Tinea capitis Causes Ringworm of the scalp is caused by one of several varieties of mold-like fungi called dermatophytes Microsporum canis or Microsporum gypseum Epidermophyton floccosum. Trichophyton mentagrophytes. Methods of transmission Ringworm is contagious and can spread in the following ways: Human to human direct skin-to-skin contact with an infected person Geophilic species Keratin - utilizing soil saprophytes Object to human: Anthropophilic species clothing, towels, bed linens, combs or brushes Animal to human : Zoophilic species: dogs and cats, especially kittens cows, goats, pigs and horses Complications Kerion Kerion is the result of the host's response to a fungal ringworm infection of the hair follicles of the scalp with secondary bacterial infection. Tests and diagnosis Tests typically include a visual exam Sometimes, you may take a sample of the hair or skin History Close contacts, duration. Morphology of lesion Broken hairs, black dots, localized Woods Lamp Blue green Culture Tinea Capitis - Treatment Must treat hair follicle Topical , but might be not effective Systemic agents Griseofulvin for children – is taken by mouth as a liquid or tablet Side effects Sensitive skin Terbinafine You may prescribe one of these medications for six weeks or more Tinea Corporis - Ringworm (body) Ringworm of the body is one of several forms of ringworm, a fungal infection that develops on the top layer of the skin It's characterized by an itchy, red circular rash with healthy-looking skin in the middle Ringworm gets its name from the characteristic ring that can appear Ringworm on the arm Clinical presentation: A circular rash on the skin that's red and inflamed around the edge and healthy looking in the middle Slightly raised expanding rings of red patches, scaly skin on the trunk or face A round, flat patch of itchy skin Causes Microsporum canis or Microsporum gypseum Epidermophyton floccosum. Trichophyton mentagrophytes; (Micro-and Macroconidia; Lactophenol-cotton blue) Risk factors predisposing for dermatophytosis: Living in humid or crowded conditions Have close contact with an infected person or animal Share clothing, bedding or towels, with fungal infection patient Sweat excessively Participate in contact sports, such as wrestling, football or rugby Wear tight or restricted clothing Have a weakened immune system Complications A fungal infection rarely spreads below the surface of the skin People with weak immune systems, may find it difficult to get rid of the infection Tests and diagnosis You will determine if patient have ringworm or another skin disorder skin scrapings or samples from the infected area and look at them under a microscope a procedure known as a potassium hydroxide (KOH) test If a sample shows fungus, treatment may include an antifungal medication If the test is negative but you still suspects that patient have ringworm, a sample may be sent to the laboratory for testing this test is known as a culture you may also order a culture if condition doesn't respond to treatment Candidiasis (Yeast Infection) Candidiasis is a fungal infection that can affect areas such as the: Skin Genitals, Throat Mouth, Blood. Overgrowth of a type of yeast called Candida, usually Candida albicans Dimorphic fungi that is normally found in human body. Oral Candidiasis (Thrush) A yeast infection of the mouth or throat area is called thrush Healthy adults do not usually get thrush. It is most often seen in: Infants Elderly Patients getting chemotherapy People with AIDS or other conditions that weaken the immune system It can also be seen in people with diabetes in those who take antibiotics asthma inhalers with steroid medication Oral candidiasis in a child Yeast Infection of the Genitals Vaginal yeast infections are common in women. Common symptoms include: Extreme itching in the genital area Soreness and redness in the genital area White, clumpy vaginal discharge Painful intercourse But men can get a yeast infection, too. Symptoms in men include: Red rash on genitals Itching or burning on the tip of the genitals It is important to get treated for a genital yeast infection. You may pass the infection back and forth to a sexual partner Subcutaneous Fungal Infection A-Sporotrichosis: Caused by Sporothrix schenkii. B-Mycetoma (Madura foot): -Localized skin abscess due to granulomatous infection of dermis and subcutaneous tissue. -Caused by: 1-Pathogenic soil fungi: Madurella mycetomatis. 2-Bacteria: Actinomycetoma: Actinomyces species or Nocardia. Subcutaneous Fungal Infection Madura Foot Chromoblastomycosis Sporotrichosis Mycetoma