Athletic Therapy
advertisement

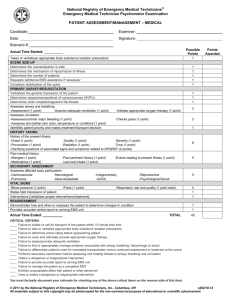
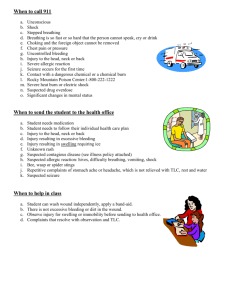
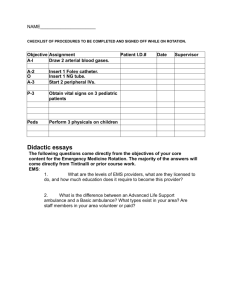
Emergency Plans Lecture 5 Emergency Action Plans Emergency personnel (team) Team physician, therapist, coach , student therapists , local EMS This team will provide 1) immediate care of athlete, 2) equipment retrieval , 3) activation of EMS, 4) directing EMS to scene Emergency communication Plan must be written out , procedure for home and away must be outlined , plan must include location of phones directions to contest site, access points for the facility Emergency equipment Stretches, spine boards, splints etc Emergency Procedures serious injuries may be frightening, particularly when breathing or circulation is impaired as first person on the scene , you must evaluate the situation , assess the extent and seriousness other injury and recognize life threatening conditions , and then provide the immediate emergency care although there are few sport related injuries of this seriousness but they do occur so one must be prepared Reasons to activate EMS Loss of consciousness Suspected cervical injury Unresponsiveness Need to establish an airway Performance of Recue breathing Performance of CPR Major bleeding Any obvious or suspected fracture Emergency Situations conditions or injuries that impair or have the potential to impair breathing and circulation primary / initial survey – determines responsiveness , recognizes and identifies immediate life threatening situations ABC’S secondary survey – involves a more hands on , detailed assessment from head to toe, looking for other non life threatening injuries Responsiveness Before making any decisions about rendering care it is essential that their level of responsiveness be determined. AVPU –Alert and aware V- responds to verbal stimulus P- responds to Painful stimulus U – Unresponsive to any stimulus A Alert and aware – name , location time etc Verbal – do they respond to verbal communication Painful – do they respond to painful stimulus , (pinching the skin , thumbnails etc) response would be facial gestures , movement of limb away from pain Unresponsive – if athlete fails to show any response to above they are said to be unresponsive. Airway Assessment Assess athlete breathing in position found ( look listen and feel) If not breathing try jaw thrust, if that does not work use the head tilt chin lift Remember to check for foreign objects , do not sweep , if you can see it then try to get out . Partial airway obstruction there is still some air exchange and individual will be able to cough will typically grasp the throat ( universal distress sign ) do not interfere stand by and encourage them to continue coughing in attempt to dislodge obstruction an ineffective cough or high pitched noise during breathing should be treated as a total airway obstruction Total Airway Obstruction no air passing through, individual unable to speak , breath or cough must react quickly to clear airway , and stimulate breathing Abdominal thrusts if standing or chest thrusts if lying down Cardiopulmonary Emergencies cardiac arrest, determine if there is a heartbeat… if not begin CPR.. AED’s S/S pain in the chest , radiating to both arms (usually left) into neck , jaw or teeth, upper back or superior middle abdomen shortness of breath , nausea, feeling of impending doom medical emergency activate EMS Unconscious Athlete head injuries leading cause of unconsciousness in sports level of consciousness may very depending on responses of individual to verbal and sensory stimuli unconsciousness identifies an individual who lacks conscious awareness and is unable to respond to stimuli different methods of stimuli – pinching triceps, rubbing knuckles on sternum if unconscious – check ABC’s and call ambulance Bleeding severe bleeding will cause a loss in blood volume and decrease blood pressure this results in increased work load on the heart (rapid weak pulse) arterial bleeding – bright red , usually spurting venous bleeding – dark blueish – red – steady flow best controlled with direct pressure over the wound elevate above the heart Internal bleeding usually the result of a blunt trauma, can lead to shock if overlooked s/s – abdominal rigidity, Nausea, discomfort emergency situation activate EMS Fractures is a break in the continuity of the bone and is classified as open or closed, depending on if the skin is broken or not. obviously open fractures are worse because the risk of infection swelling , bruising , deformities, shortening of limb, guarding , point tenderness , grating or crepitus Ice and Immobilize , minor refer to physician for x-rays , displace or more severe fractures activate EMS Splinting & Immobilization suspected #’s need to be splinted before a person is moved most organized sports settings should be prepared with commercial splints, but outdoor pursuits rarely bring splinting material --> make shift splints have to work Shock shock can occur with any injury, serious or non serious shock is an acute life threatening condition that involves the body’s failure to maintain adequate circulation to the vital organs ( hypovolemic) rapid weak pulse, breathing rapid and shallow anxiety, disorientation , cold clammy moist skin, profuse sweating and extreme thirst Activate EMS Shock Treatment of Shock control any major bleeding and splint fractures if no head or neck injury is suspected – elevate feet 8 to 12 inches if individual vomits – place on side to avoid blocking the airway maintain body heat –remove wet clothing if possible – cover with blanket do not give individual anything by mouth monitor vital signs Activate EAP Shock Anaphylactic shock A sever reaction to a stimulus (allergen) such as a bee sting , medication or food Must activate EMS immediately Anaphylactic shock Secondary Survey Obtain an accurate history SAMPLE S- signs and symptoms A- Allergies M – medications P- pertinent past history L – Last meal ( food & water) E – events leading up to the injury Secondary survey Visually inspect Pupils ( PEARL) Mouth , nose , neck Palpate body from Head to Toe ( look for bruising , swelling deformities)