Definition,Etiology & Risk factors,Pathogenesis,Investigations
advertisement
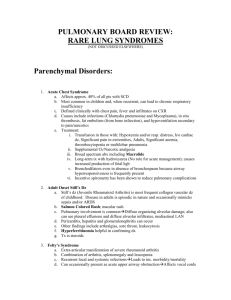
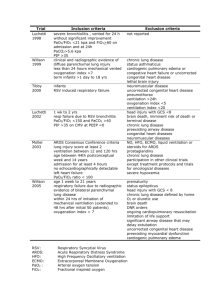
This lecture was conducted during the Nephrology Unit Grand Ground by Medical Student under Nephrology Division under the supervision and administration of Prof. Jamal Al Wakeel, Head of Nephrology Unit, Department of Medicine and Dr. Abdulkareem Al Suwaida, Chairman of Department of Medicine and Nephrology Consultant. Nephrology Division is not responsible for the content of the presentation for it is intended for learning and /or education purpose only. Presented By: Abdulrahman Al Aseem Medical Student Definition It is a clinical syndrom characterized by sever respiratory distress, hypoxemia, noncardiogenic pulmonary edema. Severe, acute lung injury involving diffuse alveolar damage, increased microvascular permeability and non cardiogenic pulmonary edema with acute refractory hypoxemia. mortality- 30-40% American European consesnsu conference (1994) criteria for ARDS: Acute onset of respiratory distress. 2. CXR: New bilateral, diffuse infiltrates. 3. PCWP <18 if measured or no clinical effidence of increased left atrial pressure. 4. Refractory hypoxemia based on PaO2/FiO2 (arterial oxygen tension/fractional inspiratory oxygen)ratio: 1. -ARDS: PaO2/FiO2 < 200mmHg -ALI : PaO2/FiO2 < 300mmHg Etiology & Risk factors May result from direct or indirect (secondary) lung injury Indirect causes: a) sepsis/ septic shock b) severe trauma, burns, pancreatits w/ shock hypoperfusion c) drug over dose d) cardiopulmonary bypass e) acute pancreatitis f) transfusion of multp blood products g) fat or amniotic fluid embolism Etiology & Risk factors Direct causes: a) pneumonia b) aspiration of gastric contents or other causes of chemical pneumonitis c) pulmonary contusion, penetrating lung injury d) fat emboli e) near drowning f) inhalation injury Pathogenesis Activation of inflammatory mediators and cellular components resulting in damage to capillary endothelial and alveolar epithelial cells Increased permeability of alveolar capillary membrane Influx of protein rich edema fluid and inflammatory cells into air spaces Dysfunction of surfactant How the patient present?? Unexplained tachypnea ( the 1st sign often). Breathlessn Increasing hypoxaemia with central cynosis. Bilateral fine Inspiratory crackles thoughout lung field. CXR: bilateral diffuse shadowing diffuse, interstitial at first but subsequently alveolar pattern and air bronchogram. May progress to a picture of complete “white-out”. DDx?? Investigations: Blood: CBC, U&E, amylase, clotting , CRP, Blood culturs. ABG CXR Pulmonary artery catheter to measure PCWP(Pulmanary capillary wedge pressure Management: Admit to ICU Give supportive therapy (respiratory support, circulatory support, nutritional support) Treat the underlying cause (e.g sepsis ) Avoid complications (such as ventilator – associated pneomonia) Respiratory support In early ARDS, CPAP with 40-60% O2 may be adequate to maintain oxygenation. However, most pts need mechanical ventilation Indications for ventilation: PaO2<8.3kPa despite 60% O2 A low- tidal –volume, pressure limited approach, with either loe or moderate high PEEP improves the outcomes. Circulatory support Invasive haemodynamic monitring Conservative fluide management approach improves outcomes Inotrops (eg. Dobutamine ) to maintaine CO and O2 delivery Nitric Oxide Thank you