SOAP Note Rotation 2 (Orthopedic Surgery—Elective) J.D./59M
advertisement

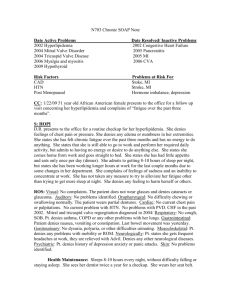
SOAP Note Rotation 2 (Orthopedic Surgery—Elective) J.D./59M Subjective: CC: Swollen hands and wrists x1 week HPI: Pt. is a 59 year old African American male complains of bilateral hand and wrist pain and swelling that has been occurring for approximately one week. The pain is rated at a 3/10. The pain occurred when carrying groceries from the store to his car. The swelling and pain start in the morning and symptoms gradually worsen throughout the day. The pt. has not experienced these symptoms previously. Radiaiton? Aggrevating/alleviating sx’s? Trauma? PMH: Gout, Hepatitis C, Hyperlipidemia, HTN, Asthma FH: HTN, denies family history of heart, respiratory, or endocrine disease. Denies family history of cancer. SH: Denies tobacco, alcohol, and illicit drug use. Currently married and lives at home. Not needed in soap note Allergies: No known food or drug allergies. Meds: Mobic 15mg, Olanzapine 10mg PO daily, Lisinopril 10mg PO qd, Zocor 20mg PO daily, Albuterol 2 puffs prn, Ecotrin prn ROS: General: Skin: Head: Eyes: Ears: Nose: Mouth: Tongue: Teeth: Gums: Throat: Neck: Cardio: Resp.: GI: Denies weakness, fatigue, malaise, fever, chills, sweats. Denies lesions, color changes, pruritus, bruising, excessive dryness, texture, hair, nails. Denies cephalgia, trauma, syncope, lightheadedness Denies changes in vision, pain, diplopia, photophobia, lacrimation, inflammation, injection, discharge, jaundice Denies injury, past disease, decreased hearing, discharge, pain, vertigo, tinnitus. Denies obstruction, headcolds, discharge, epistaxis, anosmia, abnormal odors, sneezing. Denies excessive salvation, dryness, pain, bleeding Denies enlargement, soreness, coating, loss of sense of taste, injury Denies change in condition, pain, abscess, impaction, dental extraction Denies bleeding, swelling, ulceration, discoloration Denies pain, tonsillitis, abscess, difficulty swallowing, nasal discharge Denies stiffness, pain, welling, pulsations, hoarseness, voice change, aphonia, stridor Denies dyspnea, orthopnea, paroxysmal nocturnal dyspnea, edema, palpitation, irregular heart action, chest pain,edema, coldness of extremities, claudication, night cramps, ulceration of extremities, gangrene, color changes in extremities Denies cough, sputum, hemoptysis, wheezing, SOB, pleural pain, injury Denies appetite, food allergy, nature of diet, selective dyspepsia, dysphagia, beichi heartburn, sour stomach, nausea, vomiting, hematemesis, jaundice, epigastric distress, abnormal pain G/U: Endocrine: M/S: Denies change in voiding volume, dysuria, urgency, frequency, hematuria, pyuria, incontinence, difficulty starting/stopping, appearance of urine Denies excessive hunger or thirst , unusual sensitivity to cold/heat, excessive perspiration, nervousness, fine tremor, striae Bilateral hand and wrist pain. Denies should, hip, knee, ankle, and back pain. Not needed in a soap note Objective: VS: General: Skin: HEENT: Wt 195, Ht 74”, BP 176/96, P 59, R 14 Pt. appears stated age, no acute distress, AO x3. Warm moist with normal turgor, no rashes noted. Normocephalic, atraumatic, no noted deformities, no conjuctival injection or icterus, nasal mucosa coral pink without discharge or polyps. Oral mucosa without dryness, leukoplakia, no ginival or dentition abnormalities Neck: No cervical lymphadenopathy, thyroidmegaly, carotid bruits Lungs: AP/ Lat ratio 2:1, no deformities, no accessory muscle use, resonant percussion throughout, clear to auscultation, no adventitous breath sounds noted. Heart: S2>S1 at base, RRR, PMI palpated at 5th ICS-MCL, No S3, S4, or murmurs noted Lymph: No noted lymphadenopathy in the axillary, inguinal, supraclavicular regions Peri/Vas: No marked decrease in pulses bilaterally or proximal to distal Abdominal: No visible masses, scars, rashes, ascites, striae. Normoactive bowel sound x4 quadrants, tympany on percussion. No noted tenderness or guarding. No palpable masses This is a soap note not an H&P Mus/Skel: Upper and lower extremities maintain full ROM both active and passive. No soft tissue swelling noted. No obvious arthrosis to the IP joint. Negative Tinel’s and Phalen’s test. This confusing as I do not see an detailed note regarding his wrists. Swelling? Eccyhmosis? Strength? Assessment: Dx: DDx: Inflammatory Disease—X-rays completed and showed no bony deformities, rheumatology panel to be completed to determine etiology of symptoms Arthritis—no bony deformities seen on x-ray Gout—history of gout but no crystals seen on x-ray Plan: 1. Rheumatology paneled ordered to rule out RA and SLE. 2. Continue Mobic a. 15 mg one tablet daily b. Serious reactions include GI bleed, GI ulceration, MI, stroke, HTN, CHF, nephrotoxicity, anemia c. Pt is currently prescribed Mobic and reports no adverse reactions 3. Patient educated on control of symptoms and to call the clinic if symptoms worsen. You must delineate the exact symptoms that the patient would know that indicates he is getting worse and needs to be seen. 4. Follow-up scheduled for 3 weeks in clinic to reevaluate labs and symptoms. Matt, -10 points- no signature!!!!!! -5 points incomplete PE -5 points incomplete plan 25/45 JL