Superficial Mycoses - INAYA Medical College
advertisement
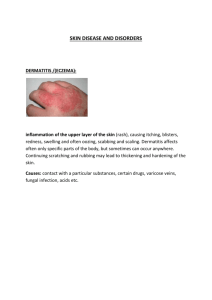
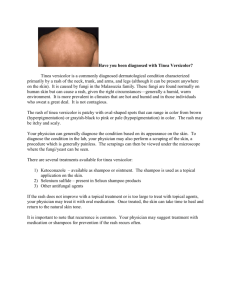
Superficial Mycoses Mrs. Dalia kamal Eldien Msc in Microbiology Lecture NO (4) Objectives Definition of Mycosis Classification of fungal infection according to the tissue levels initially Definition of Superficial mycoses the mode of transmission Causes of non-inflammatory Superficial mycoses introduction Mycosis (plural: mycoses)is fungal infection of animals& humans. Mycoses are classified according to the tissue levels initially colonized to:1-Superficial mycoses 2-Cutaneous mycoses 3- Subcutaneous mycoses 4- Systemic mycoses due to primary pathogens 5- Systemic mycoses due to opportunistic pathogens Superficial mycoses Defined as fungal infections of the skin and hair that invade only the most superficial layers and cause little or no inflammatory response. These fungi have ability to produce keratinase, which allows them to metabolize and live on human keratin tissue like skin, nail and hair. Are a major cause of morbidity in the world, particularly in the tropics, where heat and humidity provide the ideal conditions for the growth of fungi . Direct contact is sufficient to transmit the infection from a contaminated surface or host to another. PATHOGENICITY With superficial mycoses, fungi are confined to the epidermis and annexes, and rarely invade the dermis. In extremely rare cases, internal organs can also be affected. There are two categories of infection: Non-inflammatory infection Inflammatory infections NON-INFLAMMATORY INFECTIONS Infection Causative fungi Malasseziosis Malassezia species Tinea nigra Exophiala werneckii Black piedra Piedraia hortae White piedra Trichosporon species Malasseziosis Also known as pityriasis or tinea versicolor Pityriasis versicolor is a common yeast infection of the skin, in which flaky discoloured patches appear on the chest and back. In people with dark skin tones, pigmentary changes such as hypo pigmentation (loss of color) are common, while in those with lighter skin color, hyper pigmentation (increase in skin color) are more common. The term pityriasis is used to describe skin conditions in which the scale appears similar to bran. The multiple colors of pityriasis versicolor give rise to the second part of the name versicolor. pityriasis Common species • Tinea versicolor is caused by Malassezia globosa Malassezia restricta Malassezia furfur Pathogenicity Pityriasis versicolor is not contagious. Pityriasis versicolor is a rash caused by a yeast-like germ Small numbers of this germ commonly live on the skin, and do no harm. However, some people are prone to this germ multiplying on their skin more than usual, which then leads to a rash developing. Often the germ multiplies and causes the rash for no apparent reason. In some cases, hot, sunny or humid weather seems to trigger the germ to multiply on the skin. The rash usually starts as small pale patches, usually appear on the chest, neck or upper arms. The rash sometimes spreads to tummy (abdomen), thighs and back. Pityriasis versicolor is usually asymptomatic, but in some people it is mildly itchy. These fungi also cause folliculitis (inflammation of the hair follicles) also cause seborrheic dermatitis and dandruff Diagnosis – Pityriasis versicolor is usually diagnosed clinically. However, the following tests may be useful. Wood lamp (black light) examination— yellow-green fluorescence may be observed in affected areas Specimen: skin scraping, skin biopsy Microscopy using potassium hydroxide (KOH)—appearance of oval to round budding yeasts as well as short septate and sometimes branching hyphae that resemble spaghetti and meatballs are observed Fungal culture—this is usually reported to be negative, as it is quite difficult to encourage the yeasts to grow in a lab. Skin biopsy—fungal elements may be seen within the outer cells of the skin on histopathology. Wood lamp examination Septated Hyphae and yeast cell Treatment Mild pityriasis versicolor is treated with topical antifungal agents. Propylene glycol solution Sodium thiosulphate solution Selenium sulfide Topical azole cream/shampoo (econazole, ketoconazole) Tinea nigra Is a superficial fungal infection that causes dark brown to black painless patches on the palms of the hands and the soles of the feet The word Tinea means a fungal infection and Nigra means black. Tinea nigra is overall an uncommon fungal infection when compared to other tinea infections . Tinea nigra is more commonly seen in children and is more likely in girls than boys. The conditions also tends to affect lighter skinned individuals than darker skinned people. The infection is mostly acquired via direct inoculation of the fungus onto the skin due to contact with soil, wood, and decaying vegetation. Clinically, it is characterized by small unilateral, black patches that appear on palmar skin or rarely on plantar skin and the edges of fingers. Tinea nigra does not cause an itchy skin rash . Most patients are unaware of the fungal infection until the characteristic brown to black rash develops. Tinea nigra is a superficial fungal infection caused by one of the following fungi : Exophiala werneckii (Phaeoannellomyces werneckii)– more common causative agent of tinea nigra. Stenella araguata Cladophialophora saturnica Hand with Tinea nigra Diagnosis • The typical rash of tinea nigra may be sufficient to make a diagnosis. Additional investigations will assist in confirming the diagnosis and this includes : Clinical Material: Skin scrapings. Direct Microscopy: Skin scrapings should be examined using 10% KOH and Parker ink or calcofluor white mounts. Result 10% KOH showing pigmented brown to dark olivaceous (dematiaceous) septate hyphal elements and yeast cells KOH smear showing irregular, branching, septate dematiaceous hyphae Culture: Clinical specimens should be inoculated onto primary isolation media, like Sabouraud's dextrose agar. Colonial morphology: Exophiala werneckii grow slowly and mature within 21 days. From the front they are initially pale in color, moist, shiny, and yeast-like. In time these colonies become velvety, olive black, and are covered with a thin layer of mycelium. From the reverse, the color is black. Microscopical exam by lactophenol cotton blue: Septate hyphae, yeast-like conidia, and chlamydospores are observed. The yeast-like conidia are the initial structures observed in the early phase of the colony development. Septate, thick-walled, and brown hyphae are formed as the colony ages Serology: Not required for diagnosis. lactophenol stain is characterized by septated hyphae, blastospore and arthrospore-typical of the Phaeoannellomyces werneckii fungus Black piedra Piedra, meaning stone in Spanish, is an asymptomatic superficial fungal infection of the hair shaft, resulting in the formation of nodules of different hardness on the infected hair. Caused by the fungus piedraia hortae, which is more common in tropical countries. The source of infection is unknown and person-toperson transmission has been suggested, but this is not clear. Both sexes and people of all ages are equally affected. Clinical manifestations: Infections are usually localized to the scalp but may also be seen on hairs of the beard, moustache and pubic hair. Infected hairs generally have a number of hard black nodules on the shaft. The most common complication is hair loss Laboratory diagnosis: specimen: hairs with hard black nodules present on the shaft. Direct Microscopy: Hairs should be examined using 10% KOH or calcofluor white. Look for darkly pigmented nodules that may partially or completely surround the hair shaft. Culture: Hair fragments should be implanted onto primary isolation media, like Sabouraud's dextrose agar. Colonies of Piedra hortae are small, folded, velvety dark, brown-black and take about 2-3 weeks to appear. Microscopy:Septate hyphae, asci, and ascospores are seen Serology: Not required for diagnosis. Hair with Black Piedra White piedra White piedra is a superficial cosmetic fungal infection of the hair shaft. Infected hair develop soft greyish-white nodules along the shaft. soft nodules composed of yeast cells and arthroconidia that encompass hair shafts. Infections are usually localized to the axilla or scalp but may also be seen on facial hairs and sometimes pubic hair. Caused by the fungus Trichosporom beigelii. Laboratory diagnosis: Specimen: hairs with white soft nodules present on the shaft. Direct Microscopy: Hairs should be examined using 10% KOH or calcofluor white mounts. Look for irregular, soft, white or light brown nodules, 1.0-1.5 mm in length, firmly adhering to the hairs. Culture: Hair fragments should be implanted onto primary isolation media, like Sabouraud's dextrose agar. Colonies of Trichosporon beigelii are white or yellowish to deep cream colored, smooth, wrinkled, velvety, dull colonies with a mycelial fringe. Serology: Not required for diagnosis. (A) Culture on agar-Sabouraud showing a creamy, yellowish-white and cerebriform yeast colony. (B) Direct mycological examination showing a clear friable and soft nodule on the hair cuticle (10X), formed by arthro-conidia and blastoconidia (C; 40X) Colony of trichosporom beigelii