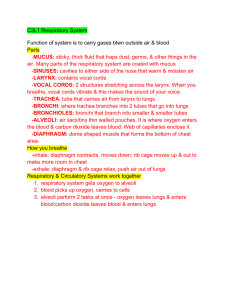
Respiratory System
advertisement

Respiratory System Fun Facts The right lung is slightly larger than the left. Hairs in the nose help to clean the air we breathe as well as warming it. The highest recorded "sneeze speed" is 165 km per hour. The surface area of the lungs is roughly the same size as a tennis court. The capillaries in the lungs would extend 1,600 kilometers if placed end to end. We lose half a liter of water a day through breathing. This is the water vapor we see when we breathe onto glass. A person at rest usually breathes between 12 and 15 times a minute. Every minute we breathe, we take in 13 pints of air! That is we breathe about 6.15 liters of air every minute. The breathing rate is faster in children and women than in men. Respiratory System Chapter 13 Anatomy of the Respiratory System A. Conduction System 1. Functions: a) Direct the air- send air to air sacs (alveoli) b) Humidify the air – add H2O vapor to the air (becomes damp) c) Purify the air – Mucus filter the air of irritants and pathogens. Cilia push mucus to the back of the throat where it is swallowed and digested. d) Warm the air – Network of veins in back of nasal cavity to bring closer to body temperature Anatomy of the Respiratory System 2. Anatomical structures of conduction pathway(in order) a) Nose with nostrils – openings through which air enters body. b) Nasal cavity - Olfactory epithelium located on the top of the cavity and other mucus and veins present to clean and warm the air. Conchae located here, there are three lobes (increase surface area) for more effective purification. c) Paranasal sinuses – openings in the skull bones that lighten the skull and provide resonance chambers for voice. Also production site of mucus that drains into nasal cavity. Anatomy of the Respiratory System d. Pharynx – (5 inches) common passage for digestive (food) and respiratory (air) system. e. Epiglottis – forms the opening to the larynx. Will close when you swallow so food does not go down into the respiratory passages. d. e. Larynx – “voice box”, formed by elastic cartilage. Location of vocal folds (vocal cords) that vibrate with expelled air forming the sounds we make when we speak. Glottis is the slit between the vocal cords. Trachea – windpipe (4 inches – down to T5). Lined with ciliated mucosa to clean, mucus is swept up to pharynx where it is swallowed or spat out. The cilia are destroyed by cigarette smoke and other pollutants. Tracheotomy Trauma to the neck area Obstructing tumors in the upper airway Respiratory failure requiring long-term mechanical breathing assistance, as in these cases: Spinal cord injury in the neck area Severe lung infection or inflammation Injury to the respiratory tract due to breathing in smoke or steam or inhaling corrosive substances Birth defects of the trachea or larynx Foreign object blocking the trachea or larynx Anatomy of the Respiratory System h. i. Primary bronchii – Formed when trachea divide, one branch goes to each lung. Bronchii subdivides within the lung, routing the air directly to the air sacs (alveloli). Lungs – House the bronchial trees (further branching). There are 3 lobes in the right lung and 2 lobes in the left lung. Apex is just deep to your clavicle and the base is by the diaphragm. The pleural membranes that surround are important for decreasing friction. Flashcard Warm-up May 16th The Respiratory Conduction System Trace the pathway of air through the conduction system until it reaches the alveoli of the lungs • Your notes have these structures in order Anatomy of the Respiratory System B. Respiratory Zone 1. Function - area of gas exchange (oxygen in and carbon dioxide out) 2. Structures a) Respiratory bronchioles – final branches of bronchi where the alveoli (air sacs) are found. Alveoli – air sacs, make up most of the lung tissue. Composed of a single cell layer (simple squamous). Sacs are connected with alveolar pores provide alternate routes when some respiratory bronchioles are blocked. Sacs are completely surrounded with capillaries (cobweb), membranes fuse forming the air-blood barrier. Oxygen (into the blood) and carbon dioxide (into alveoli sacs) move across this membrane by simple diffusion (movement from high to low concentrations). Anatomy of the Respiratory System c. Surfactant producing cell – produce a lipid molecule that coats the inside of the alveoli. Helps the sac remain “inflated” by decreasing the surface tension of water. BIG IDEA “Volume changes lead to pressure changes, which lead to the flow of gases to equalize “ Boyle's Law: Relationship Between Pressure and Volume . • These demonstrations illustrate Boyle's of its container. Thus, if you increase the volume of a container, the pressure will decrease, and if you decrease thevolume of a container, the pressure will increase. . Law, which states that the pressure of a gas is inversely proportional to the volume Intercostal muscles Internal pull rib cage in External pull rib cage up and out Respiratory Physiology A. Pulmonary Ventilation (breathing) – air moving in and out of the lungs 1. Requires volume changes in the chest cavity, which alters pressure of the gases in the lungs helping to move the air out and in. a. Inspiration – diaphragm (moves inferiorly and flattens out) and external intercostals contract this increases the intrapulmonary volume (lung size increases as chest cavity moves out) this causes a decrease in pressure inside (like a little vacuum) and sucks air into the lungs. This will continue till the intrapulmonary pressure equals atmospheric pressure. Respiratory Physiology b. Expiration – Primarily a passive process as the diaphragm and external intercostals relax (return to normal resting length) the intrapulmonary volume decreases (causing an increase in pressure – like deflating a float) when the pressure is higher than atmospheric pressure air moves out. If there is a narrowing of the passageways (asthma) or blockage with mucus (bronchitis or pneumonia), the internal intercostals are needed to depress the rib cage and abdominals can move against the diaphragm Respiratory Physiology 2. The collapse of the lungs is prevented due to the intrapleural pressure always being negative (never equal to atmospheric pressure). If this were to occur, such as when there is a puncture wound to the chest, the lungs will collapse, atelectasis. Respiratory Physiology 3. Capacity and movement of air in the lungs. a. Tidal volume – amount of air exchanged during normal breathing. b. Spirometer is used to measure the respiratory capacities of a person. Deficiencies in function can be important in determining respiratory diseases and the extent of the damage. For example, emphysema affects expiration (ERV) and the residual volume is higher. Stethescope can also be useful for diagnosing potential problems. Listening for disruptions in bronchial sounds (air rushing through the tubes) and vesicular sounds (air filling alveoli) can indicate problems. FORCEFUL INSPIRATION TV + IRV+ ERV= FORCEFUL EXPIRATION Air that is left in lungs Respiratory Physiology B. External Respiration – exchange of gases between the alveoli and the capillaries. 1. There is always a higher concentration of oxygen in the alveoli and therefore the oxygen diffuses passively into the capillary blood and binds to hemoglobin, turning the dark red blood of the pulmonary circuit to a brighter red color for its return trip to the heart and distribution to the systemic circuit. Respiratory Physiology 2. Carbon dioxide is at a higher concentration in the blood as compared to the alveoli, so this gas also diffuses into the alveoli. Carbon dioxide is transported in the blood plasma as a bicarbonate ion (HCO3-), this helps maintain blood pH, but it is converted to carbonic acid (H2CO3) before it diffuses out. http://video.about.com/asthma/How- Lungs-Function.htm http://www.youtube.com/watch?v=HiT621 PrrO0 Lung Model 1. Answer the “Think” questions on 13A-D. 2. ONE person from your group will get the ten layers to build your model. 3. Color and cut out each layer (make sure you do NOT cut out the star, square and circle (these will act as a way to connect each layer) Tomorrow we will analyze the structure, function and things that can disrupt each layer Respiratory Physiology C. Internal Respiration – exchange of gases between capillaries and body tissues. This is again primarily a passive exchange due to different concentration gradients in the tissue and the blood. Flashcard Warm-up May 17th Describe the pressure and volume changes taking place during INSPIRATION and EXPIRATION Respiratory Physiology D. Control of respiration 1. Neural control a. Respiratory centers in the brain are located in the medulla and the pons. The medulla sets the basic rhythm and the pons smoothes out that rhythm. Normal respiration is about 12-15 breaths per minute. b. Stretch receptors in the bronchioles help prevent over inflation of the lungs and can stimulate the reaction of expiration. c. If these respiratory centers are overcome with drugs (morphine, sleeping pills) or alcohol they will stop and death occurs. Respiratory Physiology 2. Other controls a. Physical factors – exercise can increase rate and depth of breathing, also increased body temperature can increase rate and depth of breathing. b. Volition - conscious control, necessary for swimming, singing, swallowing., but when oxygen gets too low involuntary controls kick in. (controlled in CORTEX of brain) world record for breath holding- 19 mins) Mammalian diving reflex- allows mammals to hold their breath longer when we are in cold water Respiratory Physiology c. Changes in blood pH due to carbon dioxide levels. This level is the most important stimulus for breathing in a healthy person. 1. If CO2 levels decrease, this RAISES the pH (too basic) of the blood leading to hyperventilation (rapid respiratory rate) which expels more carbon dioxide. 2. If CO2 levels are too high, this LOWERS pH (too acid ) hypoventilation (slow, shallow breathing occurs), keeping more CO2 in the blood. Respiratory Physiology 3. Individuals with disorders that result in continuous elevated CO2 levels (emphysema), the low oxygen levels become the primarily respiratory stimulus. This is why these patients are given low levels of oxygen. Respiratory Physiology E. Disruptions in respiratory system 1. System is particularly vulnerable to airborne pathogens and inflammations due to infections. Ex. tonsillitis, rhinitis. 2. Disorders that block or obstruct the pathways are grouped together and called chronic obstructive pulmonary disease (COPD). They typically include a patient history of smoking which leads to increased levels of dyspnea (labored breathing), coughing, frequent infections, hypoxia (lack of oxygen in the tissues), and ultimately respiratory failure. These include: a. Emphysema – Alveoli enlarge to the point where the walls can break through to other alveoli, this creates inflammation and fibrosis of the tissue (decreased air capacity). Lungs are less elastic and airways can collapse, increased difficulty exhaling. Characterized by a barrel chest due to over inflation of the lungs. Due to the air retention in the lungs (problems exhaling) the oxygen exchange is very efficient and initially do not suffer from hypoxia. b. Chronic bronchitis – Increased mucus production to the point where it pools in the lower lungs, there is a decrease in gas exchange and an increase risk of lung infections. Due to the low efficiency of gas exchange these patients are frequently hypoxic. Asthma is a chronic (longterm) lung disease that inflames and narrows the airways. Asthma causes recurring periods of wheezing (a whistling sound when you breathe), chest tightness, shortness of breath, and coughing. The coughing often occurs at night or early in the morning. Layers for Lung model Ribs and vertebrae (posterior) Ribs and sternum (anterior) Mediastinum and diaphragm Lungs (includes the pleural membranes) Bronchi Alveoli Pulmonary arteries Pulmonary veins Heart Layers for Lung model 1. Ribs and vertebrae (posterior) 2. Mediastinum and diaphragm 3. Posterior Lungs (includes the pleural membranes) 4. Bronchi 5. Alveoli 6. Pulmonary arteries 7. Pulmonary veins 8. Heart 9. Anterior lungs 10. Ribs and Sternum Question of the Week What is heartburn and is it bad for me? One in 10 Americans experiences this once a week. Despite its name, heartburn has nothing to do with the heart. Some of the symptoms, however, are similar to those of a heart attack or heart disease. Heartburn is an irritation of the esophagus that is caused by stomach acid. This can create a burning discomfort in the upper abdomen or below the breast bone. Development of Respiratory System A. Infancy and Childhood 1. Lungs are filled with fluid as a fetus and gas exchange in the placenta. 2. Surfactant is produced (lipid molecule) to keep the alveolar sacs expanded (lowers the surface tension of water). This compound is not present in high enough concentrations until 28 to 30 weeks for the infant to breath on its own. Infants are not up to full lung capacity until 2 weeks of age Development of Respiratory System a. Infants born with respiratory distress (IRDS) can be treated with new equipment that maintains proper pressure levels and keeps alveoli expanded. b. SIDS – some cases are believed to be a neural control problem many seems to be linked with heart abnormalities. The following have been linked to a baby's increased risk of SIDS: Sleeping on the stomach Being around cigarette smoke while in the womb or after being born Sleeping in the same bed as their parents (co-sleeping) Soft bedding in the crib Multiple birth babies (being a twin, triplet, etc.) Premature birth Having a brother or sister who had SIDS Mothers who smoke or use illegal drugs Being born to a teen mother Short time period between pregnancies Late or no prenatal care Living in poverty situations Development of Respiratory System 4. Respiratory rate is high ~ 40 to 80 per minute. B. Early childhood and adolescence 1. Respiratory rate will decrease ~ 30 per minute by age 5. 2. Additional alveoli develop and lungs completely mature. If individual begins smoking during this time the alveoli will not develop and the lungs never completely mature. Development of Respiratory System Asthma may develop – chronically inflamed bronchial passages. C. Adulthood and Old age 1. Respiratory rate continues to decrease, the chest cavity can become rigid and the lungs less elastic. Vital capacity decreases to about 1/3 by age 70. 2. Ciliary movements and phagocyte activity decrease which leads to increased risk of infection. 3.