Training
advertisement

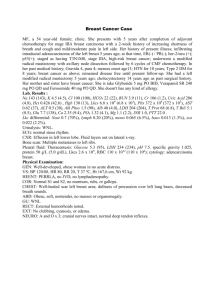
Principles of Cancer Therapy Jeffrey T. Reisert, DO University of New England Physician Assistant Program March 4, 2010 Contact Information Jeffrey T. Reisert, DO Tenney Mountain Internal Medicine 16 Hospital Rd. Plymouth, NH 03264 603-536-6355 603-536-6356 (fax) Jeffrey.T.Reisert@Hitchcock.org Case study You are on the surgical service asked to evaluate a patient with a “GI bleed” 67 y/o male with no prior endoscopies Evaluation reveals a weight loss, heme positive stools. Exam is otherwise unremarkable. Case study questions What lab w/u is needed. What testing is required? – – Lab Other evaluations What next? Outline of Program Surgery Radiation therapy Chemotherapy “Other” treatments for cancer Overview of some specific cancers Palliative care Overview of Treatment Requires tissue diagnosis and staging Risk-Benefit ratio “Kill the cancer before the patient” “A chance to cut is a chance to cure.” Choice of a given therapy is based on type of disease spread Cure vs........ palliation???? Surgery Historically the first treatment available “If cancer is the answer, tissue is the issue!” Use includes diagnosis, staging, definitive treatment Caution to avoid spread/Isolate tumor (i.e.: testicular CA) Surgical techniques Aspiration-Fine needle-i.e.: Thyroid Needle biopsy-Core specimen Incisional biopsy-Remove part of large tumor Excisional biopsy-Remove entire tumor Staging-i.e.: Exploratory lap in Hodgkin’s lymphoma Reconstructive More definitions What do you call a liver biopsy???? Surgery considerations Must take into account margin of resection, lymph node status Cure is more likely in slow growing, local tumors Palliation best for fast growing or metastatic tumors when complications arise – i.e.: Bleeding, Obstruction, Pain May need to integrate with chemotherapy Adjuvant vs....... Neoadjuvant Adjuvant-Treatment to eliminate non detectable micrometastasis Neoadjuvant-Treatment before surgery to increase success – – i.e.: Breast CA Rectal CA Prophylactic surgery Colon-Resection in familial polyposis, ulcerative colitis Breast-Removal if risk for CA >20% in five years??? Orchiectomy-Undescended testicle. Benefit? MEN II-Medullary thyroid cancer Skin-Actinic keratosis or dysplastic nevi Radiation Therapy (RT.)-Goals Local treatment Kill CA without damage to local tissues Allow interval for cellular repair Radiation Therapy-Types X-Rays-Focused beam from linear accelerator Gamma rays-Uses radioactive isotopes – External beam-AKA Teletherapy – Cobalt 60, Cesium 137, Radium 126 i.e.: Head and neck tumor Drink – i.e.: I131-Thyroid cancer Radiation Therapy-Types II Internal, Implantable-AKA Brachytherapy -Origin of word is short -Prostate or gyn tumors Particle beam-Neutrons or protons-Tertiary centers Radiation Therapy-Methods Induces biological damage to cells I.E.: DNA damage due to free radical production – Breaks down DS of DNA May be fatal at first cell division (Mitotic cell death) May be fatal in a few hours (Inducing programmed cell death (Apoptosis)) Radiation Therapy-Treatment RT. kills a percentage of total tumor (not a number of cells) Measured in Gray (Gy)=Amount of energy absorbed 1 Gy=1 Joule of energy per gram of tissue A Rad= 0.01 Gy [1 Gy = 100 RAD) Radiation Therapy-Treatment Planning Can make it very safe Usually fractionated doses to increase safety i.e.: 180-300Gy per day, 5d per week, 5-8 weeks Implantable -“Seeds”- Prostate and GYN CA Radionucleotides – – Iodine 131 (Thyroid CA) Strontium 89 (Palliate bony mets) Radiation-Specific Uses External Beam – – – – – Hodgkin’s Lymphoma, Head and Neck tumors Prostate, GYN, CNS, Skin Breast Palliation-Bony Mets Urgent Use-Spinal cord compression, SVC syndrome Radiation TherapyComplications Kills rapidly dividing cells Systemic-Fatigue – Driving to center/Rigorous schedule Skin-Erythema GI-Mucositis or dry mouth, N/V, Dysphagia, Diarrhea Myelosuppression-All 3 cell lines Cancer risk-Leukemia, Solid Tumors--Especially in Hodgkin’s disease Chemotherapy Overview Major roll is treating metastatic disease Curative or palliative intent Kills percentage of total tumor (Not number of cells) 99% reduction is a 2 log kill (1011 cells--->109 cells) Kill requires adequate dose without toxicity “Narrow therapeutic index” Testing Phase I-Test of safety (Not efficacy) Phase II-Tests activity against tumor – – Typically in patients with advanced disease “Guinea pigs” perhaps Phase III-Compares drugs with other treatments available – Large numbers of pts in multiple centers Chemotherapy-Successes Complete Remission (CR)-All malignancy gone Partial Remission-50+% reduction with no new disease Stable Progression-25% growth in size or new lesions seen Drugs can be ineffective at the start, or acquired – Spontaneous mutations Chemotherapy combinationsPrinciples Each drug should have activity against tumor Different mechanisms of action No cross resistance between agents Different toxicities Chemotherapeutic agents Included for completeness Don’t go crazy memorizing I have left this in but will not test on any specifics. Chemo examples Antimetabolites-Pyrimidine like – MOA: False substrate for biological pathway, incorporated into DNA/RNA--->breaks) – Examples 5 Fluorouracil (5FU)-Breast, colorectal Others: Cytarabine (ara-C), Gemcitabine – ADR:Bone marrow suppression and GI Chemo examples cont. Antimetabolites-Purine like – MOA False – substrate for biological pathway Examples Fludarabine, – 6-Mercaptopurine (6MP) ADR’s Myelosuppression Chemo examples cont. Class: Antimetabolites-Others – Methotrexate (MTX) MOA: Inhibits dihydrofolate reductase preventing purine synthesis – – – Use: ALL, bladder, breast, head/neck, HL) ADR: BM and GI toxicity Hydroxyurea CML, Essential thrombocytosis Chemo examples cont. Plant alkaloids – Examples Vincristine and Vinblastine (Bladder, breast, HL, NHL) – MOA: Prevent disassembly of microtubules-Stops mitosis – ADR’s : Neuropathy Paclitaxel (Taxol®) and Docetaxel (Taxotere®) (Ovarian and breast CA, Non-small cell lung CA) – – MOA: Prevent formation of microtubules-Stops mitosis ADR’s: Neuropathy, Alopecia, Bone marrow suppression Chemo examples cont. Topoisomerase Inhibitors – MOA – Examples – Etoposide (AML, lung, NHL)/Teniposide (ALL, NHL) ADR’s Prevent repair to DNA Defragments the DNA Leukopenia Anthracyclines – MOA – Examples – Produce free radicals--->cytotoxicity Doxorubicin (Adriamycin)-Bladder, Breast, HL, NHL, others Daunorubicin-ALL. AML Doxorubicin liposomal (Doxil®)-Encapsulated doxorubicin-Ovarian CA, sarcomas Mitoxantrone is similar, and less cardiotoxic-AML, Breast, NHL ADR’s Leukemia, Myelosuppression, GI toxicity, vesicants Cardiotoxic at doses of 500-550mg/m2 Chemo examples cont. Alkyalators – MOA – Examples – Breaks DNA strands by adding alkly group Cyclophosphamide (Cystitis)-Bladder, Breast, CML, lung, NHL Ifosfamide (Less myelo, more cytotoxic)-Breast, NHL Melphalan (Leukemia, pulmonary fibrosis)-Breast, multiple myeloma, ovarian Busulfan (Pneumonitis)-CML Nitrosureas such as BCNU and CCNU (Myelosuppression, pulmonary fibrosis)-HL, NHL Platinums such as Cisplatin and carboplatin (Cause DNA cross linking)-Bladder, esophagus, ovarian ADR’s Mutagenic--->Leukemia possible Myelosuppression Emetogenic Nephro and Neurotoxic (Platinums) Chemo examples cont. Antibiotics – MOA Breaks – DNA and generates free radicals Examples Bleomycin (HL, NHL, testicular) Mitomycin C (Breast, colorectal) – ADR’s Pulmonary toxicity if > 200U/m2 (Bleomycin) Targeted therapies Cell surface antibodies – Rituximab (Rituxan®) (anti CD 20) – – – Chimeric (Mouse + Human antibody) Cetuximab (Erbitux®) (anti C 225) Trastuzumab (Herceptin®) (anti Her 2 Neu) Bevacizumab (Avastin®) (anti VEGF) Small molecules – – Gefitinib (Iressa®) (anti EGFR) Imatinib (Gleevac®) (anti bcl oncogene) Chemotherapy There are MANY others Do not try to memorize – – Have listed for completion Understand CONCEPTS List continues to evolve – – New medications New uses/indications Chemotherapy Complications This I will test on (generalities) Myelosuppression-Most Common Dose Limiting Toxicity – Usually seen 10-14 days after dose – Usually recover 21-28 days – Neutropenia---> Fever (Covered later) – Low platelets usually a problem is <20K. Alopecia – Cyclophosphamide, Dactinomycin, Doxorubicin – Paclitaxel, Vincristine Chemotherapy Complications Nausea and vomiting (Emetogenic) – – Some drugs affect vomiting center, chemoreceptor trigger zone Pretreatment helps Chemotherapy Complications-II Nausea treatments – – – Prochlorperazine (Compazine®), Chlorpromazine (Thorazine®) (Anti-dopaminergic) Metoclopramide (Reglan®) (Anti-dopaminergic) Ondansetron (Zofran®), Ganisetron (Kytril®), and Dolasetron (Anzemet®) – – – Selective 5HT receptor antagonists-Block serotonin Dronabinol (Marinol®)-THC Glucocorticoids Benzodiazepines Chemotherapy Complications-III Stomatitis – – Most chemo can cause Topical anesthetics (Lidocaine viscous) Hormonal treatment of cancer-I AdrenocorticosteroidsLeukemia/Lymphoma – May help programmed cell death Antiandrogens – i.e.: Flutamide (Prostate CA) Hormonal treatment of cancer-II Estrogens – – Prostate CA historically Breast palliation (DES, ethinyl estradiol) Antiestrogens – Tamoxifen (Breast CA) Tamoxifen Use in breast CA – – – Treatment Prevention Reduces occurrence and reoccurrence in women with breast cancer or high risk for breast cancer Binds estrogen--->Agonist/antagonist Advantages: Decreased cardiovascular disease and osteoporosis Disadvantages: Menopause, thromboembolism, Endometrial CA Hormonal treatment of cancer-II Progestins – – – Endometrial and breast CA i.e.: Medroxyprogesterone, megestrol acetate Disadvantage: Irregular menses and weight gain (Megace® 800mg per day of suspension used to treat poor appetite/Cancer cachexia) Aromatase inhibitors – – – Aminoglutethimide-Prostate cancer Letrozole (Femara®)-Breast cancer Decrease steroid synthesis Hormonal treatment of cancer-III Gonadotropin-Releasing Hormone agonists – Leuprolide (Lupron®) decreases androgen levels (Prostate CA) Somatostatin analogues – Octreotide (Sandostatin®) (Carcinoid, vasoactive intestinal peptides secreting tumors) Other treatments for Cancer Bone Marrow Transplantation Kill one’s own cells Replace with own cells treated (Autologous) Peripheral stem cell transplant Or, replace with another’s cells (Allogeneic) Best use: Acute leukemia, Hodgkin’s, NonHodgkin’s, Testicular Immunotherapy Monoclonal antibodies – – Were investigational for treatment Now proven IE: – Mouse antibodies… Rituximab) Used in diagnosis (PSA, CA 125) Cytokines-Next slide Immunotherapy-Cytokines Interferon – – Use: CML, Hairy Cell leukemia, Kaposi’s, Melanoma Flu like side effects Interleukins – – Stimulate T cells and Natural Killer cells IL-2 (Renal cell, melanoma) Growth factors (GF) Colony stimulating factors that are IL like Neutrophils – Granulocyte-Macrophage Colony Stimulating factor (G-CSF) Granulocytes, monocytes, eosinophils Filgrastim (Neupogen®), Pegfiltrastim (Neulasta®) Growth factors (GF)-Cont. Red cells – Erythropoietin (Epoetin alfa (Epogen®, Procrit®), Darbepoetin alfa (Aranesp®) Platelets – Thrombopoietin (TPO) Vaccines Usual vaccines should be given, perhaps prior to treatment Adults – – – Tetanus Influenza Pneumococcus (particularly if splenectomy planned) Other treatments-Research Cellular therapy-Grown cells implanted into CA patient Vaccines Other treatments Nutritional Supplements Largely unproven Aspirin may reduce cancer 2010??? Genetic screening Should just mention here…. A budding field Experts are available regionally (bigger centers) Some specific cancers worth mentioning Skin Lung Breast GI – – Others Colorectal Myelodysplasia Lymphoma Leukemia I will not test you on which chemo works for which tumors Skin Cancer Melanoma Non-Melanoma – – Sun exposure major RF – – – 70-80% Basal cell 20% Squamous cell Equator worse Light skin worse Face including ears and nose Less risk in dark skinned individuals Basal cell skin CA (BCC) Arises from the basal cells of skin Slow growing typically Pearly nodule Telangectasias Treatment-next slide BCC Treatment Cut out Electrodessication and curettage Cryosurgery if low risk RT Laser Moh’s – – – – – – Specialized form of dermatology/pathology Anesthesia, remove lesion to edge Frozen section, stain for pathology If residual tumor (edges not free of disease) more surgery After borders clear, done! Allows smaller excision/Better cosmesis BCC prevention/treatment Fluorouracil – – – Treats actinic keratosis Reduces progression to skin cancer 5 fluorouracil (5FU) (Efudex®) Immunomodulators – – Similar indications as flourouracil Imiquimod (Aldara ®) Squamous cell skin CA (SCC) From keratinizing epidermal cells Malignant-Can metastasize Ulcerated erythematous nodule Actinic keratosis precursor – Hyperkeratotic papule Wider excision ? RT Mets: LN resection, RT or both 13-cis-retinoic acid (1mg po qd) + Interferon α (3M units sc or IM qd) Melanoma From neural crest derived melanocytes – May be amelanotic 4 types – Superficial – Superficial spreading Lentigo maligna-chronic sun exposure Acral lentiginous-palms, soles, nails, mucous membranes Deep Nodular-typically heavily pigmented and deep invasion seen at time of dx Melanoma-Prognostication Breslow’s thickness (worse if more than 1mm depth at time of dx) Ulceration Node involvement Satellites Mets Clark’s staging – Ranges from early in situ disease (I) to penetrating fat (V) Melanoma eval and TX Spreads via lymph nodes and blood Biopsy Wide excision – 2-4cm typically LN bx IFN α, dicarbazine (DTIC), nitrosureas like BCNU, cisplatin/carboplatin, vincristine Lung Cancer Tumors derived from respiratory epithelium – 88% are – Small cell (oat cell)-central tumor Squamous-central tumor Adenocarcinoma-peripheral tumor Large cell-peripheral tumor “LA is on the coast” Others include Mesotheliomas Lymphomas Sarcomas Lung cancer-II Really two types based on course Small cell (SCLC) and non-small cell (NSCLC) – – Small cell tends to spread early Non-small cell has option for surgical cure, early in disease Lung cancer III 90% are tobacco users – – – – – Lung cancer is largely a disease of smokers (Peter Jennings) Don’t let media fool you (Christopher Reeves’ wife) Recent data suggests more non-smoking women are getting cancer than non-smoking men Second hand smoke? Radon? Lung CA-Overview Symptoms (about 5 of 6 pts) – – – – – – – Cough Hemoptysis Weight loss Dyspnea Post obstructive pneumonia Chest pain Paraneoplastic syndrome Lung cancer radiography Incidental chest x-ray – – About 1 in 6 lung cancer patients are asymptomatic While often found this way, screening CXR’s in smokers do NOT improve survival in those screened (no reduction in death rates) Chest CT scan – May be better at screening (recent studies), but who will pay? Solitary pulmonary nodule X-Ray density 1-6cm in size 35% are malignant, most being lung CA Can be followed serially in low risk pts – – – Old x-rays Q3mo CT for one year then annual until stable No change in character in 2 years or favorable appearance (i.e.: dense calcium center) suggest benign Biopsy should be considered in higher risk – – Older than 35 Tobacco history Lung CA work up CXR CT Positron emission tomography (PET) Look for paraneoplastic syndromes (later lecture) – – Common in lung malignancies Systemic disease? Lung CA diagnosis Fluid – – – Aspiration of pleural effusion Sputum cytology Bronchoscopy Biopsy – – – Needle (CT guided? Interventional radiologists, chest surgeons) Open lung (thorocotomy) LN Small cell lung CA (SCLC) Two types-That’s it! – Limited stage (30% pts) – – Extensive stage Note early mets to brain 10% pts – – Single sided Regional lymph nodes only “One radiation therapy port” Prophylactic RT does NOT improve survival Also bone marrow mets in 20-30 % pts Bone scan SCLC-Chemo Median survival 6-17 weeks without TX 40-70% respond to chemo – Response predicts increased survival Etopiside + cisplatin/carboplatin Others active include paclitaxel, irinotecan, others Non-small cell lung CA (NSCLC) TNM staging NSCLC Treatment approach 1/3 of pts are candidates for surgery at diagnosis 1/3 are in the middle 1/3 have distant mets NSCLC-Surgery Consider if – – Healthy pt Early stage disease IA, – IIA, IB, IIB Local disease Contraindicated if FEV1 <1L – If over 2.5L may be candidate for pneumonectomy NSCLC-Chemo 20-30% response rate 9-10mo median survival 1 year survival is 40% Paclitaxel + Carboplatin/Cisplatin Vinorelbine + Cisplatin Others active include docetaxel, irinotecan, gemcitabine, Gefitinib (Iressa®) Breast Cancer diagnosis Breast exam – – – – – Axilla (Apex of axilla, slide fingers down across chest wall) Skin (distortion? Edema?) Breast itself (Attention upper outer quadrant….most CA there! Firm, painless, non-mobile mass) Nipple (discharge?) Self breast exam does NOT decrease death rates (large Chinese study c 2001) but is easy and safe Persistent Masses should be biopsied Cystic masses may be aspirated Breast radiography Mammograms – – Ultrasound – – Cystic vs..... solid mass Needle localization CT scan – Begin at 40 and repeat annually Looking for clustered microcalcifications, spiculated densities, architectural distortion No better MRI – – – – New May be better (cost wise) for higher risk patients Under extensive study Not necessarily better Breast cancer miscellany Mutated BRCA-1 tumor suppressor gene – – Mutated p53 tumor suppressor gene – 60% chance of developing breast CA 33% chance of ovarian CA Seen in 40% of cases See blurb on HRT risk of breast CA in handouts Breast Cancer Surgery – – – – – – Needle localization vs..... stereotactic bx? Only 1 in 5 to 1 in 10 who get bx have cancer Breast conserving tx (lumpectomy plus RT) as good as mastectomy LN bx axilla usually done If tumor <1cm surgery may be enough if LN neg If >5cm usually need mastectomy Breast CA-Chemo issues Usually multi-drug regimen are used either for metastatic disease or for adjuvant tx – – – First line doxorubicin + cyclophosphamide CMF (cyclophosphamide + Methotrexate + Fluorouracil or many others Second line Anthracycline or paclitaxel based treatment Hormone treatment Breast Cancer-Hormone treatment Tamoxifen (Nolvodex®) 10-20 mg po qd – – – Agonist/Antagonist to estrogen For 5 years Usually in post-menopausal woman after chemo done Letrozole (Femara®) 2.5 mg po qd – – Now follows tamoxifen for 5+ years May go right to Letrozole without Tamoxifen Breast Cancer-Prognosticators Tumor stage – – Receptor status – Size of mass (Larger obviously worse) LN status (Positive obviously worse) Estrogen Receptor (ER) and Progesterone Receptor (PR) positivity suggest better prognosis Other tumor issues – – – – Slower growing tumor better Histology (poor histological grade, worse) erbB2 (HER-2/neu) gene (worse) Mutant p53 gene (worse) GI Malignancies Esophagus Gastric Colon/Rectal Liver Pancreas There are others that will not be covered here Esophageal cancer Largely a disease of smokers coupled with alcohol overuse Role of GERD prominent A lethal CA – 5% 5 year survival May have dysphagia and wt loss (bad prognosis) Dx: EGD, biopsy Esophageal CA-Treatment About 45% of pts are candidates for surgery RT often precedes (Neo-Adjuvant) Chemo-poor response Palliative care? – Feeding tube Gastric cancer Nitrates (hot dogs, smoked foods) increase risk Helicobacter pylori association Ulcers in stomach found must be followed for resolution – May hide gastric CA Treatment – – – Chemo-5FU + doxorubicin based Surgery RT-not very helpful Colorectal cancer-Associations Hereditary issues – Familial polyposis syndromes Autosomal dom May reduce risks with prostaglandin blockers – – NSAIDS including aspirin, and COX-2 inhibitors such ask celecoxib (Celebrex®) Inflammatory bowel disease – – – After 10 years of diagnosis, 1% increase risk per year 8-30% risk after 25 years of diagnosis >15 years consider prophylactic colectomy Colorectal CA-signs and symptoms Screening – – Stool tests for blood Colonoscopy Blood loss – – Hematochezia (blood in stool) Iron deficiency anemia must be worked up Abdominal pain Obstruction (bad) Colorectal cancer-Prognostication Depth of invasion LN involvement Mets Surgically resectable disease likely to do better Colorectal cancer treatment Resection when possible RT in the case of rectal cancer – Harder to resect disease deep in pelvis Chemo – – – 5FU is single most effective single agent Usually combined with leucovorin Others include Irinotecan (CPT-11) Liver tumors Primary (hepatocellular, hepatoma) or Secondary (metastatic) Primary associated with cirrhosis, viral hepatitis C. – Elevated AFP Metastatic-Must find primary Pancreatic cancer Difficult to diagnose and treat – – 5 year survival only about 10% 98% fatality Cause unknown CA 19-9 excellent tumor marker May present with vague or specific symptoms – – – – Abd pain Jaundice with itching Weight loss Clay colored stools (plugged bile duct, not bile in stool) Pancreatic Ca-Diagnosis CT Abd U/S – Endoscopic ultrasound (EUS) MRI PET scan may help (not that great) Endoscopic retrograde cholangiopanreatography (ERCP) Percutaneous bx or by laparotomy Pancreatic Ca-Treatment Complete excision is only thing that substantially impacts survival – – – Chemo – – Only 10-15% of pts are candidates when found Surgery has 15% mortality rate Pancreaticoduodenectomy (Whipple procedure) 5FU + gemcitabine Others RT? Myelodysplasia Ineffective hematopoesis – – Many classification systems – – – Dyspoeisis-Abnormal functioning marrow Results in cytopenias French American British (FAB) Modified by World Health Organization Table 94-5 Requires bone marrow biopsy – – Standard bone marrow prep ?Philadelphia chromosome (CML and ALL) The first reproducible chromosome abnormality in human malignancy. 9, 22 translocation allows ABL oncogene to be close to BRC (breakpoint cluster region) Gene product leads to independent cell growth Gleevec blocks the response to this (A new form of chemo, now available for CML) Myelodysplasia- Approach to treatment Observation? Support Drugs may help – – – Thalidomide Azacitine (Vidazza®) Others (Dacagoen, ARA-C, Angiogenesis inhibitors such as Avastin® (used for colon CA), other growth factors Transfusion Bone marrow transplant in younger pts (<65) Treat aggressively if conversion to leukemia Lymphoma Hodgkin’s vs...... non-Hodgkin’s – – Reed Sternberg cell (large cell with bilobed nucleus…owl’s eye appearance) is key microscopic feature in Hodgkin’s lymphoma 90% survive Hodgkin’s B symptoms – – – RT responsive Doxorubicin+bleomycin+vinblastine+acarbazine (ABVD) Fever Night sweats Weight loss Often incurable T cell lymphomas have HTLV-1 retrovirus association NH lymphomas Classified broadly into aggressive and indolent Includes low grade small cell lymphomas, mantle cell lymphomas arising from the mantle zone of the follicle, and mucosal associated lymphoma (MALT) associated with H. pylori 6 classification systems exist – Ann Arbor most common LN status Presence of B symptoms NH Lymphoma treatment Aggressive – – Goad of cure Multiple meds (many combos) or BM transplant Most common is CHOP (Cytoxan+adriamycin+vincristine+prednisone) May add Rituxan (Anti CD 20, against a cell surface AB) RT Indolent-next slide NH Lymphoma treatment cont. Indolent – – – – – Slower growing Quality of life (watchful waiting?) Chemo may not alter survival Treat when symptoms, bulky disease Drugs include alkylators, vinca alkaloids, anthracyclines, nucleoside analogues (Fludara), and targeted therapies (Rituxan) Leukemias-4 broad categories Acute Chronic Lymphocytic ALL CLL Myeloid AML CML AML >20% myeloblasts WBC’s elevated – Non-specific s/s – – – Fatigue, weak Pain, fever Enlarged LN’s, or hepatosplenomegaly Progostics – Usually >15K Old, worse Treatment-next slide AML-Treatment Induction chemotherapy – Attempt CR – Cytarabine (cytosine arabinoside)+anthracycline +/- etoposide Increased survival Treat relapses CML Often have chromosome 9, 22 translocation – – – s/s – – – T (9,22) Seen in 90-95% of pts MC is Philadelphia chromosome Usually insidious onset Hepatosplenomegaly Elevated WBC with <5% blasts Treatment – – Cured with allogeneic BM transplant (Family or matched donor with 5-6 MCH Ag match) Imatinide (oral chemo that inhibits ATP binding inducing apoptosis) ALL B cell AL is MC CA in children May have Philadelphia chromosome CLL B cell CLL is MC lymphoid leukemia Prolonged survival likely – Median survival is 10 years Treatment – – – Chlorambucil PO or Fludarabine IV or Both Other cancer topics Palliative care Definition – Giving relief of the symptoms without curative intent Decisions – – Cure or not to cure Must take into account physical, emotional, spiritual needs Palliative Issues Pain Cancer complications – – The “C” word – – Bleeding Obstruction Fear of cancer Stigma of having cancer Fear of dying – DNR orders Hospice Originally in Europe, a place for weary travelers in the Middle Ages Today, the compassionate care given in homes or institutions to the terminally ill “Dying with dignity” Hospice-cont. Effort on the part of many including physicians, nurses, social workers, counselors, volunteers, religious, etc. Helps the dying AND their family Attention to pain control Settings – – – Home Inpatient setting Outpatient setting (hospice houses) Hospice specifics/treatments Pain control (future slide) Nausea – – Prochlorperazine (Compazine®) po or pr, metochlopramide (Reglan®) po or IV Newer agents (Zofran®, others po or IV) Hospice specifics/treatments cont. Constipation – – – – Terminal secretions (“Death rattle”) – – Stool softeners (docusate (Colace®)) Laxatives Non-absorbable sugars (lactulose) Newer agents polyethylene glycol (Miralax®) Atropine injectable or eye drops given po Scopolamine IV, IM, sc, patch Seizures in brain mets Pain medication in palliative care Short-vs-Long acting? Route – – – – – IV IM SC Topical (fentanyl (Duragesic®)) Intrathecal (pump) Constipation may be limiting, particularly if dehydrated (New med for this c 2008 Relistor® (methylnaltrexone bromide)) Communicating Bad News Difficult Requires tact and experience Do you tell the patient? The family? Sugar coat it? Will pt lose hope and perhaps give up? Should you stop usual meds (i.e.: cardiac meds)? Case Evaluation Diagnosis Staging Biopsy Treatment/planning Follow up Summary Treatment of cancer requires understanding of stage of disease Stage and knowledge of best treatment is key Combination of surgery, radiation, and chemotherapy, hormones, supportive care may be used Anticipate complications of treatment When you can’t cure, keep comfortable Cancer is a scary diagnosis, but with team approach, can be treated successfully Where to get more information Harrison’s or Cecil’s DaVida’s textbook of oncology American Cancer Society-Excellent reference, including on line resources