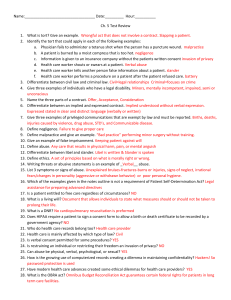
AMA 102 PowerPoint
advertisement

AMA 102 Legal Concepts Sources of Law U.S. Constitution Legislative branch; Congress Judicial branch; U.S. Supreme Court Executive branch; President Statutory Law Created by Congressional and state legislative bodies Published in statutes known as codes Broad scope subject only to constitutional limitations Direct social effect through the political process Administrative Law A type or extension of statutory/legislative law Given power to enact regulations, have force of law Examples: Internal Revenue Service (IRS), Federal Trade Commission (FTC), state medical boards, Medicare, Drug Enforcement Agency (DEA) Common Law Created by judicial branch through decisions in cases decided by courts Diffuse; rules found in fact, patterns, and decisions of prior cases Narrow in scope; limited to actual cases Indirect social effect; judges somewhat insulated from political pressure Civil Law Court actions between private parties, corporations, government bodies, or other organizations Compensation sought usually monetary Recovery of private rights Plaintiff: Party bringing action Defendant: Person accused Criminal Law Court actions brought against individual(s) or groups of people accused of committing a crime Punishment, usually imprisonment and/or fine Recovery of rights of society Crime Defined Felony A serious crime such as murder, assault, rape The punishment is usually severe Misdemeanor Less serious than a felony Disorderly conduct, thefts of small amounts Controlled Substances Act DEA governed, administrative law Regulates addicting medications Greatest potential for abuse, dependence Five schedules from most addicting to least Rules to administer, dispense, or prescribe Registration every 3 years Record keeping Inventory Security Subpoenas An order to appear in court under penalty for failure to do so Subpoena duces tecum Court order requiring a witness to appear and bring certain records or tangible items to a trial or deposition Expert Witness Qualified to testify to professional standard of care; reputable, honest, impartial Essential when subject is beyond understanding of laypersons Testifies what they see, hear, know to be a fact Entitled to a fee Medical Practice Act State statute that defines practice of medicine Describes methods of licensure Sets guidelines for suspension or revocation of license Professional Liability Criminal liability or malfeasance Civil liability or misfeasance Commission of unlawful act Improper performance resulting in injury to another Nonfeasance Failure to perform an act when there is a duty to do so Standard of Care Requires physicians to use the ordinary, reasonable skill, experience, and knowledge commonly used by other reputable physicians when caring for clients HIPAA Passed by Congress in 1996 1. Requires standardized, electronic client data 2. Created unique health identifiers for clients and practitioners 3. Created security standards to protect confidentiality of client data Confidentiality Any communication between client and physician must be kept private Share with other professionals on a “need to know for client’s care” basis Privilege belongs to the client Special consideration for clients with HIV/AIDS Contract Agreement between two or more competent persons upon consideration or payment to do or not to do a task that is legal Expressed Implied Abandonment Physicians are liable if they abandon client Prevention: Formally withdraw from a case Breach of Contract One party fails to satisfy the contract Is cause for litigation Torts Private or civil wrongs Wrongful acts committed against persons that cause harm to the persons Damage to client, proximately caused by conduct of physician that falls below the standard of care Professional Negligence Failure to perform professional duties according to accepted standard of care Performing act reasonable, prudent physician would not perform OR failure to perform act that reasonable, prudent physician would perform Same as malpractice Four Ds of Negligence Duty Derelict Direct Cause Damages Res Ipsa Loquitur A Latin phrase meaning, “The thing speaks for itself” A doctrine of negligence law Respondeat Superior Legal doctrine Literally means, “Let the master answer” Employer is responsible for the actions of his/her employees Risk Management Prevention within the health care setting Prevention with clients Communicable/Notifiable Diseases Concern for public welfare Laws vary among states Health departments publish list Health professionals must report Notifiable/Reportable Injuries Concerns public welfare Gun or knife wounds are examples Child, Elder Abuse, Domestic Violence Child Abuse All states, District of Columbia mandate reporting of child abuse Reporting: Who, what, when Civil liability of reporter Intimate Partner Violence (IPV) Violence between Spouse/former spouse Current or former boyfriend/girlfriend Current or former same sex or heterosexual intimate partners Elder Abuse Intentional or unintentional physical or psychological harm to someone 60 years or older Commonly occurs in the home, nursing home, or other institutions Remember… Vulnerability of survivor to future harm, assault Respect survivor’s right not to report if permissible by law Survivor and abuser need professional care Evidence Carefully document in medical records Documentation must be clear, concise, complete, and in order Chain of evidence cannot be broken Substance Abuse Commonplace in society today Health professionals are especially vulnerable to substance abuse Follow HIPAA and confidentiality guidelines Keep prescription orders secure Have frank, open discussion with clients Good Samaritan Laws Purpose is to encourage health professionals to render first aid to victims without liability for negligence Exist in all 50 states May be poorly defined Do not protect persons who perform outside their scope of practice Consent The affirmation by a client to allow touching, examination, and/or treatment by medically authorized personnel Types of Consent Informed Uninformed Doctrine of Informed Consent Law requiring client to understand nature of illness and be told: What the procedure is and how it is performed Possible risks involved and expected results Any alternative procedures/treatments and risks Results if no treatment is given Problems in Consent Minors Mature minors Emancipated minors Foster children Mentally incompetent clients Language barrier/interpreter Exceptions to Informed Consent Unique to each state Need not disclose risks commonly known if knowledge might be detrimental to clients if client asks to remain ignorant Implementing Consent Consent forms must be: Understandable Protect client’s rights Be broad but specific Signed with expiration date Witness verifies that signature is that of the client Purpose of Medical Records Base for managing client’s care Provide inter/intraoffice communication Document health from birth to death Allows patterns to surface Serve as legal basis for litigation Provide clinical data for education and research POMR & SOAP/SOAPER Problem Oriented Medical Record Subjective Objective Assessment Plan Education Response HIPAA--PHI Protected health information (PHI) in electronic medical records Notice of Privacy Practices (NPP) Restrict usage of PHI Request confidential communication Inspect and obtain copy of PHI Request amendment of PHI Receive an accounting of PHI disclosure Correcting Medical Records Handwritten errors Draw line through error w/red pen Write “corr,” sign initials, date, write in correction Never use whiteout, it is illegal Never alter a medical record, just add corrections or additions Correcting Medical Records Electronic errors Use word processing tracking device to draw line through error Place correction after information lined out Word “correction” or “corr” is indicated Place initials and date correction is made Electronic Medical Records Computer safety and security required Robust firewalls, antivirus installed Password protected, changed regularly Computer limits access to invalid attempts Computer screens out of view Screensaver prevents unwanted viewer’s access Email Automated replies to acknowledge receipt Explain email privacy risks to clients Avoid email that requires urgent reply Email goes in clients records Do not forward without permission Establish regular time to read and respond to email Fax Use only when more secure measures is not appropriate Keep machines in restricted-access, secure areas Verify fax recipient, number, machine location Include statement for receiving fax in error Medical Records Ownership of records Right to privacy of record release Storage of records Retention of records