Cardiac Disorders and Management Outline
advertisement

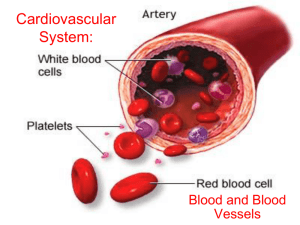
Cardiac Disorders and Management Coronary Vascular Disorders o CAD o Angina o Myocardial Infarction (MI) o Acute Coronary Syndrome (ACS)-describe an array of clinical presentations of CAD that ranges from unstable angina to acute MI Coronary Artery Disease (CAD) o Cardiovascular (CV) disease is the leading cause of death in the US o CAD is most prevalent type of CV disease in adults o Coronary atherosclerosis is most common cause of CV o What’s the Problem With CAD? Narrowing of the arterial lumen Thrombus formation Obstruction of blood flow to myocardium AHA CAD progression o Risk factors High lipids Smoking HTN DM Obesity Family history Inactive lifestyle Age Gender/race Which ones are modifiable? What can be done to prevent CAD? o What problems can CAD lead to? Ischemia Angina MI o How is CAD diagnoses? Health history Physical exam ECG Stress testing Angiography Angina Pectoris o info Chest pain caused by myocardial ischemia Can occur anywhere in chest, neck, arms, or back Most common is behind sternum Lack of Oxygen in Tissue=Pain (in ANY tissue) o Types of Angina Pectoris Stable angina Unstable angina Intractable or refractory Variant Angina (AKA Prinzmetal’s) Silent Ischemia o What is the problem? oxygen demand > oxygen supply Myocardium uses a large amount of oxygen from coronary circulation. Obstruction of a major coronary artery (commonly from atherosclerosis) causes ischemia and results in episodes of pain or pressure in the chest. o Medical Management Objective: to decrease oxygen demand of the myocardium and to increase O2 supply Pharmacological therapy Nitrates, ASA, BB, CCB, antiplatelets, O2 Reperfusion procedures Percutaneous transluminal coronary angioplasty Intracoronary stents CABG Nitroglycerin Vasodilator used to ↓ myocardial O2 consumption→decreased ischemia→pain Sublingual, tablet, or spray, oral capsule, topical agent of IV SL placed under tongue or in buccal pouch May be taken 3x in 5-minute intervals for unrelieved CP Patient Teaching on Nitroglycerin Moisten mouth before taking Carry with them at all times Keep in original (dark) bottle-very unstable Renew supply every 6 months Take note of how long it takes for nitro to relieve pain Anticipated side effects: headache, hypotension, tachycardia and flushing Sit down when taking o Nursing Management PQRST to gather information about CP Reduce anxiety Prevent/reduce pain (stop all activity, semi-Fowler’s position) Patient and family education o PQRST Assessment of CP P: position/location (where? And provocation (what makes it worse?) Q: quality (describe the pain) R: radiate? Relief? S: severity (pain scale); other symptoms T: timing (when did it start?) Myocardial Infarction (MI) o info Sustained ischemia → injury → death of heart muscle cells Immediate recognition of signals is crucial Time is muscle CPR is essential! Basics! ABCD o Signs and Symptoms Sudden and continued CP despite rest and medication Shortness of breath Diaphoresis Indigestion Nausea Anxiety o o o o o o o o Cool, pale, clammy skin Assessment and Diagnostic findings Diagnosis usually made based on S/S, ECG, and lab tests Goal: ECG within 10 minutes of reported CP or arrival to ED Review of cardiac labs Troponin: elevates in 3-4 hrs, peak 4-24, stay up for 1-3 weeks CK-MB: predominately cardiac specific, first enzyme to increase, elevated short time Myoglobin: not very cardiac specific, increases 1-3 hrs after MI, peaks 4-12 hrs, normal within 24 hrs. Diagnosis? Unstable angina: symptoms of ischemia without evidence of acute MI on ECG or cardiac labs ST-segment elevation MI (STEMI): ECG changes in two leads; indicates significant damage to myocardium Non-ST elevation MI (NSTEMI): elevated cardiac markers without definitive ECG evidence Medical Management for MI Goal: minimize myocardial damage, preserve myocardial function, and prevent complications Thrombolytics (stretokinase, tPA) within 3 hours of symptoms Inotropic support (dobutamine)- ↓ SVR Preload/afterload reduction to decrease O2 demand, diuretics, vasodilators (nitro) Emergent PCI CABG Pharmacological Management of MI’s Thrombolytics (stretokinase, tPA) within 3 hours of symptoms Inotropic support (dobutamine)- ↓ SVR Preload/afterload reduction to decrease O2 demand, diuretics, vasodilators (nitro) Anticoagulants Early Treatment of MI’s Aspirin Nitro VS 12-lead ECG Morphine for pain Oxygen Beta Blocker (metoprolol) MONA M-morphine O-oxygen N-nitroglycerine A-aspirin (have them chew it so it gets into their system faster) Cardiac Rehabilitation Active program started once symptoms are resolved Reduces risk through education and physical activity Goal: to extend life and improve quality of life Nursing Process Assessment: important to assess baseline symptoms and identify changes in these Nursing Diagnoses: Ineffective cardiac perfusion Risk for imbalanced fluid volume Risk for ineffective peripheral tissue perfusion Collaborative problems/potential complications Acute pulmonary edema Acute pulmonary edema Heart failure Cardiogenic shock Dysrhythmia’s and cardiac arrest Pericardial effusion and cardiac tamponade Cardiogenic Shock o Info ↓ CO → inadequate tissue perfusion and initiation of shock syndrome May occur after MI (due to areas of ischemia and necrosis) Also can occur with end-stage HF, cardiac tamponade, PE, cardiomyopathy, and dysrhythmia Life-threatening/high mortality rate o Who is at risk? Elderly (>65 yrs) Females Diabetics Pre-existing CAD Anterior wall MI o Signs and symptoms Cerebral hypoxia (restlessness, confusion, agitation), decreased BP, rapid & weak pulse, cold clammy skin, tachypnea o Assessment findings ↓CO , ↓SV, ↑ SVR , ↓BP, ↓ tissue perfusion o Management/Treatment Medications: diuretics, vasodilators, vasopressors Circulatory assist devices (IABP) Hemodynamic monitoring Intra-aortic Balloon Pump (IABP) o Primary goal: decrease workload and maintain adequate perfusion o A catheter with an inflatable balloon at the tip is inserted through the femoral artery and the balloon is placed in the descending thoracic aorta. o Balloon inflates during diastole and aortic valve closure to augment the pumping action of the heart and decrease afterload o Inflation and deflation synchronized to ECG o Indications: cardiogenic shock, LV failure, post-op open heart, unstable angine, post MI o Contraindications: aortic valve incompetence, Peripheral vascular occlusive disease, aorto-femoral/ or illiac bypass grafts, aortic aneurysm o Complications: ↓circulation to leg, left arm or balloon rupture o Wean by decreasing ratio 1:1, 2:1, 4:1 Cardiac Arrest o Info Heart ceases to produce an effective pulse and circulate blood Most reliable sign of this is by absence of a pulse… check carotids Loss of consciousness, pulse and BP ineffective or absent breathing. o Emergency management ABCD Maintain open airway Provide artificial ventilation Promote artificial circulation Defibrillate (*defibrillate for pulseless Vtach and Vfib) Invasive Coronary Artery Procedures o Percutanous Coronary Interventions (PCI’s) Variety of procedures used to treat diseases of the arteries of the heart Previously known as angioplasty, PTCA, and balloon angioplasty Balloon-tipped catheter threaded from groin artery to blocked/diseased area of the heart. When inflated it widens the narrowed artery →increased blood flow. o Randoms Anti-clotting meds are used before, during, and after PCI Plavix, Lovenox Time is muscle Goal: restore blood flow to heart muscle within 90 minutes of arrival in ED “door to balloon time of 90 minutes” o Complications Bleeding, swelling at insertion site, CP o Post-procedure care Assess for back pain (retroperitoneal bleeding) Check pulses (15 min x 2 hrs, then Q1-2 hrs) HOB <30 degrees while sheath in place Leg straight for several hours Direct pressure for 15-30 minutes after removal of sheath o Stent Placement mesh wire tubes inserted during PCI to keep vessel open “permanent scaffolding” o Cardiac Catheterization Guidewire, then sheath, threaded into artery or chamber of heart Opaque dye injected; fluoroscopy Helps determine whether an intervention is needed http://upload.wikimedia.org/wikipedia/commons/6/63/Hk_lv_big_bionerd.gif Coronary Artery Bypass Surgery o info Surgical revasculization (of areas that have been blocked off) Can be used when several arteries have significant blockage Blood vessel grafted distal to coronary artery lesion, bypassing the area of obstruction Saphenous vein or LIMA (left internal mammary artery) vessels most commonly used Off-pump vs on-pump o Immediate Post-Op Period Recovered in critical care unit or PACU Very critical period of time Focus: achieving hemodynamic stability Issues: managing pain, cardiopulmonary status, wound care Assessment for complications ↓ CO, fluid volume and electrolyte imbalances, impaired gas exchange, impaired cerebral circulation Structural Disorders Mitral Valve Prolapse o Info Leaflets papillary muscle of mitral valve do not work correctly leading to prolapse of leaflets, allowing them to go back into the atrium Regurgitation? Cause is unknown Most common form of vavular heart disease o 2x women over men S/S Often patient is asymptomatic Palpitations Dyspnea CP Activity intolerance Mitral Regurgitation o Patho Caused by defect in mitral valve allowing blood to flow back from LV to LA during systole Acute: o causes: rupture of papillary muscle following an acute MI and rupture or one or more chordae teninae o Forceful jet of blood sent retrograde into lt. atrium →sudden increase atrial pressure→acute pulmonary edema, ↓CO and possibly cardiogenic shock Chronic o Elderly most common as structures sag and stretch over time Mitral Stenosis o Obstruction of blood flow from LA to LV due to narrowing of mitral valve orifice o Low-pitched murmur o Occurs during diastole o Best heard in mitral area o Can lead to a-fib and atrial thrombi o ↑ left atrial pressure creates pulmonary congestion, breathlessness, moist cough, and rt. sided heart failure Aortic Regurgitation o Aka aortic insufficiency o Incompetent aortic valve “leaking valve” o High-pitched blowing murmur o Early diastolic o Heard best at aortic area Aortic Stenosis o Narrowing of aortic valve orifice o LV has ↑ difficult ejecting blood into aorta → increased intraventricular pressure→LV hypertrophy (↑ muscle mass)→loss of contractile force in LV o Leads to ↓ decreased blood flow to aorta means less efficient filling of coronary arteries→Chest Pain o Two yrs of symptoms→Survival rate of <50% without valve replacement o Low-pitched, systolic murmur, heard in aortic area Treatment of Valvular Disorders Valvuloplasty-repair of the valve o Commissurotomy o Annuloplasty o Leaflet repair Valve replacemento Mechanical valves o Biologic valves Xenografts Homografts Autografts Infectious Diseases of the Heart o Any of 3 layers can be affected by infections o Named by layer of heart most involved o Rheumatic Endocarditis (endocardium) o Infective Endocarditis o Myocarditis (myocardium) o Pericarditis (pericardium) Infective Endocarditis o info An infectious process which leads to vegetation in heart, usually the leaflets or endocardium Usually caused by strep or staph Portals of entry: dental procedures, tonsillectomy, burns, rheumatic heart disease, IV drug abuse, prosthetic valves Prevention: oral antibiotics for dental procedures o Signs and Symptoms Systemic signs: mild fever, malaise, murmur, chills, abd. pain, dypsnea Petechiae Osler nodes: small, red, raised nodules on fingers or toes Janeway lesions: hemorrhages, flat, red, nontender macules on palms and soles Clubbing Anemia, ↑ WBC’s, + blood cultures Infective Endocarditis cont’d o Treatment: antibiotics, may need valve replacement o Complications: HF, myocardial abscess (from staph), pericarditis, myocarditis, emboli Myocarditis o Causes: infectious agent invading myocardium o S/S: may be asymptomatic or have s/s of HF, ST-T changes, fatigue, dypsnea, temp, CP o Treatment: tx for dysrhythmia’s and HF, O2, steroids, interferon Pericarditis o Causes: MI, viruses, bacteria,trauma, lupus, post-open heart o S/S: Positional CP (worse when lying down, improved when sitting up/leaning forward), friction rub (heard best at lower sternal border) o Complications: pericardial effusion, pericardial tamponade o Treatment: NSAIDS, steroids Pericardial Effusion & Cardiac Tamponade o Pericardial sac normally contains <50 mL of fluid needed to decrease friction of beating heart o Increase in the fluid raises pressure within the sac and compress the heart o Cardinal signs: falling SBP, narrowing pulse pressure, rising venous pressure (inc. JVD) and distant (muffled) heart sounds Cardiomyopathy o Info Disease of the heart muscle associated with cardiac dysfunction Different classifications according to the structural and functional abnormalities of the heart muscle o Patho: decreased stroke volume→ sympathetic nervous system stimulation and the renin-angiotensin-aldosterone resonse→ ↑SVR and ↑ Na and fluid retention →workload on the heart o Known Causes Cardiotoxic agents: alcohol, cocaine, Adriamycin Aortic stenosis HTN Ischemia Can occur acutely or over time. o Types Dilated cardiomyopathy (DCM) Info o o o o Most common type (~90%) Significant dilation of ventricles without simultaneous hypertrophy (increased muscle wall thickness) and systolic dysfunction Diminished ability of the heart to contract ↑ stystolic and diastolic volumes and ↓ ejection fraction S/S o Tachycardia o Fatigue o S3, S4 heart sounds o Murmurs o S/S HF o Echo-easy observation of structure and function of ventricles o ECG may show dysrhythmia’s o Cardiac catheterization may be used to r/o CAD for the cause of the symptoms Management o Treating underlying causes o Treatment similar to that for HF Enhance contractility of heart Decrease afterload Hypertrophic Cardiomyopathy (HCM) Restrictive Cardiomyopathy Arrhythmogenic RV Cardiomyopathy Unclassified Cardiomyopathies Heart Failure (HF) Info o Previously referred to as Congestive Heart Failure (CHF) o HF is a clinical syndrome with s/s of fluid overload or inadequate tissue perfusion o Problem is with either contraction (systolic dysfunction) or filling (diastolic dysfunction) o Number of patients with HF is increasing in the U.S. Over 5 million in US have HF, 550,000 new cases each year; 300,000 die each year from HF o Heart failure is a response to cardiac dysfunction o Any condition which impedes the ability of the heart to pump blood at a volume required to meet the body’s needs can lead to HF CAD→necrotic damage to LV, Valvular dysfunction, Cardiomyopathy, Infection (myocarditis or endocarditis) Types o Systolic (more common) is characterized by a weakened heart muscle o Diastolic is characterized by a stiff and non-compliant heart muscle, making ventricular filling difficult o Ejection fraction is used to help determine the type of dysfunction nl=55%-65% EF is severely ↓ in systolic HF and nl in diastolic Signs of Left vs. Right Heart Failure LEFT RIGHT tachypnea Peripheral edema Tachycardia Hepatomegaly cough Splenomegaly Bibasilar crackles Hepatojugular reflex S3 and S4 Ascites Increase PA pressures JVD Hemoptysis Increased CVP Cyanosis Pulmonary HTN Pulmonary Edema Symptoms of Left vs. Right HF RIGHT Weakness Anorexia Indigestion Weight gain Mental Changes CHRONIC ongoing hypervolemic Na and H2O retention Structural changes in chambers of the heart Acute vs. Chronic HF LEFT fatigue dyspnea orthopnea Paroxysmal nocturnal dyspnea Nocturia ACUTE Rapid onset Pulmonary Edema Low CO Cardiogenic shock Chronic Heart Failure o Info Diagnosis usually made with echocardiogram (ultrasound) Ejection fraction (EJ) is determined through echo CXR is also helpful BNP is key diagnostic indicator of HF Exercise testing or cardiac catheterization can be used to determine whether CAD or cardiac ischemia is the cause o Medical Management Pharmacological therapy ACE inhibitors BB Diuretics Digitalis Nutritional therapy Additional therapy O2 ICD o Nursing Management Careful assessment and monitoring Fluid balance, I/O’s Daily weight Monitoring JVD, VS Monitor for complications r/t diuretic therapy Hypokalemia, hyponatremia, hyperuricemmia o Nursing Diagnosis Activity intolerance Excess fluid volume Powerlessness Acute Heart Failure (Pulmonary Edema) o Info Acute event related to HF May occur with MI Exacerbation of chronic HF o o o Clinical manifestations Pulmonary edema: abnormal accumulation of fluid in the lungs Rapid onset Patient becomes restless and listless Sense of suffocation Cold hands, cyanotic nail beds, ashen skin Weak, rapid pulse JVD Productive cough Medical Management O2 therapy Morphine Diuretics IV medications Dobutamine Nesiritide milrinone Nursing management Position patient to promote circulation and reduce venous return to the heart (upright and feet dangling) Provide emotional support Monitor effects of medications